In the current era, many patients present with a small primary breast cancer detected by mammography or other screening procedures. In recent decades, the median size of nodal metastases has decreased, paralleling the decrease in primary tumor size. The median size of nodal metastases is now approximately 6 mm,1 and 70% to 80% of patients have negative nodes after surgical and pathologic nodal staging. A systematic approach to the evaluation of lymph nodes is needed today to reliably identify metastatic carcinoma.
Sentinel lymph node (SLN) biopsy has led to the use of more sensitive pathologic techniques to reliably detect small metastases and reduce the risk of false-negative results. The nature of SLNs as first-draining lymph nodes, combined with the use of multilevel sections and cytokeratin immunohistochemistry, has significantly increased the number of patients with nodal micrometastases or isolated tumor cells2 and intensified the debate over the therapeutic benefit of axillary dissection and the clinical impact of minimal metastases on patient prognosis and choices for adjuvant therapies. Clinicians, including pathologists, need to understand that minimal nodal disease, when present, should be considered in the context of the primary tumor characteristics and the patient’s clinical status. A multidisciplinary breast conference discussion helps to optimize individual patient care recommendations.
SLN biopsy performed by an experienced surgeon provides prognostic and staging information equivalent to that provided by axillary dissection. Validation studies, with comprehensive pathologic analysis of both SLNs and non-SLNs, have confirmed the accuracy and safety of SLN biopsy. 2-4 The accuracy of SLN biopsy compared with complete level I and II axillary dissection is greater than 95% at major centers.5 Axillary recurrence rates for patients with negative SLN biopsy followed by adjuvant therapies appear similar to recurrence rates for patients who have had complete axillary dissection.6
Nonsurgical alternative approaches to axillary staging have recently focused on ultrasound evaluation to determine whether SLN biopsy is indicated.7,8 Patients with a large primary tumor9,10 or suspicious axillary clinical examination may benefit from preoperative axillary ultrasound with fine-needle aspiration cytology or core biopsy of suspicious nodes (Chapter 24). Patients with a positive needle biopsy result can proceed to complete axillary dissection, whereas those with a negative or nondiagnostic result undergo SLN biopsy. Studies with fine-needle aspiration cytology have demonstrated a high level of accuracy for ultrasound-detected macrometastases, with a reduction of SLN procedures by 10% to 15% and resultant cost savings.9 Pathologists should be careful to avoid a false-positive result, which has been reported rarely.
Primary tumor typing with phenotypic and molecular genotypic assays, under investigation today,11 may help in the future to determine which patients benefit from SLN biopsy and complete axillary node dissection (CLND).
Optimal patient care derives from a well-functioning surgeon–pathologist team. Sentinel nodes should be submitted to pathology preferably as single nodes dissected free of adipose tissue and with a description as hot or blue. Individual institutions and physicians need to decide whether intraoperative pathologic examination is a good management approach in their practice setting, and, if so, which methods would be best with the available personnel, facilities, and instruments.
The clinical significance of axillary node micrometastases and isolated tumor cells continues to be debated, because in population-based statistical comparisons, the prognostic impact of nodal micrometastases is relatively small. Recent studies using more thorough lymph node embedding and improved immunohistochemical methods have reported a significant association between micrometastases and poor survival compared with that of node-negative patients.12,13 However, the prognostic significance of nodal micrometastases remains unclear,14 particularly in adjuvant therapy–treated patients. Ongoing clinical trials will further help to define the clinical impact of nodal micrometastases and isolated tumor cells.
The goal for the pathologist in current practice is to minimize the risk of missing macrometastases and micrometastases in SLNs. Because the likelihood of identifying metastases is related to the number and depth of histologic sections, the use of cytokeratin-immunohistochemistry (CK-IHC) stains, and the size of metastases, it is now well accepted that SLNs should be examined more thoroughly than other lymph nodes. The detection of early metastasis helps to reduce the false-negative rate of the SLN staging procedure.15 Nevertheless, it should be recognized that detection of all cases with only isolated tumor cells is an unrealistic goal with the available techniques and resources.
