Oncologic Components of Lymphadenectomy
CRITICAL ELEMENTS
Resection of lymph nodes in the central compartment
Management of the recurrent laryngeal nerve when involved by extranodal extension from lymph node metastases
Management of clinically positive lymph nodes in the lateral neck
Management of extranodal extension in the lateral neck
1. RESECTION OF LYMPH NODES IN THE CENTRAL COMPARTMENT
Recommendation: A central compartment neck dissection that includes resection of the lymph nodes within the paratracheal, paraesophageal, prelaryngeal, and pretracheal areas should be performed routinely during thyroidectomy for papillary thyroid cancer with clinically involved lymph nodes in the central or ipsilateral lateral compartments.
Type of Data: Retrospective case series.
Grade of Recommendation: Strong recommendation, moderate-quality evidence.
Rationale
Involvement of cervical lymph nodes in papillary thyroid cancer (PTC) is common and occurs in 20% to 50% of patients.52,53,54,55,56 The presence of lymph node metastases may increase recurrence rates and decrease long-term survival.57,58,59,60,61 Both macroscopic (clinically involved) and microscopic (pathologically involved) lymph node metastases are encountered in PTC; however, the significance of micrometastatic disease in relationship to outcomes may be minimal.62,63,64 In the absence of macroscopic disease,
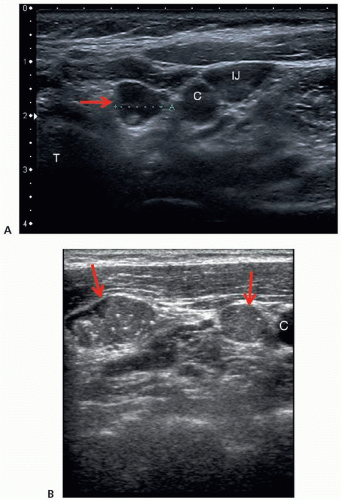
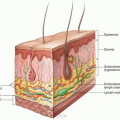
a prophylactic neck dissection is controversial (see discussion later in this chapter’s Key Question). Preoperative ultrasonography is important in determining the presence of macroscopic lymph node metastases, which will be clinically evident in approximately 20% to 31% of cases and, if present, may potentially alter the surgical approach (Fig. 2-1).65,66,67,68,69 Identification of involved central compartment (level VI) lymph nodes by ultrasonography may be limited because of the overlying thyroid, depth from the skin, or acoustic shadowing from the manubrium and clavicles.70,71,72,73
a prophylactic neck dissection is controversial (see discussion later in this chapter’s Key Question). Preoperative ultrasonography is important in determining the presence of macroscopic lymph node metastases, which will be clinically evident in approximately 20% to 31% of cases and, if present, may potentially alter the surgical approach (Fig. 2-1).65,66,67,68,69 Identification of involved central compartment (level VI) lymph nodes by ultrasonography may be limited because of the overlying thyroid, depth from the skin, or acoustic shadowing from the manubrium and clavicles.70,71,72,73
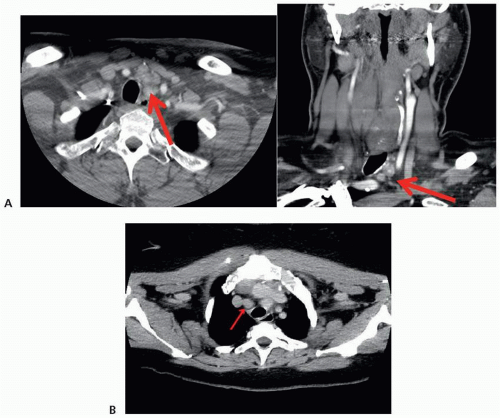
Therefore, adjunct cross-sectional imaging (typically contrast-enhanced computed tomography [CT]) can be helpful in analyzing the central compartment and superior mediastinal lymph node basins if there is suspicion of disease not readily visualized on ultrasonography (Fig. 2-2).70,71,72,73 Gross inspection of the central neck compartment lymph tissue at the time of thyroidectomy should also be performed, given this adenopathy is readily encountered during the procedure.
The most common site of lymph node metastasis in PTC is the central compartment.74 Therapeutic surgical resection of involved lymph nodes with the use of compartment-oriented, en bloc resection of the lymph nodes in the involved compartments provides the best treatment for cervical lymph node metastasis and is well established.42,57,75,76,77 Macroscopic cervical lymph nodes cannot be adequately treated with radioactive iodine (RAI) therapy alone. Metastatic lymph nodes are the most common cause of persistent and recurrent PTC after initial treatment.78,79,80 Persistent lymph node metastasis after thyroidectomy often occurs because of lack of or inaccurate preoperative imaging and subsequent omission of or incomplete lymphadenectomy in patients with clinically involved lymph nodes at the time of initial surgical
treatment.81,82 Reoperative lymph node dissection for persistent and recurrent PTC carries a higher risk of surgical complications than does primary surgery.83 These issues underscore the utmost importance of accurate and complete preoperative and intraoperative analysis to allow for a definitive resection of both local and regional disease at the time of initial surgical treatment of PTC.
treatment.81,82 Reoperative lymph node dissection for persistent and recurrent PTC carries a higher risk of surgical complications than does primary surgery.83 These issues underscore the utmost importance of accurate and complete preoperative and intraoperative analysis to allow for a definitive resection of both local and regional disease at the time of initial surgical treatment of PTC.
An ipsilateral therapeutic CCND should be performed for macroscopic metastatic lymphadenopathy; if macroscopic disease is seen in the contralateral central compartment, bilateral therapeutic CCND should be performed.84,85,86 The role of a contralateral CCND, in the absence of a known contralateral cancer and no macroscopic evidence of metastatic lymphadenopathy in the contralateral central compartment, is controversial. However, intraoperative inspection of the central compartment has a poor predictive value for the presence of metastatic disease, and consideration could be given to proceeding with a contralateral dissection in the presence of ipsilateral macroscopic disease.87,88
Intraoperative decision-making plays an important role in the conduct of CCND. After ipsilateral dissection, the functional status of the RLN should be considered prior to completing the contralateral CCND, if being considered. Intraoperative RLN monitoring can be helpful in this decision-making process. For example, if the RLN is nonfunctional after the ipsilateral CCND, surgeons should carefully consider the implications before proceeding with a contralateral dissection. This is especially pertinent in the absence of clinically involved lymph nodes, considering the ramifications of bilateral RLN paralysis and the subsequent need for tracheostomy. A staged procedure might also be considered; however, if a total thyroidectomy has already been performed, the contralateral central compartment will become a reoperative field, which may be associated with higher rates of RLN injury or hypoparathyroidism. The viability of the parathyroid glands should also be a consideration during bilateral CCND. Care should be taken to preserve all parathyroid glands. If multiple glands have questionable viability, a limited contralateral dissection can be considered in order to preserve viable parathyroid tissue in those patients with no evidence of contralateral metastatic lymphadenopathy.
Technical Aspects
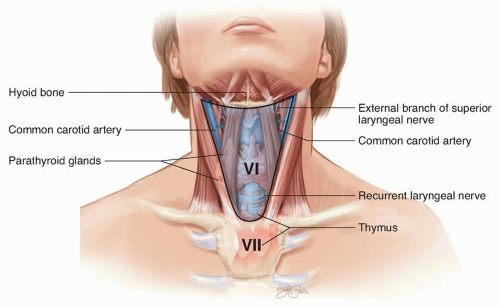
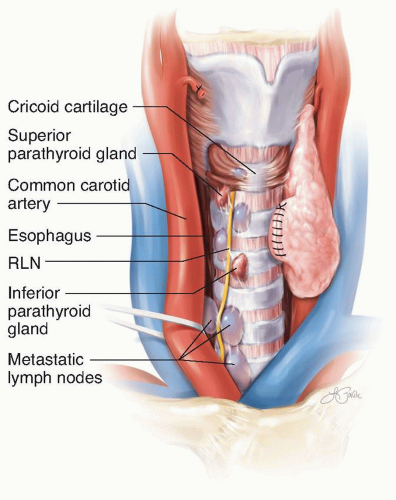
CCND typically can be accomplished through the lower cervical collar incision used for thyroidectomy. The central compartment of the neck is defined by anatomic boundaries, and CCND should be performed in a compartment-oriented manner, with en bloc resection of the lymph nodes contained within these boundaries.77,89,90 The central compartment is bounded cranially by the hyoid bone, caudally by the innominate artery on the right and the corresponding axial plane on the left, laterally by the common carotid arteries, posteriorly by the deep layer of the cervical fascia, and anteriorly by the superficial layer of the cervical fascia (Fig. 2-3). The thyroid and parathyroid glands, the level VI lymph nodes, the upper portion of the level VII lymph nodes, and the cervical portion of the thymus are within the central compartment. Common locations of metastatic central compartment lymph nodes include the paratracheal and paraesophageal lymph nodes inferior and posterior to
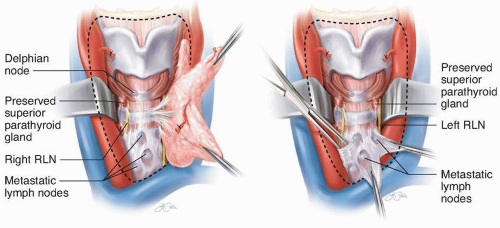
the thyroid, the pretracheal lymph nodes inferior to the thyroid isthmus, and the prelaryngeal (Delphian) lymph node(s) just superior to the thyroid isthmus (Fig. 2-4). The majority of the level VI lymph nodes are located inferior to the cricoid cartilage and posterior and inferior to the thyroid gland. The RLN can be situated anterior or posterior to involved central compartment lymph nodes, and care should be taken to examine behind the RLN to avoid missing lymph node metastasis, particularly on
the right side (Fig. 2-5). Central compartment nodal metastasis can also be situated posterior to the common carotid arteries and posterior to the innominate artery on the right, and care should be taken to include these lymph nodes during CCND. The retropharyngeal lymph nodes are rarely involved in PTC; however, primary tumors in the superior pole can metastasize to this location.91,92 Cervical ultrasonography will not visualize the retropharyngeal space, and contrast-enhanced cross-sectional imaging (typically CT) can be useful in evaluation if retropharyngeal and retroesophageal space involvement is suspected (Fig. 2-6).
the thyroid, the pretracheal lymph nodes inferior to the thyroid isthmus, and the prelaryngeal (Delphian) lymph node(s) just superior to the thyroid isthmus (Fig. 2-4). The majority of the level VI lymph nodes are located inferior to the cricoid cartilage and posterior and inferior to the thyroid gland. The RLN can be situated anterior or posterior to involved central compartment lymph nodes, and care should be taken to examine behind the RLN to avoid missing lymph node metastasis, particularly on
the right side (Fig. 2-5). Central compartment nodal metastasis can also be situated posterior to the common carotid arteries and posterior to the innominate artery on the right, and care should be taken to include these lymph nodes during CCND. The retropharyngeal lymph nodes are rarely involved in PTC; however, primary tumors in the superior pole can metastasize to this location.91,92 Cervical ultrasonography will not visualize the retropharyngeal space, and contrast-enhanced cross-sectional imaging (typically CT) can be useful in evaluation if retropharyngeal and retroesophageal space involvement is suspected (Fig. 2-6).
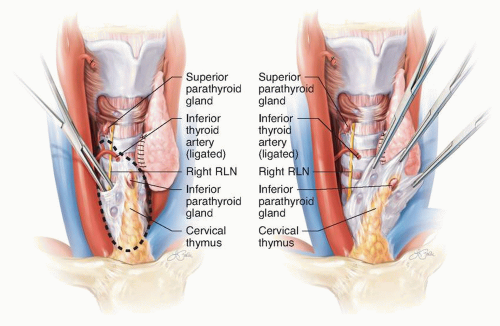
A CCND can be executed either by en bloc resection of the lymph nodes with the thyroid specimen or by separate resection. Removal of the thyroid initially may allow for easier visualization of the lymph nodes posterior to the thyroid and along the course of the RLN. Removal of the entire lymph node basin is recommended in patients with clinical involvement, and “berry picking” or “plucking” of individually involved nodes is not recommended and is associated with higher rates of persistent disease.42,93,94 Typical nodal yield from a bilateral level VI lymph node dissection can vary greatly; however, a recent study noted that patients with recurrent papillary thyroid cancer (PTC) had a lower mean nodal yield than those without recurrence, thus suggesting the importance of a complete CCND in the presence of nodal metastasis.95 Exposure of the entire anterior surface of the RLN is recommended, from its insertion point at the cricothyroid muscle to its proximal extent as it emanates from the mediastinum. This allows for removal of the lymph nodes anterior to the RLN with direct
visualization of the nerve as dissection progresses either distally or proximally along the nerve. In some instances individual lymph nodes situated posterior to the RLN can be removed separately if en bloc removal with the lymph nodes anterior to the nerve would stretch or place undue tension on the RLN.96 Common locations of missed metastatic central compartment lymph nodes include nodes posterior to the RLN, those posterior to the common carotid artery, and those extending below the level of the sternal notch in the paraesophageal and paratracheal spaces and into the superior portion of level VII.
visualization of the nerve as dissection progresses either distally or proximally along the nerve. In some instances individual lymph nodes situated posterior to the RLN can be removed separately if en bloc removal with the lymph nodes anterior to the nerve would stretch or place undue tension on the RLN.96 Common locations of missed metastatic central compartment lymph nodes include nodes posterior to the RLN, those posterior to the common carotid artery, and those extending below the level of the sternal notch in the paraesophageal and paratracheal spaces and into the superior portion of level VII.
 FIGURE 2-6 Right retropharyngeal lymph node metastasis (arrow) visible on computed tomography scan enhanced with intravenous contrast. |
Preservation of parathyroid gland function is important during CCND. The superior parathyroid glands typically derive arterial supply from branches of the inferior thyroid artery, and avoidance of high ligation of the inferior thyroid artery can help with preservation of the vascular pedicle. In some circumstances, a branch of the superior thyroid artery supplies the superior parathyroid glands, and confirmation of viability after thyroidectomy is warranted. The inferior parathyroid glands are typically more closely associated with the lymph nodes removed during CCND and may therefore be difficult or impossible to preserve in situ on their vascular pedicles (Fig. 2-7). The inferior parathyroid glands also are often in close association to or within the thyrothymic tract, which runs through the anterior aspect of the inferior level VI lymph nodes. The thyrothymic tract and cervical portion of the thymus do not necessarily need to be excised during a CCND, and preservation may aid in preserving the viability of the inferior parathyroid glands that reside in the cervical thymus.97 Devascularization or inability to preserve the parathyroid glands in situ should prompt reimplantation of parathyroid tissue into a viable muscle within the operative field (typically the sternocleidomastoid muscle [SCM]). Confirmation of parathyroid tissue
by microscopic examination may help avoid inadvertent reimplantation of tumor or nodal metastasis. Addition of a CCND to total thyroidectomy has been shown to increase parathyroid reimplantation rates and temporary hypoparathyroidism but not permanent hypoparathyroidism.52,76,98,99,100,101,102
by microscopic examination may help avoid inadvertent reimplantation of tumor or nodal metastasis. Addition of a CCND to total thyroidectomy has been shown to increase parathyroid reimplantation rates and temporary hypoparathyroidism but not permanent hypoparathyroidism.52,76,98,99,100,101,102
At least an ipsilateral CCND should be performed in patients with lateral compartment lymph node (levels II to V) involvement. In general, lymph node metastases spread in a centripetal manner, and although “skip metastases” (no evidence of central compartment lymph nodes in the presence of lateral compartment nodal involvement) are described, their occurrence is atypical. Most patients with lateral compartment nodal involvement will also have metastatic central compartment lymph nodes.103,104,105
Level VII lymph nodes reside in the superior mediastinum caudal to the innominate artery on the right and the corresponding axial plane on the left. The level VII nodal basin is not typically involved in a CCND; however, lymph node involvement in this basin is not uncommon in patients whose lymph node metastasis is more extensive than usual.106 Transcervical access to level VII is feasible in the initial and reoperative settings, and partial or complete sternotomy is rarely indicated.
When central compartment lymph nodes encountered during thyroidectomy are suspected of harboring metastases, intraoperative pathology consultation can be helpful in determining the presence of metastatic disease.107 Visual inspection has been shown to have poor predictive value in central compartment nodal metastasis.87,88 Sentinel lymph node biopsy for PTC has been described, but the practice has not been
widely adopted.108,109 If microscopic examination is consistent with cervical lymph node metastases, a compartment-oriented ipsilateral or bilateral CCND should be performed. Given the poor predictive value of ultrasonography of the central compartment and of visual inspection, surgeons should anticipate the need for CCND at the time of initial thyroidectomy for PTC and discuss this potential with the patient; if a surgeon is not experienced with CCND, consideration should be given to referring the patient to a surgeon with a high-volume CCND caseload, because complication rates are lower in high-volume centers.110,111,112,113
widely adopted.108,109 If microscopic examination is consistent with cervical lymph node metastases, a compartment-oriented ipsilateral or bilateral CCND should be performed. Given the poor predictive value of ultrasonography of the central compartment and of visual inspection, surgeons should anticipate the need for CCND at the time of initial thyroidectomy for PTC and discuss this potential with the patient; if a surgeon is not experienced with CCND, consideration should be given to referring the patient to a surgeon with a high-volume CCND caseload, because complication rates are lower in high-volume centers.110,111,112,113
2. MANAGEMENT OF THE RECURRENT LARYNGEAL NERVE WHEN INVOLVED BY EXTRANODAL EXTENSION FROM LYMPH NODE METASTASES
Recommendation: Lymph nodes with extranodal extension that involves the recurrent laryngeal nerve should be resected to avoid leaving gross residual disease while attempting to preserve the integrity of the recurrent laryngeal nerve.
Type of Data: Retrospective case series.
Grade of Recommendation: Strong recommendation, moderate-quality evidence.
Rationale
Gross extranodal extension of PTC nodal metastasis is uncommon, but it is associated with increased risk of recurrence.60,64,114,115,116 Extranodal extension rarely involves the recurrent laryngeal nerve (RLN). Preoperatively, this may be evident in patients presenting with unilateral RLN paralysis. Intraoperative discovery of extranodal extension involving a functional RLN is also a rare occurrence; however, the surgeon should attempt disease resection to preserve the nerve anatomically and functionally without leaving gross disease. Intraoperative RLN monitoring can be especially helpful in these more difficult situations.
Technical Aspects
Intraoperative management of central compartment lymph node metastases with extranodal extension involving the RLN should be considered in the context of the functionality of the nerve. In patients with extranodal macroscopic disease and a nonfunctional nerve, the nerve should be resected to achieve a complete (R0) resection. In patients with extranodal macroscopic disease with a functioning RLN, attempts at preservation of the nerve anatomically and functionally should be made with a shave resection to remove all gross disease, even if this achieves only an R1 resection (microscopically positive margin), because outcomes appear similar between R0 and R1 resections.117 A shave resection can be performed with sharp dissection of the involved node away from the neural sheath, excising as much of the node as possible while preserving the nerve. Immediate nerve reconstruction in short segment resections with direct neural anastomosis can be considered if a surgeon with experience in microanastomotic techniques is available.118,119
3. MANAGEMENT OF CLINICALLY POSITIVE LYMPH NODES IN THE LATERAL NECK
Recommendation: In patients with clinically involved lateral compartment lymph nodes, a compartment-oriented, en bloc lymphadenectomy should be performed. A prophylactic lateral compartment neck dissection is not recommended.
Type of Data: Retrospective case series.
Grade of Recommendation: Strong recommendation, moderate-quality evidence.
Rationale
Macroscopic lymph node involvement is not effectively treated with RAI therapy alone; therefore, surgical excision of metastatic lymph nodes provides the best option for regional control of disease. A compartment-oriented lymphadenectomy provides the most effective clearance of metastatic lymph nodes rather than removal of individually involved nodes (“berry picking”).
In patients with PTC, metastases to the regional lymph nodes is common. Metastases are most common in the central compartment, followed by the ipsilateral lateral compartment.93,94,120 Metastases to the contralateral lateral compartment or skip metastases (no clinical or pathologic evidence of central compartment metastasis with verified ipsilateral lateral compartment metastasis) can occur, but both are rare.103,104,105 The presence of lateral compartment lymph node metastasis has been shown to confer a decrease in long-term survival in older patients with PTC.64,121
Preoperative imaging of the lateral compartments is important because it can identify lymph nodes with abnormalities suggestive of metastasis.65,66,67,68,69,71,73,74,93,94 Confirmation of metastasis by fine-needle aspiration (FNA) biopsy should be performed prior to lateral compartment lymph node dissection. Even if there is only one metastatic node identified preoperatively, additional microscopic metastases are often present; therefore, a compartment-oriented dissection of the involved compartment should be performed.73,106,122,123,124,125,126 “Berry picking” lymph nodes in the lateral neck is discouraged, because it underestimates the extent of disease, may undertreat patients, and may make a future reoperative neck dissection more difficult.33,126,127,128,129,130,131,132
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree