Step 1
Surgical Anatomy
Thyroid
- ♦
The thyroid consists of two lobes joined by an isthmus. The normal weight of the adult gland is approximately 20 grams. Each lobe has a conical shape and measures approximately 5 × 3 × 2 cm. Normal thyroid is dark wine red in color, soft, and covered by a thin capsule.
- ♦
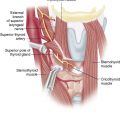
The gland is situated in the lower part of the neck, with the isthmus crossing the trachea at the level of the second and third tracheal rings. The posterior suspensory ligament (ligament of Berry) attaches the gland to this structure. It is covered by the strap muscles (sternohyoid and sternothyroid muscles), joined in the midline by the cervical linea alba (anterior fascia cervicalis).
- ▴
The medial part of each lobe lies over the larynx and the trachea. The esophagus is situated on the posteromedial aspect of the thyroid lobe, and the recurrent laryngeal nerve runs more or less vertically on each side along the tracheoesophageal groove.
- ▴
The superior poles are in contact with the inferior constrictor muscle and the cricothyroid muscle.
- ▴
The inferior pole usually reaches the fourth or fifth tracheal ring. Often, a residual of the thyroglossal duct extends cranially from the isthmus and is variably developed (pyramidal lobe).
- ▴
- ♦
The gland receives its arterial blood supply from the superior and inferior thyroid arteries. The superior thyroid artery originates from the external carotid artery. It descends along the surface of the inferior constrictor muscle of the pharynx and enters the upper pole of the thyroid on its anterosuperior surface. In approximately 10% of cases a branch of this artery feeds the superior parathyroid gland. The external branch of the superior laryngeal nerve runs very close to the branches of the superior thyroid artery, but this relationship is quite variable.
- ♦
The inferior thyroid artery is a branch of the thyrocervical trunk; it passes superiorly behind the common carotid artery and jugular vein, toward the cricoid cartilage. At the level of the gland the artery loops downward and medially and enters the middle aspect of the lobe. It divides into several terminal branches. This artery and its branches have a very close relationship with the inferior laryngeal nerve. A branch of the inferior thyroid artery usually supplies the inferior parathyroid gland; in most cases the inferior thyroid artery also supplies the superior parathyroid gland.
- ♦
The venous drainage is more variable than the arterial supply. The superior thyroid vein is closely related to the superior thyroid artery and drains into the internal jugular vein. Middle thyroid veins vary in number and pass from the lateral border of the lobe into the internal jugular vein.
Lymphatic Drainage
- ♦
The lymphatic drainage of the thyroid is extensive. The surgeon must consider two main zones of lymphatic drainage: the central compartment (periglandular space) and the lateral compartment. The carotid sheath separates the two compartments.
- ♦
The central compartment includes the prelaryngeal, pretracheal, and paratracheal-esophageal groups. The anterior boundary of this compartment is made up of strap muscles, but sometimes lymph node metastases may be found on the cricothyroid muscle just above the isthmus (Delphian nodes).
Laryngeal Nerves
- ♦
The external branch of the superior laryngeal nerve has a close relationship with the superior thyroid vessels and the superior thyroid pole. The superior laryngeal nerve arises from the vagus nerve and descends lying on the middle constrictor muscles. At this level it divides into external and internal branches.
- ▴
The external branch continues inferiorly and innervates the cricothyroid muscle, which produces tension of the vocal cord; thus, injury to this nerve may compromise the production of high-pitched voice sounds.
- ▴
In 6% to 18% of cases the external branch of the superior laryngeal nerve runs with or around the superior thyroid artery or its branches and is thus susceptible to injury during surgical dissection.
- ▴
In almost 20% of cases it is not situated in the surgically accessible area near the superior pole vessels of the thyroid gland and cannot be visualized during conventional surgery.
- ▴
- ♦
The recurrent laryngeal nerves arise from the vagus nerve and supply all muscles of the larynx except the cricothyroid muscle. On the right side the nerve passes behind the subclavian artery, recurring upward toward the larynx. On the left side the nerve passes around the ligamentum arteriosum. On both sides, the nerve runs cranially and medially, toward the cricoid cartilage where it enters the larynx. The recurrent laryngeal nerve is often not a single strand but may have several branches (to the esophagus, trachea, and thyroid) and anastomoses with other nerves (superior laryngeal nerve, sympathetic system, and contralateral nerve). The relationship between the inferior thyroid artery and the inferior laryngeal nerve is variable.
Parathyroids
- ♦
The normal parathyroid glands are soft, pliable, and compact. The majority are spherical or bean-shaped; a few are elongated, bilobed, or even flattened and multilobed. Their color ranges from reddish brown in the well-vascularized gland to pale yellow in a gland with high fat content. The average gland weighs approximately 40 mg, with dimensions of approximately 5 × 3 × 1 mm. The parathyroids are frequently found in fat or in the thymus, from which they are easily separated.
- ♦
Almost all individuals have at least four parathyroid glands. Supernumerary glands are found in 5% to 15% of individuals; the most common sites (two thirds) are within the thymus or thyrothymic ligament. Approximately one third are located close to the thyroid between two normally situated parathyroids.
- ▴
Occasionally there may be multiple supernumerary glands. This is especially significant in pathologic states in which there is an underlying genetic disorder, such as multiple endocrine neoplasia type 1, or an ongoing stimulatory influence, as seen in secondary hyperparathyroidism associated with renal failure.
- ▴
In some individuals a fifth gland is the result of splitting of a normal or bilobed gland during development. The two components are close together, often in direct contact with each other.
- ▴
- ♦
The superior parathyroids are fairly constant in position because of their simple restricted embryologic descent. More than 80% are located in an area 2 cm in diameter centered 1 cm above the intersection of the inferior thyroid artery and the recurrent laryngeal nerve. Superior gland ectopia is less common than that of the inferior gland, although a few glands are more posterior in position. During their descent in the tracheoesophageal groove the superior glands tend to move posteriorly; the further caudal their migration, the more posterior their ultimate location.
- ▴
Retropharyngeal or retroesophageal locations have been described, but when a superior gland is found far inferior in the posterior mediastinum, alongside the esophagus, it is usually the result of migration of an enlarged adenomatous gland brought about by the effects of esophageal peristalsis and deglutition. Occasionally, superior glands may be found on the posterior aspect of the thyroid upper pole or in relation to the superior vascular pedicle of the thyroid. On even rarer occasions they may be located superior to the thyroid upper pole or within the thyroid gland.
- ▴
- ♦
Because of their longer embryologic migration the inferior parathyroids are more likely to be positioned at ectopic sites. During their descent they tend to move anteriorly. The majority of glands are located in relation to the posterior or inferior ventral aspect of the lower pole of the thyroid. Approximately 25% lie at a lower level, within the thyrothymic ligament or within the posterior cervical thymic horns. Approximately 4% to 5% are in the anterior mediastinum within the retrosternal thymus near the innominate vein and ascending aorta. A few will be outside the thymus and related to the aortic arch and the origin of the great vessels. An even lower position of the inferior parathyroid gland is in the aortopulmonary window or in contact with the pleura or pericardium below the thymus. Other ectopic glands can be located medial to or within the carotid sheath or even near the carotid bulb at the level of the mandible.
- ▴
The inferior parathyroid gland may be truly intrathyroidal within the lower pole of the thyroid in 1% to 3% of individuals. Symmetry of position of the superior glands occurs in 80%, of the inferior glands in 70%, and of all four glands in 60%.
- ▴
- ♦
The vascular supply of the parathyroid glands has been carefully investigated. The main arterial input is of end artery type, with approximately one third of glands supplied by two or more arterial branches. Although the principal parathyroid blood supply is derived from the inferior thyroid artery, a significant proportion of superior glands will receive their main blood supply from either the posterior branch of the superior thyroid artery or an anastomotic loop that this vessel makes with the inferior thyroid artery. A small component of the parathyroid blood supply also is from the thyroid capsular vessels.
- ♦
Venous drainage accompanies the venous drainage of the thyroid, including capsular vessels and the larger main thyroid veins.
Step 2
Preoperative Considerations
Indications for MIVAP
- ♦
Generally the ideal patient for minimally invasive video-assisted parathyroidectomy (MIVAP) is one with sporadic primary hyperparathyroidism and a single, well-localized adenoma in a neck that has not had a previous operation. There is debate about the percentage of patients who are eligible for minimally invasive parathyroidectomy; this depends on the selection criteria used by the surgeon. In our experience these criteria have been modified by the experience acquired during the development of our technique and the continuing improvement of surgical instruments.
- ♦
Contraindications may be absolute or relative and are shown in Table 9-1 .
TABLE 9-1
Absolute and Relative Contraindications to MIVAP
RELATIVE CONTRAINDICATIONS
ABSOLUTE CONTRAINDICATIONS
Adenomas larger than 3 cm *
Large goiters
Lack of preoperative localization **
Recurrent disease
Neck surgery required on the opposite side of the suspected adenoma †
Extensive previous neck surgery
Previous neck irradiation or small thyroid nodules ‡
MEN and familial PHPT Parathyroid carcinoma
MEN, multiple endocrine neoplasma; PHPT, primary hyperparathyroidism.
* Depending upon their shape, even larger adenomas can be removed.
** A bilateral exploration can be achieved from the central incision.
† A lateral access can be used.
- ♦
A careful selection of patients is important to achieve an excellent outcome and to keep the conversion rate low. Although these criteria are presumably shared by the majority of surgeons performing minimally invasive parathyroidectomy, the percentage of patients eligible for this surgery varies greatly, from as little as 25% to as much as 66%.
Indications for MIVAT
- ♦
Careful selection of patients undergoing minimally invasive video-assisted thyroidectomy (MIVAT) is the only guarantee of a good outcome. Only a minority of patients are eligible for a video-assisted approach to the thyroid.
- ▴
An important limit is the volume of both the nodule and the gland. The lobe has to be removed without disrupting its capsule because accurate histologic evaluation is necessary for the nodules that are suspected for malignancy (either follicular or papillary).
- ▴
Other limits of this technique include the presence of adhesions, which can make dissection difficult. Adhesions can be due to previous surgery or thyroiditis, which can be suspected by typical ultrasound findings and can be confirmed by thyroid antibodies.
- ▴
- ♦
General indications for MIVAT include the following:
- ▴
Thyroid nodule smaller than 30 mm on the largest diameter
- ▴
Thyroid gland volume smaller than 20 mL, as estimated by ultrasound
- ▴
No history of thyroiditis
- ▴
No previous neck surgery or irradiation.
- ▴
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree