Meniscal Structure, Function, Repair, and Replacement
Mark C. Drakos
Answorth A. Allen
The menisci are triangular wedges of fibrocartilage located on the medial and lateral aspects of the knee joint. They function to absorb shock and dissipate load between the distal femur and the proximal tibia. The knee may encounter forces two to four times body weight while walking and almost double that while running. Due to the high shear stresses that arise across the knee joint during activity, injury to the menisci is quite common. Epidemiologic studies indicate an annual incidence of meniscal tears of 60 to 70 per 100,000 people. In addition, these lesions are highly associated with both chronic and acute anterior cruciate ligament (ACL) tears as well as tibial plateau fractures. Initial treatment of these lesions is usually conservative. However, the natural history of meniscal tears depends on the specific location and characteristics of the tear within the meniscus. Due to the relatively avascular nature of the tissue, central injuries will often not heal. Repair and regeneration of normal cartilage is an area of increased interest in the orthopaedic community and a popular area for research. The focus of this chapter will be the anatomy, structure, and function of the menisci and how this pertains to potential treatments, including regeneration, repair, and replacement.
Gross Anatomy
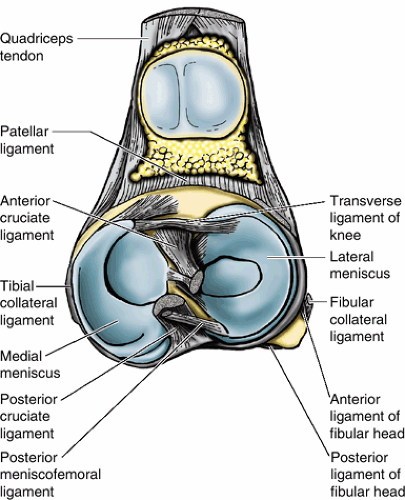
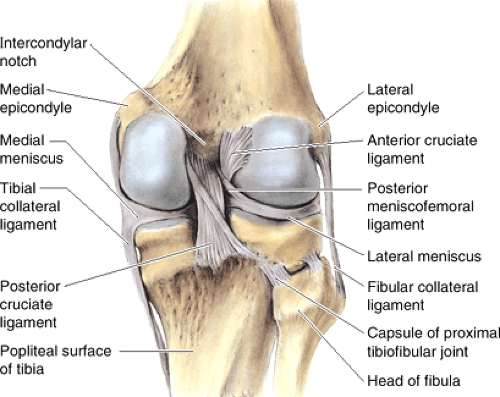
The menisci of the knee joint were originally considered to be “functionless remnants of intra-articular leg muscles.” We now know that these wedges of fibrocartilage play a critical role in normal knee kinematics. There are medial and lateral menisci, which are each divided into thirds: anterior horn, middle, and posterior horn. The anterior and posterior horns of each meniscus attach to intercondylar fossa (Figs. 22-1 and 22-2).
Medial Meniscus
C-shaped
∼3.5 cm in length
Greater diameter than the lateral meniscus
Posterior horn wider than anterior horn
Coronary ligaments attach the meniscus to capsule.
Deep bundle of the medial collateral ligament (MCL) is condensation of capsule that attaches to the meniscus at its midportion.
Transverse meniscal ligament connects the anterior horns of the medial and lateral meniscus, but the attachment to anterior horn of the medial meniscus can be variable.
Multiple attachments to medial meniscus are postulated to result in less mobility, to which the higher incidence of medial meniscal tears (three times as common as lateral meniscus) has been attributed.
Lateral Meniscus
Semicircular
Covers larger tibial surface area than medial meniscus
Anterior and posterior horns are the same width.
More mobile, weaker coronary ligament than medial meniscus
No attachment to capsule in area of popliteal hiatus
Meniscofemoral ligaments attach posterior horn of lateral meniscus to medial femoral condyle and posterior cruciate ligament (PCL).
Ligament of Humphrey is anterior to PCL.
Ligament of Wrisberg is posterior to PCL.
One or the other may be present, but not both, in 70% to 90%.
Microscopic Anatomy and Histology
The meniscus is composed of a complex network of proteins, chondrocytes, water, and other matrix components, each of which plays a role in the biomechanics of the meniscus.
Meniscal Composition
Predominant protein is collagen, which contributes 60% to 70% of the dry weight.
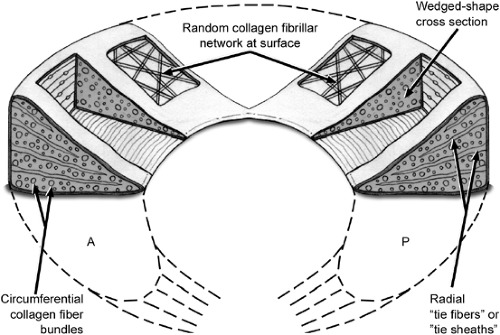
Specialized orientation to respond to large stresses (Fig. 22-3)
Peripheral fibers: arranged circumferentially following the contour of the meniscus
Woven in a mesh fashion superficially
Thicker and oriented more parallel at deeper layers
Radially oriented fibers: interposed fibers that act as “ties” to prevent longitudinal tears and provide structural stability. In addition, this arrangement helps the meniscus to function as a “wet sponge” (see below).
Primarily composed of type I collagen (90% of total collagen)
While mature cartilage has no progenitor cells, immature cartilage has a stem cell population, and it has been hypothesized that the stem cells
differentiate into chondrocytes, which secrete type I collagen due to the tensile loads on the menisci.
Less common collagen components: types II, III, V, VI
Larger proportion of type II collagen in the central, inner regions
Remaining dry weight of the meniscus comes from other proteins, including proteoglycans and elastin.
Interaction of collagen and proteoglycans (“wet sponge” function): Aggregan, a common proteoglycan, combines with glycosaminoglycans to form a macromolecule that binds positively charged sodium ions. These ions then associate with the negative charge on the water molecules by hydrogen bonding. When a force that spreads the collagen fibrils apart is applied, these bonds are broken and water exudes from the tissue. When the force is relaxed, the water is drawn back into the cartilage by the electrostatic charge of the glycosaminoglycans. Thus, force is dissipated through the cyclic disruption and reformation of the hydrogen bonds with the glycosaminoglycans.
Meniscal water content: 65% to 75%
Cellular component: fibrochondrocytes
Terminology based on microscopic appearance as well as the fibrocartilaginous matrix that they synthesize
Secrete collagen, proteoglycans, and enzymes for cartilage metabolism
Differing morphologies based upon depth
Superficial zone: fusiform cells
Remainder: more rounded
Predominately anaerobic metabolism
Few mitochondria
Prevalent Golgi complexes and endoplasmic reticulum
Vascular Anatomy
The vascularity of the menisci decreases precipitously after birth to assume its adult, relatively avascular composition by 10 years of age (Table 22-1). In the adult, only the peripheral third carries meaningful blood supply to either meniscus. The menisci derive their blood supply from the superior and inferior branches of the medial and lateral geniculate arteries as well as the middle geniculate artery. These vessels form a perimeniscal capillary plexus.
A reflection of vascular synovial tissue gives a limited vascular supply to the peripheral 1 to 3 mm of the menisci.
In the adult form, Arnoczky and Warren demonstrated that the peripheral 10% to 25% of the lateral meniscus is vascularized.
The peripheral 10% to 30% of the medial meniscus is vascularized.
Red-and-white classification system
Divides the meniscus into an inner, middle, and peripheral third (Figs. 22-4 and 22-5)
Inner third = white/white zone (poor healing potential for tears)
Middle third = red/white zone (intermediate healing potential)
Table 22-1 Vascularity of the Menisci
Age
Vascularity
Birth
Entire meniscus
9 months old
Peripheral two thirds
10 years old to adult
Peripheral third
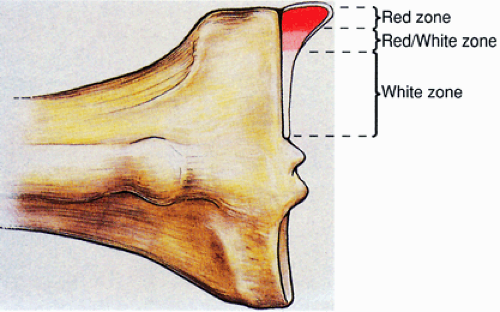
Figure 22-4 Distribution of healing zones within the meniscus. (From Miller MD, Warner JJP, Harner CD. Meniscal repair. In Fu FH, Harner CD, Vince KG. Knee Surgery. Baltimore: Williams & Wilkins, 1994.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access