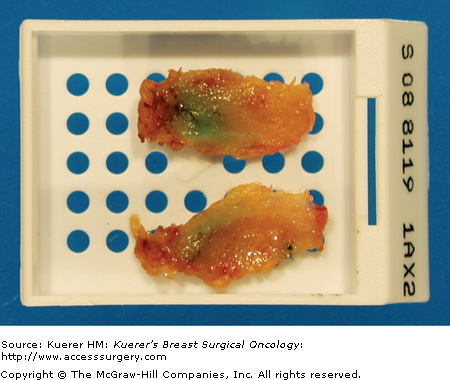
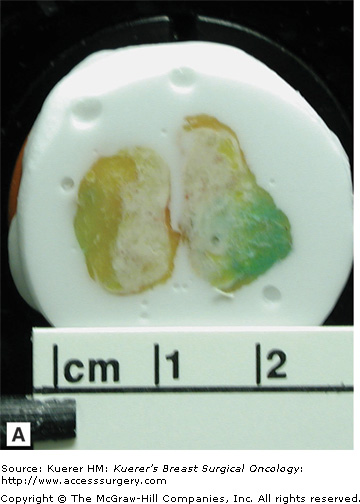
Variations in gross and microscopic sectioning methods for SLNs account, in part, for substantial differences in rates of metastasis detection reported in the literature. Longitudinal sections are recommended,5 since afferent lymphatics generally enter the node in the midline plane of the long axis, and small metastases are most likely to be found near that entry point.16,17 Placement of the central nodal surfaces at the bottom of the cassette will result in the highest yield of metastasis detection in the first histologic levels.18,19 It is also important to cut thin gross sections, no thicker than 2 mm, which is accomplished with simple longitudinal bisection of most SLNs (Figs. 26-1 and 26-2). When gross sections are thick, additional deep histologic levels may be needed for sufficient sampling. Histologic examination of only half of the SLN, as occurs with rapid molecular assays, may cause a histologic false-negative result.20
There is no consensus among pathologists regarding how many hematoxylin and eosin (H&E) and CK-IHC levels should be examined. Conflicting data on this subject may be explained, at least in part, by differences in methods applied to gross sections and the number of cytokeratin levels examined, in addition to the absence of an accepted standard for metastasis detection. The studies that have supported limited (2 to 4) step sections have generally utilized longitudinal gross sections with both CK-IHC and H&E at each microscopic level. Comprehensive examination with CK-IHC has demonstrated that positive lymph nodes nearly always have multiple clusters/deposits and that limited sections are sufficient to detect some of them in nearly all patients with metastasis (Table 26-1).18,19,21-23 Institutions that have applied transverse gross sections or utilized predominantly H&E stains in histologic evaluation have generally concluded that more numerous levels of the paraffin block are needed to identify cases with small metastases.
| Study | Limited Sections | Accuracy Versus Deeper Levels |
|---|---|---|
| Turner et al (1999)18 | Two levels, 40 μm, each with CK-IHC | 98% (41/42) |
| Cserni (2002)19 | Five levels, 50-100 μm, no CK-IHC | 90% (111/123) |
| Freneaux et al (2002)21 | Three levels, 150 μm, with CK-IHC | 97% (72/74) |
| Yared et al (2002)22 | Three adjacent levels with one CK-IHC | 98% (94/96) |
Before publication of the sixth edition of the AJCC Cancer Staging Manual,24 isolated tumor cells (ITCs) were commonly considered micrometastases; therefore, the early SLN studies tended to overstate the frequency of micrometastasis compared with current practice because the minimal findings on cytokeratin stains or step sections are commonly ITCs, classified as N0(i+). The goal today should be to detect all cases with nodal macrometastasis and the large majority of cases with micrometastasis as currently defined by the 0.2-mm threshold. Several histologic levels (2 to 4) with CK-IHC accomplish that goal with a high degree of accuracy. In clinical practice, the pathologist who encounters multiple ITC clusters, in a limited section protocol, may choose to examine deeper levels to exclude fusion of those clusters as a micrometastasis or macrometastasis deeper in the paraffin block.
Both superficial and limited deeper histologic sections are needed to reduce variations in gross sections, to ensure adequate examination of the capsular–subcapsular areas, and to control different sizes and shapes of lymph nodes. It is best for an institution to have a single protocol with a limited number of histologic and CK-IHC levels, usually 2 to 4 levels separated by a specified interval in the paraffin block, so that histotechnologists can follow the protocol systematically. The levels are typically separated by 100 or 200 μm, but may be up to 500 μm or as little as 50 μm apart. Both H&E and CK-IHC stains should be examined at each level so that any cytokeratin-positive finding can be closely scrutinized on the corresponding H&E section and any suspicious finding on H&E stain can be discounted when the adjacent cytokeratin stain is negative.
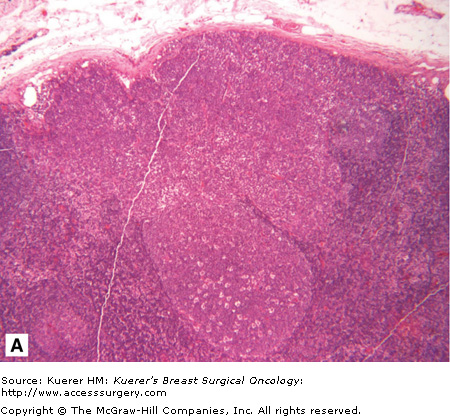
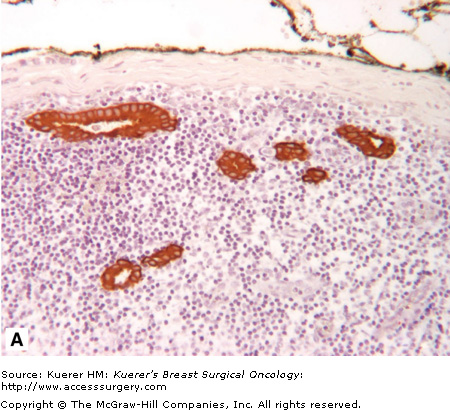
Standard H&E examination of lymph nodes reliably detects macrometastases but commonly fails to identify small metastases, which are easily missed because their shapes and colors may not be obvious in the background of reactive lymphoid tissue (Fig. 26-3). CK-IHC provides a sharp contrast between metastases and lymph node cellular constituents and permits consistent identification and measurement of tumor cell deposits. The value of adding IHC to the SLN work-up is to avoid missing metastases that should have been seen on H&E stains; this promotes reproducible pathology reporting and assures patients that their SLN results are accurate.
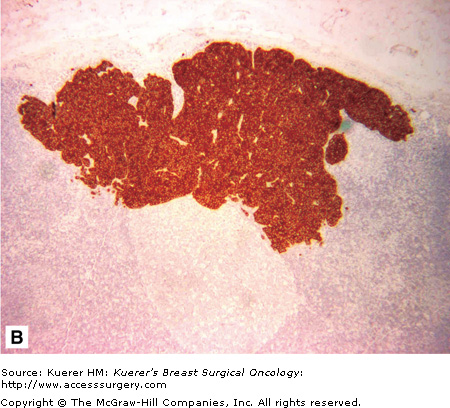
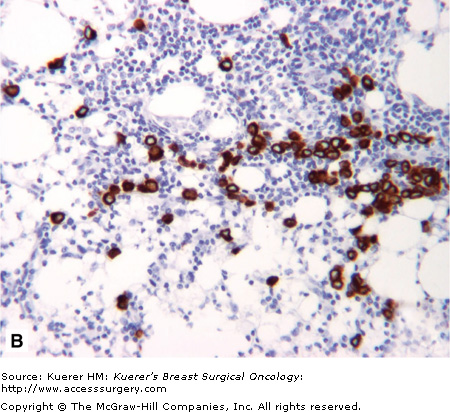
The American Joint Committee on Cancer (AJCC) staging system24 provides a framework for consistent diagnosis of nodal metastases, with measurement thresholds up to 0.2 mm for ITCs (pN0[i+]), up to 2.0 mm for micrometastasis (pN1mi), and greater than 2.0 mm for macrometastasis (pN1a). However, histologic criteria for classification of multiple clusters or single dispersed tumor cells, as commonly seen with lobular carcinomas (Fig. 26-4), are unclear in the sixth edition of the AJCC Cancer Staging Manual, which has led to variable application among pathologists. The new category of ITC, plus the use of different terminology in the International Union Against Cancer system, has contributed to diagnostic variation.25,26
Reproducible reporting is readily achievable using strict, simple criteria for measurement of tumor cluster size. In the presence of multiple clusters and single cells, the greatest dimension of the largest cluster is used for classification, irrespective of the number of clusters. These criteria have demonstrated a high level of reproducibility among pathologists, without which valid statistical comparisons between institutions and pathologists would not be possible. The proposed clarification of the AJCC system26 may have a bias toward a lower nodal stage and more ITC diagnoses, with a trend toward a higher frequency of non-SLN positivity in patients with SLN ITCs, but this may not be statistically significant.27 A basic tenet of the AJCC system is that clinicians faced with a borderline finding should select the lower stage category. Understaging is appropriate with minimal nodal disease and causes substantially less diagnostic variation than the overstaging that occurs when tumor cells clusters are summed or spanned in adjusted measurements.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree