Pancreatic adenocarcinoma (PDA) is a highly lethal and aggressive malignancy with high mortality rates. It is critical to evaluate novel therapeutic strategies and targets for the treatment of this disease. In this article, the authors describe the important areas of focus in pancreatic cancer research, recent advances in these areas, and novel approaches that have the potential to bring about positive patient outcomes in this lethal disease. This article also focuses on recent developments in identifying new, more sensitive, and more specific blood biomarkers with potential use in the early detection of PDA.
Pancreatic adenocarcinoma (PDA) is a highly lethal and aggressive malignancy with high mortality rates. Surgical resection remains the only potential curative option for pancreatic cancer. But most cases of pancreatic cancer at presentation have evidence of locally advanced or metastatic disease and are left with no curative option. At diagnosis, only about 15% of patients are candidates for pancreatic resection; yet even in patients who undergo a successful surgical resection, the 5-year survival rate is only about 25% to 30% for node-negative tumors and 10% for node-positive tumors. Patients with metastatic disease have a poor prognosis, with a median survival of less than 6 months. The benefit associated with standard gemcitabine-based chemotherapy and radiation is modest, with improvements in overall survival measured in months as compared with that associated with best supportive care. During the past decade, several new chemotherapeutic and targeted therapeutic modalities have been tested in clinical trials. However, the outcome for pancreatic cancer remains dismal, with most therapies being ineffective. Hence, it is critical to evaluate novel therapeutic strategies and targets for the treatment of this disease. In this article, the authors describe the important areas of focus in pancreatic cancer research, recent advances in these areas, and novel approaches that have the potential to bring about positive patient outcomes in this lethal disease.
Early detection biomarkers in PDA
Major advances in pancreatic cancer control can be greatly aided by early detection for diagnosing and treating the disease in its preinvasive state before the development of metastases. Hence, a successful screening strategy would be targeted at the identification of biomarkers that are capable of detecting preinvasive lesions of the pancreas. Early detection of preinvasive lesions of the pancreas may be possible through noninvasive means (imaging) and invasive means (pancreatic juice analysis or profiling of patient serum). Given the complexity and high cost-to-benefit ratio of imaging methodologies, such as helical computed tomography (CT), magnetic resonance imaging, positron emission tomography scan, endoscopic ultrasound (EUS), and endoscopic retrograde cholangiopancreatography for obtaining pancreatic juice for analysis, these technologies are unlikely to be adopted for mass screening. Therefore, most interest has been focused on identifying new blood biomarkers for the early detection of PDA. Existing biomarkers for this disease are inadequate. Carbohydrate antigen (CA) 19-9 has been tested for its utility as an early detection marker for pancreatic cancer. However, the sensitivity and specificity of this biomarker are not high, and serum levels are significantly increased in inflammatory diseases of the pancreas and the biliary tract. Therefore, CA19-9 is not useful for early diagnosis, mass screening, or distinguishing between PDA and chronic pancreatitis. Thus, a great need exists for new biomarkers for PDA. The following sections focus on recent developments in identifying new, more sensitive, and more specific blood biomarkers with potential use in the early detection of PDA.
Autoantibodies to tumor-associated antigens
The humoral immune response to cancer in humans has been well demonstrated by the identification of autoantibodies to several different intracellular and surface antigens in patients with various tumor types. A tumor-specific humoral immune response directed against oncoproteins or mutated proteins, such as p53 or other aberrantly expressed proteins, has been described. Although it is currently unknown whether the occurrence of such antibodies is beneficial, knowledge of potential tumor antigens that may evoke tumor-specific immune responses may have utility in early cancer diagnosis. In pancreatic cancer, autoimmunity has been shown against several cellular proteins, including mucin 1 (MUC1), p53, RAD51, and DEAD-box protein 48. Autoantibodies to MUC1, a transmembrane glycoprotein involved in cell-cell and cell–extracellular matrix interactions, have been observed in sera from patients with various tumors. In pancreatic cancer, the presence of MUC1 immunoglobulin G autoantibodies has been shown to be associated with a favorable prognosis. The presence of p53 autoantibodies has been observed in 18.2% of patients with pancreatic cancer. However, p53 autoantibodies were also found in 5.3% of patients with acute pancreatitis and 12.1% of patients with chronic pancreatitis; thus the humoral response to p53 was not specific to malignancy. The recombination factor RAD51 is highly expressed in PDA, and RAD51 autoantibodies have been observed in 7% of patients with pancreatic cancer. Autoantibodies to DEAD-box protein 48, a member of the DEA (D/H)-box RNA helicase family, were observed in the serum from 63.6% of patients with pancreatic cancer but were found in the serum from only 1.9% of normal subjects. Analysis of autoantibodies to tumor-associated antigens (TAAs) in PDA has been limited because only a small subset of patients (typically <50%) with PDA develop humoral response to a specific TAA. Moreover, the development of an adequate humoral immune response is also influenced by intersubject variability in the major histocompatibility antigens and resultant variability in immune responses, thus limiting the utility of this technique.
Autoantibodies to tumor-associated antigens
The humoral immune response to cancer in humans has been well demonstrated by the identification of autoantibodies to several different intracellular and surface antigens in patients with various tumor types. A tumor-specific humoral immune response directed against oncoproteins or mutated proteins, such as p53 or other aberrantly expressed proteins, has been described. Although it is currently unknown whether the occurrence of such antibodies is beneficial, knowledge of potential tumor antigens that may evoke tumor-specific immune responses may have utility in early cancer diagnosis. In pancreatic cancer, autoimmunity has been shown against several cellular proteins, including mucin 1 (MUC1), p53, RAD51, and DEAD-box protein 48. Autoantibodies to MUC1, a transmembrane glycoprotein involved in cell-cell and cell–extracellular matrix interactions, have been observed in sera from patients with various tumors. In pancreatic cancer, the presence of MUC1 immunoglobulin G autoantibodies has been shown to be associated with a favorable prognosis. The presence of p53 autoantibodies has been observed in 18.2% of patients with pancreatic cancer. However, p53 autoantibodies were also found in 5.3% of patients with acute pancreatitis and 12.1% of patients with chronic pancreatitis; thus the humoral response to p53 was not specific to malignancy. The recombination factor RAD51 is highly expressed in PDA, and RAD51 autoantibodies have been observed in 7% of patients with pancreatic cancer. Autoantibodies to DEAD-box protein 48, a member of the DEA (D/H)-box RNA helicase family, were observed in the serum from 63.6% of patients with pancreatic cancer but were found in the serum from only 1.9% of normal subjects. Analysis of autoantibodies to tumor-associated antigens (TAAs) in PDA has been limited because only a small subset of patients (typically <50%) with PDA develop humoral response to a specific TAA. Moreover, the development of an adequate humoral immune response is also influenced by intersubject variability in the major histocompatibility antigens and resultant variability in immune responses, thus limiting the utility of this technique.
Serum and proteomic profiling studies and biomarkers
Scientists have sought to identify other potential biomarkers for PDA using genomic analysis of primary pancreatic cancers, with results compared with those obtained from samples of chronic pancreatitis (a control for the extensive fibrosis and inflammation seen in PDA) and normal pancreas. Using such an approach, several potential biomarkers have been identified for PDA that outperform CA19-9. Two new serum biomarkers identified from such gene expression studies were carcinoembryonic antigen-related cell adhesion molecule 1 and macrophage inhibitory cytokine-1 (MIC-1). Both markers were found to be superior to CA19-9 in distinguishing cancer from normal but not from chronic pancreatitis. In both studies, the combination of either CEACAM1 or MIC-1 with CA19-9 enhanced the performance of the assay. In an additional study using a novel immunoassay, MUC1 was reported to be superior to CA19-9 and more effective in differentiating pancreatic cancer from chronic pancreatitis. Several studies support the use of a panel of biomarkers as opposed to single biomarkers, but such a panel is yet to be defined.
Glycoproteomics
Posttranslational modification of the proteome has recently emerged as a cornerstone in biomarker analysis. The study of glycosylation patterns of serum proteins in cancer constitutes the basis of glycoproteomics. In fact, most tumor markers currently used in the clinical setting are serum glycoproteins. Alterations in the pattern of protein glycosylation have been found to occur during carcinogenesis and contribute to the neoplastic phenotype. Alterations in glycosylation patterns in major glycoproteins in serum have been identified and shown to correlate with the progression of PDA. Because the altered glycosylation patterns occur in normal versus tumor cells and also in preinvasive lesions, they may have utility in early diagnosis. The identification and assay of disease-related glycan structures have been accomplished using several methodologies, including liquid separations, protein microarrays, and mass spectrometry.
In addition to the high sensitivity, the specificity of detecting disease-related glycan structures is further aided by the incorporation of lectins, which specifically and reversibly bind to glycans with different structural moieties. Lectin glycoarrays have been used for high-throughput profiling of glycan expression patterns of various glycoproteins in PDA and chronic pancreatitis. The clinical utility of lectin glycoarray data has been further optimized using bioinformatics analysis to identify and highlight a lectin response signature for specific disease states. Using lectin glycoarrays, certain glycoprotein alterations, such as increased sialylation and fucosylation on several proteins, including hemopexin, kininogen-1, and antithrombin III, seem to be present in pancreatic cancer sera as compared with normal and chronic pancreatitis sera. In PDA, processes such as fucosylation and sialylation appear to be specific and have been noted to be a predominant change that correlates with disease progression.
The specificity of lectin glycoarrays has been improved further by using an antibody-based “sandwich technique” whereby microarrays using antibodies to previously identified PDA-associated glycoproteins were made. These were then coated with patient serum to extract the target glycoproteins. Lectins were then used to detect variation in the glycan structure. This methodology had high sensitivity and specificity in detecting PDA in sera samples. In addition to improved sensitivity and specificity, glycoproteomics have the additional advantage of performing direct analysis in samples without purification of proteins. In summary, analysis of glycosylation patterns of candidate glycoproteins is a promising tool for early detection of PDA in the future. In addition to its utility in diagnosis, it could also serve as a potential prognostic and decision-making aid for personalized treatment of PDA.
Integrative web-based platforms to assist in biomarker identification
Technological advances in genomics and proteomics have facilitated high-throughput studies in which large datasets are generated and data are analyzed in isolation compared with other published data that may be buried in supplemental tables. It is clear that a central repository or Web portal of such data would be extremely useful in the biomarker field. Several such repositories have recently been compiled. Oncomine is a public cancer microarray platform, which spans 35 tumor types and incorporates data from 264 independent microarray datasets. It provides a compendium of genomic datasets with the incorporation of data from other public datasets. Yang and colleagues identified potential biomarkers in Oncomine using a software program called the Ingenuity Pathways Analysis program. In addition to the identification of biomarkers that are unique to a specific cancer type, several shared biomarkers among different tumor types were also identified. Hence, genomic databases, such as Oncomine, provide an invaluable tool to complement histopathologic examination and gene profiling to identify molecular signatures and potential biomarkers within a cancer type.
Similarly, proteomic datasets accessible through the Internet have been compiled. In a recent compendium report by Harsha and colleagues, a systematic compilation of messenger RNA (mRNA) and protein overexpression data of candidate biomarkers from the published literature in PDA was performed. A total of 2516 genes were included in the compendium report with 441 proteins reported to be overexpressed at the mRNA and protein levels. They further identified which of these proteins were membrane-associated or secreted molecules and expressed in pancreatic intraepithelial neoplasia (PanIN) lesions, identifying a subpopulation of proteins more likely to serve as useful early detection biomarkers. This bioinformatics approach is a valuable tool for the PDA research community to identify and validate the most promising individual or set of biomarkers. In fact, this approach is already being used by a consortium of investigators who are developing antibodies against the 60 most promising targets in a new research initiative funded by the Lustgarten Foundation for Pancreatic Cancer Research.
Diabetes mellitus as a biomarker
Most patients with PDA (75%–80%) will have new-onset diabetes mellitus (DM) as an early manifestation of the disease, often predating the diagnosis of invasive PDA by 1 to 2 years. Pancreatic cancer–associated DM may improve after surgical resection of the pancreatic tumor despite resection of a significant portion of pancreatic parenchyma, highlighting the fact that these tumors produce some type of diabetogenic substance. Animal data support this observation. In a study by Basso and colleagues, daily intraperitoneal injections of supernatant from the MIA PaCa-2 pancreatic cancer cell line into immunodeficient mice led to an increase in blood glucose measurements and impaired glucose tolerance as compared with controls injected with saline. The pathogenesis of impaired glycemic control in PDA seems to result from the presence of humoral factors that lead to peripheral insulin resistance and β-cell dysfunction. These humoral factors are yet to be identified.
Given the association of new-onset hyperglycemia and PDA, the use of new onset of diabetes as a screening modality toward early detection of PDA in this patient population may be beneficial. Early diagnosis of PDA in older patients (>50) with new-onset DM is limited by a low sensitivity of CT scanning for PDA. Two studies have examined the use of CA19-9 as an additional filtering biomarker in patients with new-onset DM, with a subsequent incorporation of invasive modalities, such as EUS, to further aid the diagnosis. Most patients diagnosed with PDA in this study were unresectable, thus limiting the utility of CA19-9 as an additional screening criterion for early pancreatic cancer detection in patients with new-onset DM. Other promising biomarkers to further filter those patients who need additional invasive testing are being explored. In a study by Basso and colleagues, S100A8 N-terminal peptide was identified in pancreatic cancers from diabetic patients but not in those from nondiabetic patients or in nonneoplastic tissues. In another study, Pfeffer and colleagues reported that connexin 26, a gap junction protein, was overexpressed in islets from patients with pancreatic cancer, and there was a correlation between connexin 26 mRNA levels and glucose levels. The findings from these 2 reports are interesting and warrant additional study. Overall, further studies have to be conducted to determine if new-onset diabetes, used either alone or in combination with other biomarkers, will be a useful approach for the early detection of PDA. Importantly, additional studies elucidating the pathogenesis of DM in this patient population also need to be done with a goal to identify biomarkers that could reliably distinguish PDA-associated DM from non-PDA–associated DM.
Tissue biomarkers to distinguish PDA from chronic pancreatitis
A hallmark feature of PDA is the production of an extensive fibrotic reaction in the gland surrounding the cancer cells. In the clinical arena, it may be difficult to differentiate PDA from other pathologic states of the pancreas, such as chronic pancreatitis, a benign process that also produces extensive fibrosis. A tissue-based biomarker approach would be useful in differentiating these disease states and allowing select patients to avoid unnecessary surgery. One such approach, the use of microRNA (miRNA), has produced promising results. miRNAs are small RNA molecules of approximately 22 nucleotides, which have recently been characterized as key regulators of mRNA expression within the human genome. miRNAs appear to be tissue specific and disease specific, with changes in miRNA correlating with certain disease states. Methods such as miRNA microarrays and quantitative real-time polymerase chain reaction may be used in miRNA detection in tissue samples. In several studies, miR-216 was identified as being specific for the pancreas. Other studies have determined that abnormal production of miR-196a and miR-217 can distinguish PDA samples from samples of healthy pancreas and chronic pancreatitis. A later study showed that increased production of miR-196a predicted a poorer survival in patients with PDA. These results suggest that the analysis of miRNA expression provides a complex and unique signature as a molecular biomarker useful in early diagnosis and predicting prognosis in this disease.
Current status of biomarker field in the early detection of PDA
Detection of PDA in its preinvasive state would greatly affect the treatment and prognosis of patients with this deadly malignancy. At present, suitable biomarkers have not been identified for the early detection of pancreatic cancer. Biomarker discovery for this disease is very much in its discovery phase. Multiple approaches have been developed, as described earlier, that hold promise for the identification of blood biomarkers. The biomarkers that have been identified to date do not possess the requisite sensitivity and specificity to have utility individually as a biomarker for the early detection of pancreatic cancer but ultimately may have utility within a panel of protein biomarkers. In addition, other emerging technologies, such as genetically engineered mouse models of pancreatic cancer, may have the utility to identify panels of serum biomarkers that can be further explored in human sera. To determine the utility of any promising protein biomarkers, the candidates have to be tested and validated by multiple independent studies using an adequately sized test and training set of sera samples from very early stage pancreatic cancer, a resource that does not currently exist. Development of such resources, including serum from patients with nonmalignant pancreatic lesions and prospective serum collection from individuals at high risk of being diagnosed with pancreatic cancer as well as serum from patients with other malignancies, is of critical need for the identification of biomarkers with utility for the early detection of pancreatic cancer. To date, serum or plasma collection has been primarily performed in individual laboratories, using heterogeneous sample collection methods. Currently, an effort is being made by the National Cancer Institute, through the Early Detection Research Network, to develop suitable serum resources for the discovery phase and the subsequent validation phase of biomarkers for the early detection of cancer. With the ultimate development of these standardized resources, it is expected that suitable biomarkers would be validated and would have utility for the early clinical detection of pancreatic cancer within the next 5 to 10 years.
Signaling mechanisms in pancreatic cancer
PDAs are poorly responsive to most chemotherapeutic agents and also to radiation therapy. The cell of origin of PDA is still in debate; however, the most accepted model of progression of PDA involves neoplastic progression of precursor lesions of the pancreas classified as PanIN. In general, PDAs are known to display extensive genomic instability and aneuploidy.
The vast majority of PDAs are characterized by a mutation in codon 12 of K- ras that results in a constitutively active form of the protein. This mutation is also detected in PanIN lesions and therefore has been considered one of the early events in pancreatic carcinogenesis. The importance of K- ras in the initiation of pancreatic cancer has been firmly established in studies in genetically engineered mouse models. Expression of the mutant forms of K- ras , either K- ras G12D or K- ras G12V, in the pancreatic epithelium results in the development of PanIN lesions that eventually progress to PDAs. However, the long latency of disease in K- ras mutant animals underscores the need for additional genetic changes. Studies in mouse models have shown that loss of function of tumor suppressor genes, such as INK4A/ARF and p53 , leads to anticipated onset of PanIN lesions and faster progression to adenocarcinomas. Those same tumor suppressor genes are often lost or mutated in human tumors, underscoring their role in preventing oncogenic changes.
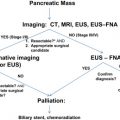
Another key feature of human pancreatic cancer is the inappropriate activation of embryonic signaling pathways, such as Notch, hedgehog, and Wnt ( Fig. 1 ). In particular, Notch and hedgehog have been shown to be associated with close to 100% of human pancreatic cancers in a recent comprehensive analysis of genomic alterations. The next section discusses the current understanding of the contribution of these embryonic pathways to PDA.
The role of Notch signaling in pancreatic development has been widely studied. When Notch signaling is activated in the developing pancreas by overexpression of the Notch intracellular domain, differentiation of endocrine and exocrine lineages is impaired and pancreatic progenitors remain trapped in an undifferentiated state. On the other hand, Notch pathway inactivation early in the development using a conditional RBPJ knockout causes premature differentiation of pancreatic progenitors into endocrine cells and impaired exocrine differentiation. However, late embryonic and postnatal development of the pancreas is not affected by Notch pathway inactivation. Combined inactivation of Notch 1 and Notch 2 during early pancreatic development causes only mild developmental phenotypes, leaving the possibility that the RBPJ knockout phenotype depends, at least in part, on Notch-independent functions of this transcription factor. In the adult pancreas, Notch signaling activity is restricted to the centroacinar cell compartment.
A comprehensive study of human pancreatic cancer has provided ample evidence that the Notch signaling pathway is reactivated in pancreatic cancer and pancreatic cancer precursors. More recently, Notch inhibition in mice using gamma-secretase inhibitors (GSIs) has been shown to inhibit tumor initiation and maintenance in mice. Conversely, constitutive activation of Notch in the pancreatic epithelial cells synergizes with K- ras in driving PanIN formation.
The first evidence for the importance of hedgehog signaling in pancreatic cancer was the observation that PanIN lesions and invasive PDAs express the Sonic Hedgehog (Shh) ligand. This finding was somewhat surprising because Shh expression has not been found in normal embryonic or adult pancreatic tissue, suggesting that the transcriptional profile of pancreatic cells is aberrant during tumor formation. Several follow-up studies have confirmed the importance of hedgehog signaling in pancreatic cancer and have led to a deeper understanding of its mechanism of action in this disease.
Hedgehog ligand overexpression by the tumor cells has been shown to activate the hedgehog pathway in a paracrine manner in the surrounding fibroblasts and potentially mediate fibroblast expansion, leading to the accumulation of a desmoplastic stroma, which is a common characteristic of pancreatic cancer. Although ligand-mediated hedgehog signaling pathway does not appear to be active in the tumor cells themselves, GLI1, one of the transcription factors acting downstream of the hedgehog pathway, is expressed in the epithelial cells and promotes their growth. Several studies have hypothesized a “noncanonical” mode of GLI activation. Moreover, activation of GLI in an epithelial-specific manner synergizes with mutant K- ras in accelerating PanIN formation.
The role of Wnt signaling in pancreatic cancer has been controversial. On one hand, mutations in components of the pathway have not been associated with pancreatic cancer, and several early studies discounted a role for this signaling pathway in the disease. On the other hand, studies in different mouse models and in human samples have shown that the pathway is indeed active and that it is important for tumor maintenance. A potential mechanism for the stabilization of β-catenin in pancreatic cancer implicates ataxia-telangiectasia group D complementing (ATDC) gene as a key player in pancreatic tumorigenesis. The Wnt signaling pathway is activated downstream of hedgehog signaling in the late stage of PanIN formation and at lower levels than tumors in which activating mutations in the β-catenin signaling pathway are found (comparable with levels found in normal tissues but not with other, traditionally Wnt-linked, tumors). In genetically engineered mouse models, high-level activation of the Wnt pathway in the pancreas leads to profound developmental alterations. On the other hand, activation in the adult mouse pancreas leads to the development of solid pseudopapillary neoplasms of the pancreas, and if it is combined with K- ras mutations, it leads to the formation of acinar tumors that do not follow PanIN progression and do not resemble PDA.
The importance of Wnt signaling in human PDAs is beginning to be unraveled. Pasca di Magliano and colleagues identified 65% of human PDAs to have increased cytoplasmic expression of Wnt. Regulation of Wnt signaling is complex. Wang and colleagues showed a regulatory role for ATDC in Wnt/β-catenin signaling. ATDC is overexpressed in PDA as compared with nonneoplastic controls based on affymetric gene analysis data. Thus ATDC/Wnt signaling may be an important therapeutic target for the treatment of PDA.
Clinical Aspects
Given that pancreatic cancer is resistant to conventional cytotoxic chemotherapy, a better understanding of molecular signaling pathways has led to the development of novel therapeutics for the treatment of this disease. Several small-molecule inhibitors of hedgehog signaling have completed preclinical testing with evidence of efficacy in xenograft models. Currently, these agents are in early-phase clinical trial testing. Several Notch inhibitors have also been evaluated. GSIs block a critical event in Notch signaling and have emerged as effective Notch pathway inhibitors that have been recently implemented in human clinical trials to target several types of malignancies, with a recent trial initiated to target breast cancer. Similarly, several inhibitors of Wnt/β-catenin signaling are being evaluated in early-phase clinical trial testing. Incorporation of these and other novel therapeutic targeted agents will likely play a critical role in the management of this disease in the near future.
Mouse models in pancreatic cancer research
Given the dismal outcome of pancreatic cancer in patients, there is a dire need for new therapeutic options. Mouse models of cancer have greatly contributed to advances in our knowledge of tumor biology and have been used for preclinical validation of new drugs. Different cancer models have been used to study pancreatic cancer. In subcutaneous xenograft models, human pancreatic cancer cell lines are implanted in immunocompromised mice. Subcutaneous models are the easiest to set up, requiring only host animals and cell lines in culture. However, they have significant limitations. The human tumor cell lines that are commonly used in those models have often been cultured for a long time, and they may have undergone clonal selection and may possess culture-induced artifacts. Moreover, the subcutaneous space does not mimic the normal environment surrounding pancreatic cancer; finally, the models necessitate the use of mice with a compromised immune system. For all of these reasons, this type of xenograft model has been defined as “animal culture.” Nevertheless, such xenograft models have strongly contributed to some of the advances in basic pancreatic cancer research.
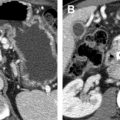
A different transplantation model is represented by the orthotopic xenograft, which implies the transfer of human tumor cells into the mouse pancreas. Although these models lack an intact microenvironment, they do place the tumor cells in the pancreas and therefore allow them to interact with pancreatic fibroblasts and other cell types that might be important for tumor growth. Importantly, orthotopically transplanted tumors can metastasize. The use of primary human tumor cells, rather than established cell lines, in orthotopic transplantation models is probably the closest one can get to studying how a specific patient’s tumor responds to different treatment regimens. Moreover, they can provide a representation of the variability found in human tumors and might be useful to determine whether the human malignancies can be subdivided into different subsets that are more likely to respond to a specific treatment.
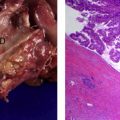
Arguably, the tumor model that most readily lends itself to studying basic biologic questions relevant to the development of pancreatic cancer is the genetically engineered mouse model (GEMM). Several attempts at developing genetic mouse models of pancreatic cancer have been based on either the expression of a viral oncogene in the pancreas or the expression of a mutant form of K- ras in either acinar or ductal cells. Those models failed to recapitulate the PanIN to PDA progression typical of the human disease and often produced no invasive tumor or tumors that did not resemble human PDA (Hezel and colleagues have provided a comprehensive review of those models). Dramatic progress in the ability to mimic the human disease has been made through the use of a conditional model of K- ras activation, whereby the mutant K- ras G12D is expressed on the cyclization recombination (Cre) of the endogenous K- ras locus. Pancreas-specific activation of the mutant K- ras allele can be obtained using Pdx1-cre or p48cre. The resulting double-mutant mouse, known as the KC mouse, develops PanIN lesions that are indistinguishable from their human counterpart and occasionally progress to metastatic adenocarcinoma. The KC mouse has been used to understand the role of different tumor suppressor genes in the development of pancreatic cancer. Conditional loss of the INK4A/ARF locus leads to anticipated development of PanIN lesions and metastatic adenocarcinoma. The Pdx1-cre; LSL-K- ras G12D; Trp53 R172H mouse, or KPC, has a mutant allele of the p53 tumor suppressor gene and develops metastatic adenocarcinoma with a 100% penetrance and high genomic instability, a characteristic of the human disease ( Fig. 2 ). The tumor characteristics observed in these models are different, depending on the specific tumor suppressor gene involved. It will be of great interest to determine whether these tumor suppressor mutations confer differences in histology and/or metastatic behavior. PanINs are the most common precursor lesions for pancreatic cancer. However, invasive adenocarcinoma can also arise from different benign lesions, such as intraductal papillary mucinous neoplasms (IPMNs) and mucinous cystic neoplasms (MCNs). The development of IPMN and MCN lesions can be modeled in the mouse. Loss of SMAD4 in the KC mouse leads to IPMNs or MCNs that progress to invasive adenocarcinoma.