New Imaging Techniques for the Diagnosis of Early Gastric Cancer and Premalignant Lesions
Thomas Paulraj Thamboo
Zhiwei Huang
Ming Teh
INTRODUCTION
The advent of the flexible endoscope has revolutionized gross examination of the stomach and allowed real-time examination of subtle mucosal changes in situ. In practice, this enables directed biopsies of gastric mucosa for early premalignant changes and malignant lesions. Naturally, this has tremendous implications for screening surveillance programs for gastric cancers, as well as for patients on follow-up for conditions predisposing them to the development of gastric malignancies. Also, in endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD)— increasingly the definitive treatment for many early intestinal-type gastric cancers and high-grade dysplasias-careful endoscopic visualization is indispensable in ensuring the lesion is completely excised.
We hope that this chapter’s images and descriptions of the different endoscopic modalities can serve as a useful introduction for the practicing GI pathologist to the tremendous advances in endoscopic imaging. Except for Raman spectroscopy, which could conceivably gain greater acceptance in the future, these techniques use conventional images, either “gross” or “microscopic.” Notwithstanding the universal acknowledgement that histological analysis remains the diagnostic gold standard and is likely to continue to do so for a very long time, a basic understanding of these endoscopic images, easily accessible from most hospital information systems, can be helpful to the practicing GI pathologist and might just provide the gross-histological or light microscopicendoscopic correlation that is so necessary in difficult diagnostic situations.
WHITE LIGHT REFLECTANCE ENDOSCOPY (CONVENTIONAL ENDOSCOPY)
White light reflectance forms the basis of conventional endoscopic examination and imaging and continues to be the modality used in most gastroscopic procedures, either on its own or in combination with newer techniques (image-enhanced endoscopy, see below). In white light reflectance endoscopy, white light is channeled to the tip of the endoscope via optical fibers and illuminates the gastric mucosa. Light reflected from the mucosa is received by a lens in the endoscope
tip and channeled to a video CCD. This enables real-time video imaging of the mucosa with the ability to obtain a video recording of the procedure, as well as still images of selected fields. More recently, endoscopic magnification techniques have allowed the acquisition of magnified images of the mucosa under white light. Magnifying endoscopy has been shown to be able to identify gastric carcinoma on the basis of changes in the pattern of the gastric pits and mucosal microvasculature.1, 2 and 3 Magnifying endoscopy has also been used in conjunction with other techniques that enhance contrast (see below), for detection of intestinal metaplasia and dysplasia.4, 5 and 6
tip and channeled to a video CCD. This enables real-time video imaging of the mucosa with the ability to obtain a video recording of the procedure, as well as still images of selected fields. More recently, endoscopic magnification techniques have allowed the acquisition of magnified images of the mucosa under white light. Magnifying endoscopy has been shown to be able to identify gastric carcinoma on the basis of changes in the pattern of the gastric pits and mucosal microvasculature.1, 2 and 3 Magnifying endoscopy has also been used in conjunction with other techniques that enhance contrast (see below), for detection of intestinal metaplasia and dysplasia.4, 5 and 6
IMAGE ENHANCED ENDOSCOPY
“Image enhanced endoscopy” is a term proposed by the American Gastroenterological Association to describe various means of enhancing contrast during endoscopy, using dye, optical, or electronic methods.7 These techniques include chromoendoscopy, autofluorescence imaging (AFI) endoscopy, and narrow-band imaging (NBI). Confocal laser endomicroscopy is another technique that allows improved visualization of the mucosa during endoscopy, but this relies on increasing magnification rather than contrast. Other techniques are currently under study as well.
CHROMOENDOSCOPY
Chromoendoscopy, probably the oldest method of image enhancement in endoscopy, involves the application of dyes or stains to the mucosal surface during endoscopy in order to enhance the appearance of mucosal lesions and better differentiate them from surrounding normal mucosa under conventional white light. Staining is performed during the endoscopy procedure, and the stain may be applied to a wide area of the mucosa or targeted on a visible lesion. Contrast stains, such as indigo carmine, tend to concentrate in depressions and crevices in the mucosa, and in so doing, highlight the mucosal surface architecture and topography. Absorptive stains, such as methylene blue, are preferentially taken up by intestinal absorptive cells, which are then highlighted against the rest of the mucosa. Reactive stains, such as Congo red, react chemically with certain substances within cells, giving rise to a color change.
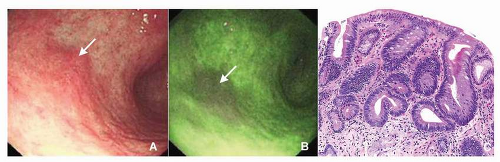
Indigo carmine is the most commonly used contrast stain in gastric chromoendoscopy. It has been used for over 30 years and continues to be shown to improve the endoscopic visualization of gastric neoplasia as compared to white light examination alone.8 The dye allows visualization of the disordered gross architecture of the mucosa associated with gastric dysplasia and carcinoma (Fig. 12-1). Recently, indigo carmine combined with acetic acid has shown potential to be even more effective than indigo carmine alone in highlighting areas with gastric neoplasia.8, 9 and 10
Methylene blue staining has been shown to improve the detection of intestinal metaplasia in the stomach.4,5,11,12 The dye is applied to the mucosa, followed by irrigation with water. Areas of intestinal metaplasia show persistent blue staining with this technique, while normal nonmetaplastic mucosa is not stained. Magnification chromoendoscopy using methylene blue has been shown to be able to detect intestinal metaplasia and dysplasia with an accuracy of 84% and 83%, respectively.4 Areas of intestinal metaplasia stained blue but maintained a regular mucosal pattern. Areas of dysplasia showed no clear color change but showed loss of the regular mucosal pattern. A more recent study has shown this technique to be reproducible with high specificity (99%) for detection of dysplasia.13
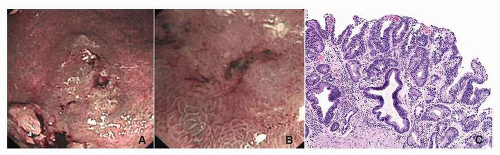
AUTOFLUORESCENCE
AFI endoscopy involves illumination of the gastric mucosa with blue (short-wavelength) light that stimulates endogenous substances to fluoresce, that is, to emit visible light of a longer wave-length. These fluorescent substances, also known as fluorophores, vary in their distribution and concentration in different tissue types. Thus, under endoscopy, metaplastic and neoplastic tissue can be identified, as it has different autofluorescent colors compared to normal tissue. These differences can be enhanced by AFI systems to produce real-time images (Fig. 12-2).
AFI endoscopy has been shown to be able to identify gastric neoplasms, including early gastric cancers.14,15 However, study results are mixed. One study found that for detection of early gastric neoplasia, AFI was less sensitive (68.1%) and specific (23.5%) than white light imaging (sensitivity 76.6%; specificity 84.3%).16 Another study similarly found AFI to be of limited utility for the diagnosis of gastric neoplasia, with a sensitivity of 96.4% but a specificity of 49.1%.14 Nonetheless, one study has shown that autofluorescence may be better than white light imaging at detecting the lateral extent of early gastric cancers, especially when these lateral extensions are flat or isochromatic, but was still not as good as chromoendoscopy15 AFI in combination with other modalities will likely prove more useful, and a combination of AFI, white light imaging, and NBI (trimodal imaging endoscopy) has been shown to be more sensitive and specific than AFI or white light imaging alone.16
NARROW-BAND IMAGING
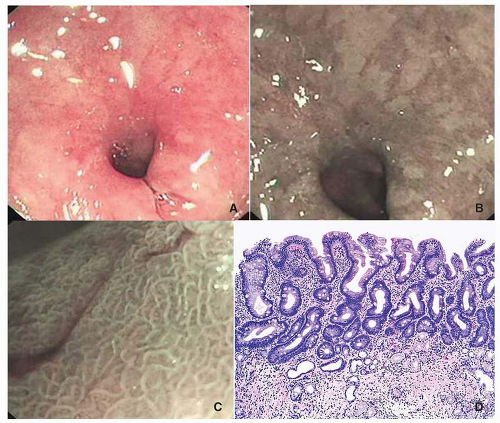
NBI consists of illuminating the mucosa with selected narrow bands of wavelengths of light. White light from a conventional white light source is passed through narrow band filters to produce narrow bands of blue (centered on 415 nm) and green (centered on 540 nm) light that illuminate the mucosa. These bands of light are reflected by the mucosal surface but are maximally absorbed by hemoglobin within blood vessels. The reflected light from the bands is captured, either sequentially or simultaneously, and analyzed and displayed as an image. The images obtained with NBI
thus show the mucosa and its vascular network with enhanced contrast. As disease processes alter the mucosal structure and vascular network, these changes allow the identification of preneoplastic and neoplastic changes (Figs. 12-3 and 12-4). Under NBI, areas with intestinal metaplasia appear to have a light blue crest (blue-white lines on the epithelial surface) (Fig. 12-5).17 Uedo et al. showed that NBI can demonstrate intestinal metaplasia in the gastric mucosa with a sensitivity and specificity of 89% and 93%, respectively.17
thus show the mucosa and its vascular network with enhanced contrast. As disease processes alter the mucosal structure and vascular network, these changes allow the identification of preneoplastic and neoplastic changes (Figs. 12-3 and 12-4). Under NBI, areas with intestinal metaplasia appear to have a light blue crest (blue-white lines on the epithelial surface) (Fig. 12-5).17 Uedo et al. showed that NBI can demonstrate intestinal metaplasia in the gastric mucosa with a sensitivity and specificity of 89% and 93%, respectively.17
With NBI, superficial gastric cancer shows an irregular microvascular pattern6,18 and an irregular pattern of the mucosal surface. Three microvascular patterns (fine network; corkscrew and unclassified) are recognized in early gastric cancers with the first two more common in differentiated (tubular) and undifferentiated (discohesive), respectively.18 However, there is currently no evidence that NBI is superior to magnified white light imaging for the detection of early gastric neoplasms, and prospective controlled trials are lacking.19,20 Nonetheless, NBI with magnification has been shown to be effective in identifying the lateral extent of superficial gastric cancer,6 which is useful in guiding EMR or ESD of these lesions.
CONFOCAL LASER ENDOMICROSCOPY
Confocal laser endomicroscopy (CLE) is a technique that enables in vivo visualization of the gastric mucosa at a microscopic level, providing real-time “virtual histology” images. A low-powered laser is transmitted through an optical fiber and focused through a lens onto a point on the mucosa. Light reflected from the illuminated point is focused by the same lens to converge back into the optical fiber (Fig. 12-6). In this way, the illuminating (incident) light and the reflected light detected by the system are in the same focal plane, hence the term “confocal.” Light that is reflected back (or scattered) from other points and from other focal planes is rejected. This provides for a sharp, high-resolution optical image representing the tissue in one focal plane only.
Intravenous and topical fluorescence contrast agents that fluoresce under the incident laser light21 are used in order to achieve high contrast at high resolution. The most commonly used




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree