VII.C.001 Burkitt Lymphoma
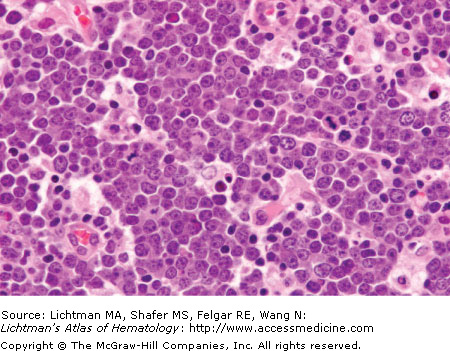
VII.C.002 Burkitt Lymphoma
VII.C.003 Burkitt Lymphoma
VII.C.004 Burkitt Lymphoma
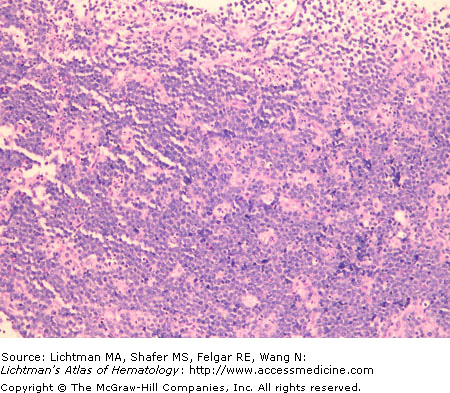
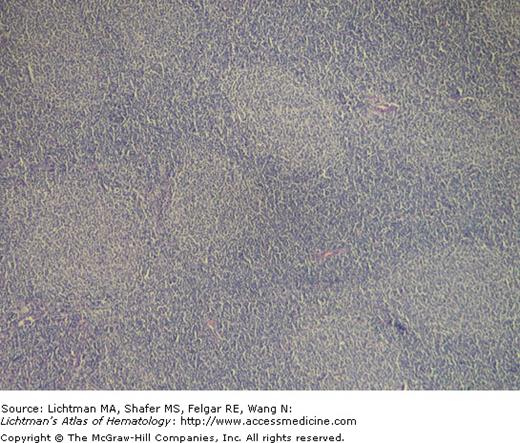
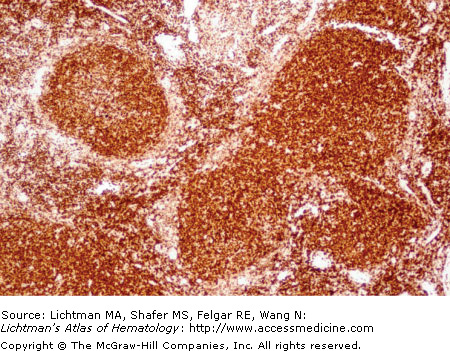
VII.C.004
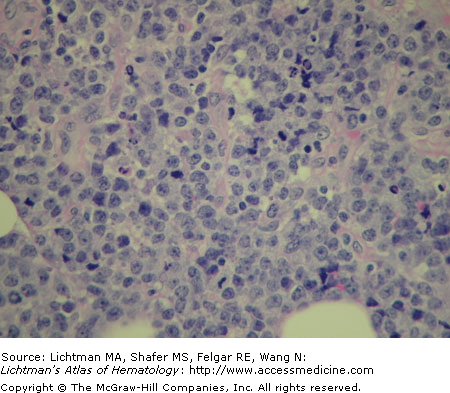
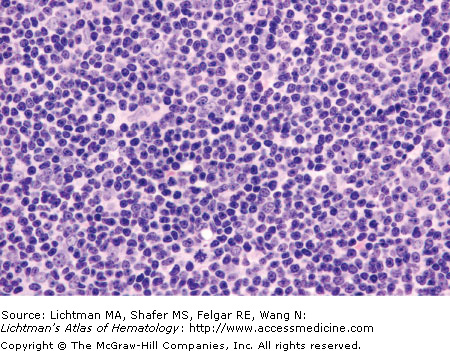
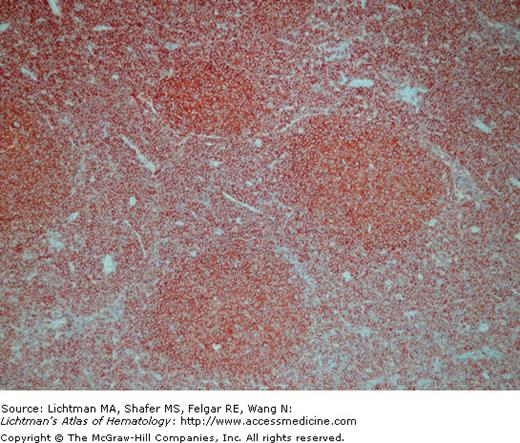
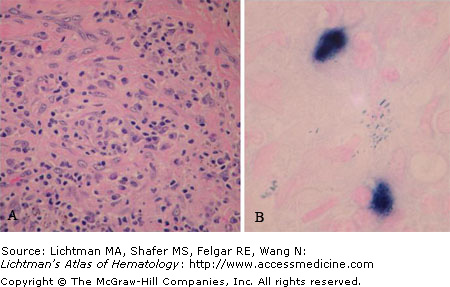
Burkitt lymphoma. Lymph node biopsy. Low power view. Note areas of clearing that impart the so-called “starry sky” appearance. These areas represent tingible-body macrophages within the tumor that are recruited to phagocytize cellular debris. A similar appearance may also be seen in other lymphomas that have a high proliferative rate.
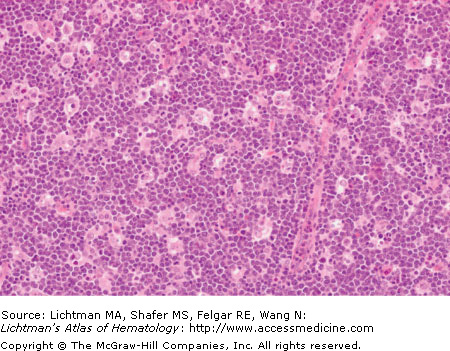
VII.C.005 Burkitt Lymphoma
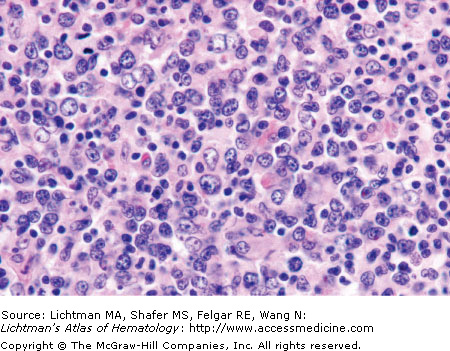
VII.C.005
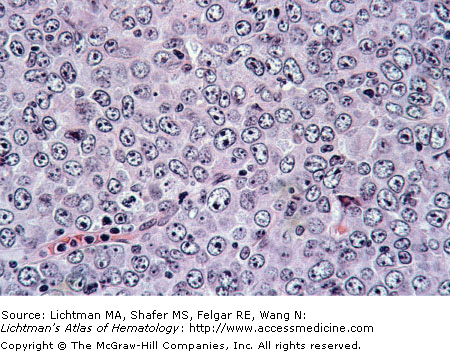
Burkitt lymphoma. Lymph node. Biopsy. Higher power view. Individual tumor cells have a high nuclear: cytoplasmic ratio, round nuclear contours, and small, barely perceptible nucleoli (sometimes called “inconspicuous” nucleoli). These overall features are often referred to as a “small non-cleaved” cell or “small transformed” cell cytology.
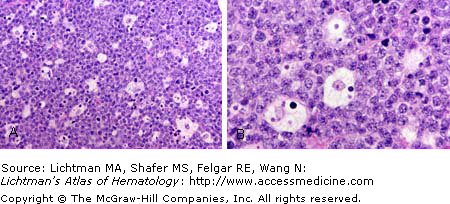
VII.C.006 Burkitt Lymphoma
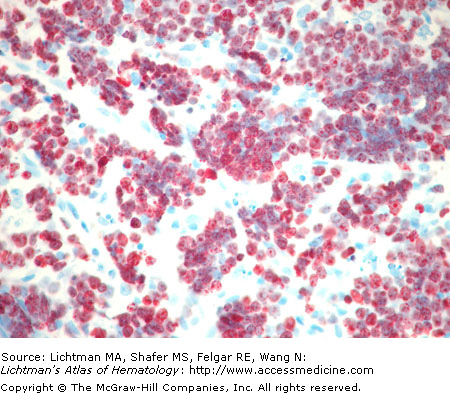
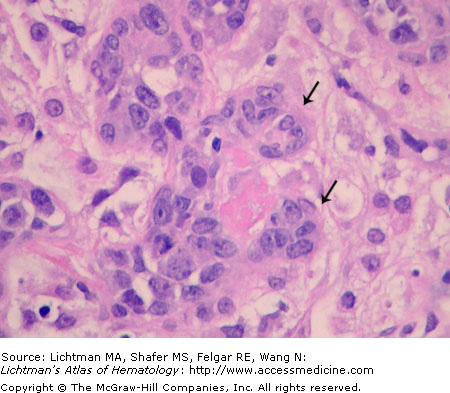
VII.C.006
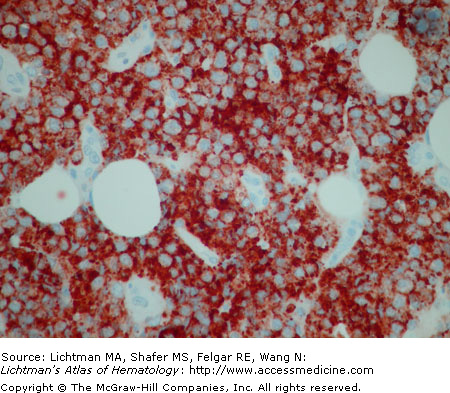
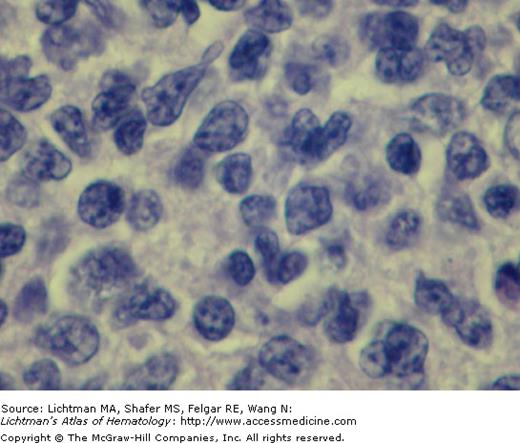
Burkitt lymphoma. Lymph node biopsy. (A) Lower power view showing diffuse replacement of nodal tissue with Burkitt lymphoblasts with classical interspersed macrophages presenting a starry sky appearance. (B) Higher power view. Burkitt lymphoblasts with prominent nucleoli. Interspersed macrophages with ingested cellular debris. Relative increase in mitotic figures.
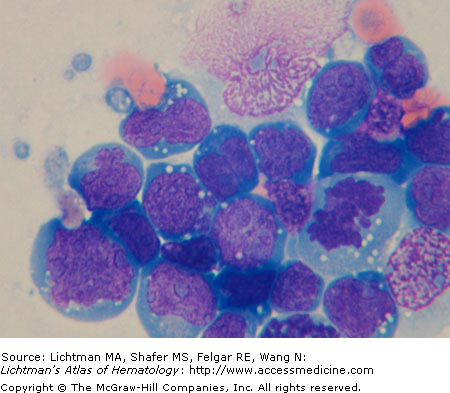
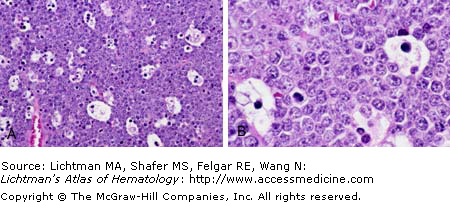
VII.C.007 Burkitt Lymphoma
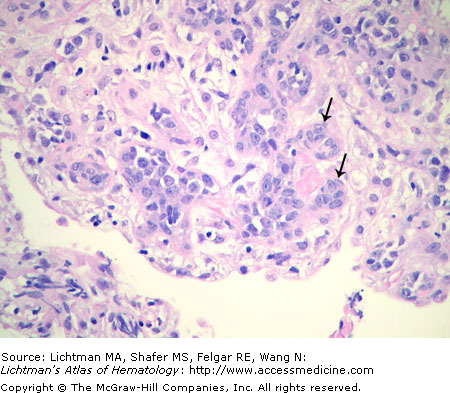
VII.C.007
Burkitt lymphoma. Lymph node biopsy. (A) Lower power view showing diffuse replacement of nodal tissue with Burkitt lymphoblasts with classical interspersed macrophages presenting a starry sky appearance. (B) Higher power view. Burkitt lymphoblasts with prominent nucleoli. Interspersed macrophages with ingested cellular debris.
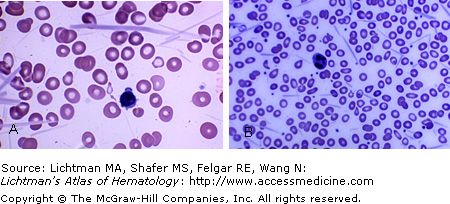
VII.C.008 Cryoglobulinemia
VII.C.009 Cryocrystalglobulinemia
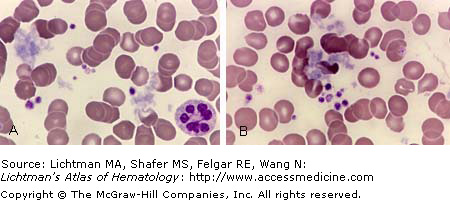
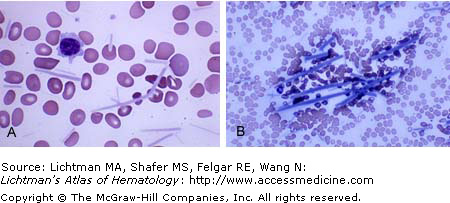
VII.C.009
Cryocrystalglobulinemia. Blood films. Patient with circulating immunoglobulin that crystallized at room temperature. (A) Higher power image of blood film prepared at room temperature with precipitated crystals, ranging from about 5 to 60μM in length. (B) Lower power blood film displaying precipitated crystals. No crystals were evident at 37oC. The white count fluctuated unpredictably based on the temperature of blood during white cell counting. At temperatures closer to room temperature the crystals were being counted as white cells by the electronic particle counter. This type of phenomenon is less of a problem with more modern analyzers that rely on light scatter to identify and enumerate blood cells than on older analyzers that used electrical impedance (Coulter principle) to detect blood cells.
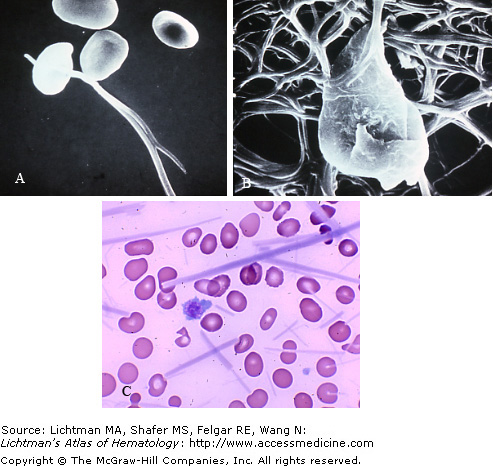
VII.C.010 Cryocrystalglobulinemia
VII.C.010
Cryocrystalglobulinemia. Blood films. Patient with circulating immunoglobulin that crystallized at room temperature. (A) Blood film prepared at room temperature with precipitated crystals. (B) Precipitated crystals. Note very long crystals approaching 100μM in length. No crystals were evident at 37oC. The white count fluctuated unpredictably based on the temperature of blood during white cell counting. At temperatures closer to room temperature the crystals were being counted as white cells by the electronic particle counter. This phenomenon is less of a problem with more modern analyzers that rely on light scatter to identify and enumerate blood cells than on older analyzers that used electrical impedance (Coulter principle) to detect blood cells.
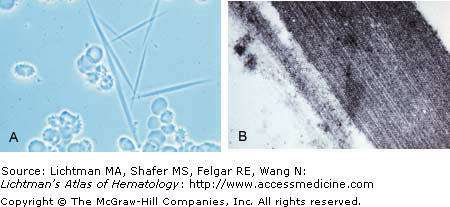
VII.C.011 Cryocrystalglobulinemia
VII.C.012 Cryocrystalglobulinemia. Scanning Electron Micrographs
VII.C.013 Diffuse Large B-Cell Lymphoma
VII.C.013
Diffuse large B-cell lymphoma. H&E stained histologic section shows a diffuse infiltrate of neoplastic centroblasts with a high nuclear:cytoplasmic ratio, irregular nuclear contours, and prominent nucleoli. In addition, mitotic figures and apoptotic nuclei are seen, indicating a high proliferative rate in this tumor.
VII.C.014 Diffuse Large B-Cell Lymphoma
VII.C.015 Diffuse Large B-Cell Lymphoma
VII.C.016 Diffuse Large B-Cell Lymphoma
VII.C.017 Extranodal Marginal Cell Lymphoma of Mucosa-Associated Lymphoid (MALT) Tissue Marginal Zone Lymphoma
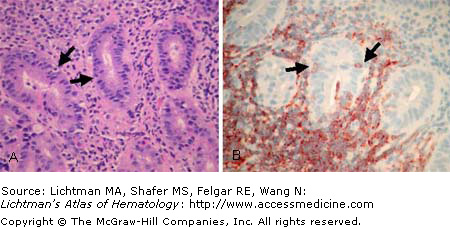
VII.C.017
Extranodal marginal cell lymphoma of mucosa-associated lymphoid tissue marginal zone lymphoma. Endoscopic gastric biopsy showing MALT lymphoma. (A) Small lymphocytes in gastric mucosa, a site normally devoid of lymphocytic cells and with no native lymphoid follicles except in states of chronic inflammation. Lymphocytes are also seen invading the epithelium (arrows). (B) CD20 immunostain confirms that the infiltrating lymphocytes are CD20+ B cells (arrows). PCR demonstrated a clonal rearrangement of the immunoglobulin heavy chain locus (clonal B-cell population). This subtype of lymphoma is linked to chronic gastritis caused by Helicobacter pylori infection, and these organisms can often be seen on tissue biopsy when in the chronic inflammatory stage. In this case, as in most cases of MALT lymphoma, no H pylori were seen histologically.
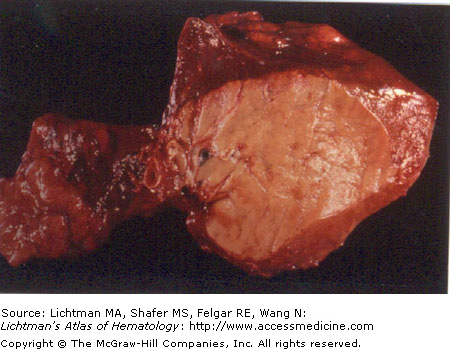
VII.C.018 Extranodal Marginal Cell Lymphoma of Mucosa-Associated Lymphoid Tissue (MALT)
VII.C.018
Extranodal marginal cell lymphoma of mucosa-associated lymphoid tissue (MALT). Pulmonary lobe resection showing typical “fish flesh” appearance of lymphoma. In this case, the tumor is an extranodal marginal zone lymphoma of extranodal mucosa associated lymphoid tissue, so-called MALT lymphoma.
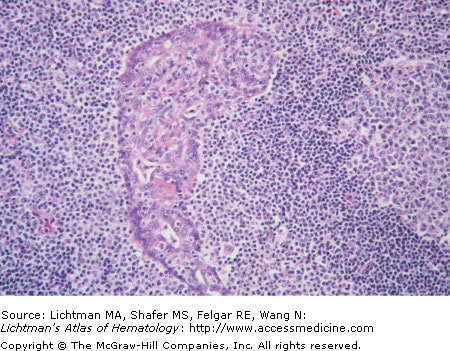
VII.C.019 Extranodal Marginal Cell Lymphoma of Mucosa-Associated Lymphoid Tissue (MALT) Marginal Zone Lymphoma
VII.C.019
Extranodal marginal cell lymphoma of mucosa-associated lymphoid tissue (MALT) marginal zone lymphoma. Section of lung shown in VII.C.046 showing lymphoepithelial lesion characteristic of MALT lymphoma. Epithelial cell layer (arrow) with infiltrate of small lymphocytes.
VII.C.020 Extranodal Marginal Cell Lymphoma of Mucosa-Associated Lymphoid Tissue (MALT) Marginal Zone Lymphoma
VII.C.021 Follicular Lymphoma
VII.C.022 Follicular Lymphoma
VII.C.023 Follicular Lymphoma
VII.C.024 Follicular Lymphoma
VII.C.024
Follicular lymphoma. Lymph node biopsy. High power view of the central portion of a neoplastic follicle showing small, cleaved cell cytology (centrocytes) as the predominant cell type. These are features associated with grade 1 histology using the 3 grade system in use by the World Health Organization Classification of Hematological Malignancy.
VII.C.025 Follicular Lymphoma
VII.C.025
Follicular lymphoma. Lymph node biopsy. Admixed amongst the centrocytes are scattered large cells with prominent nucleoli called centroblasts (arrow). Follicular lymphoma can be graded histologically based on the number of centroblasts from low grade (grade 1) to more aggressive (grade 3) cases. In the particular case illustrated, the majority of the tumor met criteria for histologic grade 2.
VII.C.026 Follicular lymphoma
VII.C.027 Follicular Lymphoma
VII.C.028 Follicular Lymphoma
VII.C.028
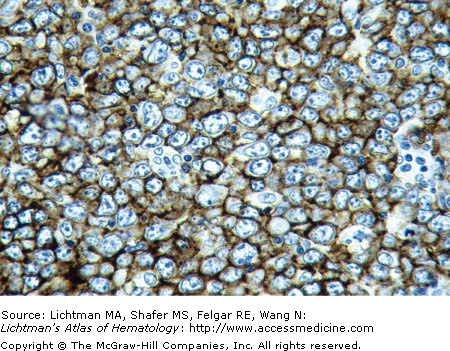
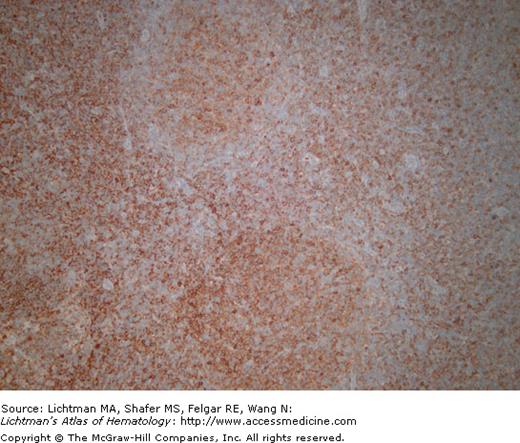
Follicular lymphoma. Lymph node biopsy. BCL-2 immunostain shows reddish-brown staining of neoplastic follicular cells. Normal germinal center cells are negative for BCL-2, an anti-apoptotic protein. In follicular lymphoma, tumor cells over express BCL-2 as a result of a t(14;18) translocation in which the BCL-2 gene locus is translocation next to the immunoglobulin heavy chain locus, resulting in constitutive over expression of this gene product.
VII.C.029 Follicular Lymphoma, Large Cell Type, Histologic Grade 3a
VII.C.029
Follicular lymphoma, large cell type, histologic grade 3a. Lymph node biopsy. This specimen illustrates a case of follicular lymphoma at the more high-grade end of the histologic spectrum of cases. In grade 3a histology, more than 15 centroblasts can be seen per standard 40x (high power) microscopic field. In grade 3a, centroblasts are seen as single cells scattered within a background of centrocytes. In grade 3b, these centroblasts form large clusters or sheets. Survival curves in clinical trials have clearly established the more aggressive nature of grade 3 histology over grade 1 histology. More recent studies have suggested also that separation into grade 3a and grade 3b (as outlined above) may also help to predict more aggressive from more indolent cases within that particular subtype.
VII.C.030 Intravascular Large B-Cell Lymphoma
VII.C.030
Intravascular large B-cell lymphoma. Lung biopsy. H&E section. This rare type of large cell lymphoma shows neoplastic centroblasts in small blood vessels. The centroblasts remain confined to the intravascular space. Scattered microinfarctions are often present. Two arrows point to microvasculature plugged with tumor cells.
VII.C.031 Intravascular Large B-Cell Lymphoma
VII.C.032 Lymphomatoid Granulomatosis
VII.C.032
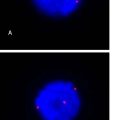
Lymphomatoid granulomatosis. (A) Angiocentric-angioinvasive and destructive lesion that is Epstein-Barr virus–driven and occurs commonly in lungs, liver, brain, and skin but can be seen at any site. This is a grade 1 lesion. The majority of background cells are reactive T cells. Lesions are graded on a scale of 1 to 3 based on the number of large cells and nuclear atypia. Grade 3 lesions are considered to be a form of large B-cell lymphoma, an aggressive neoplasm. (B) The admixed large CD20+ B cells are positive for Epstein-Barr virus latent RNA (EBER) as indicated by the blue-black nuclear reaction product in two B cells. The nuclei of non-reactive cells are stained pale pink.
VII.C.033 Mantle Cell Lymphoma
VII.C.034 Mantle Cell Lymphoma
Get Clinical Tree app for offline access