Chapter 38 Management of the Neck
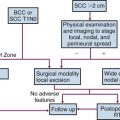
Anatomy of the Lymphatic System of the Neck
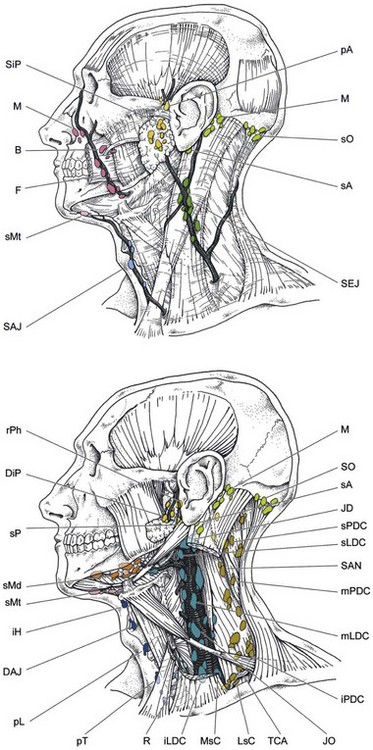
The head and neck region has a rich network of lymphatic vessels draining from the base of the skull through the jugular nodes, spinal accessory nodes, and transverse cervical nodes to the venous jugulosubclavian confluence or the thoracic duct on the left side and the lymphatic duct on the right side.1,2 A comprehensive anatomic description of this network was made by Rouvière more than 50 years ago.1 The whole lymphatic system of the neck is contained in the celluloadipose tissue delineated by the aponeurosis enveloping the muscles, vessels, and nerves (Fig. 38-1). The lymphatic drainage is mainly ipsilateral, but structures such as the soft palate, tonsils, base of the tongue, posterior pharyngeal wall, and especially the nasopharynx have bilateral drainage. On the other hand, sites such as the true vocal cord, paranasal sinuses, and middle ear have few or no lymphatic vessels at all.
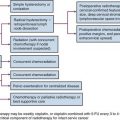
The nomenclature of head and neck lymph nodes has been complicated by various confusing synonyms that are still in use in major textbooks and articles. Several expert bodies have proposed the adoption of systematic classifications aimed at standardizing the terminology. Following the description by Rouvière, the TNM (primary tumor, regional nodes, metastases) atlas proposed a terminology that divides the head and neck lymph nodes into 12 groups.3 In parallel to this classification, the Committee for Head and Neck Surgery and Oncology of the American Academy for Otolaryngology–Head and Neck Surgery has been working on a classification (the so-called Robbins classification), dividing the neck into six levels, including eight node groups.4 This classification is based on the description of a level system that has been used for a long time by the Head and Neck Service at the Memorial Sloan-Kettering Cancer Center (MSKCC).5 Because one of the objectives in developing the Robbins classification was to create a standardized system of terminology for neck dissection procedures, only the lymph node groups routinely removed during neck dissection were considered. The terminology proposed by Robbins was recommended by the International Union Against Cancer (UICC).6 A comparison of the TNM system and the Robbins terminology is shown in Table 38-1. The major advantage of the Robbins classification over the TNM terminology is the definition of the boundaries of the node levels. The delineation of these boundaries is based on anatomic structures such as major blood vessels, muscles, nerves, bones, and cartilage that are easily identifiable by a surgeon during neck dissection procedures. The anatomic boundaries are oriented to a patient lying in a supine position with the neck in a surgical position (i.e., hyperextension) to better individualize the anatomic structures.
TABLE 38-1 Comparison of the TNM Atlas Terminology and the Robbins Classification of the Lymph Nodes of the Neck
Level IV includes the lower jugular lymph nodes located around the inferior third of the internal jugular vein from the caudal limit of level III to the clavicle caudally. The anterior and posterior limits are the same as for level III (i.e., the lateral border of the sternohyoid muscle and the posterior edge of the sternocleidomastoid muscle, respectively). Laterally, level IV is limited by the sternocleidomastoid muscle and medially by the internal carotid artery and paraspinal muscles. Level IV contains a variable number of nodes and receives efferent lymphatics primarily from levels III and V; some efferent lymphatics from the retropharyngeal, pretracheal, and recurrent laryngeal nodes; and collecting lymphatics from the hypopharynx, larynx, and thyroid gland.1 Level IV nodes are at high risk for harboring metastases from cancers of the hypopharynx, larynx, and cervical esophagus.
Level V includes the lymph nodes of the posterior triangle group. This group includes the lymph nodes located along the lower part of the spinal accessory nerve and the transverse cervical vessels. Level V is limited cranially by the convergence of the sternocleidomastoid muscle and the trapezius muscles, caudally by the clavicle, anteriorly by the posterior border of the sternocleidomastoid muscle, and posteriorly by the anterior border of the trapezius muscle. Laterally, level V is limited by the platysma muscle and the skin and medially by the splenius capitis, levator scapulae, and scaleni (posterior, medial, and anterior) muscles. Level V is currently subdivided into levels Va and Vb. The distinction between the upper posterior triangle (level Va) and the lower posterior triangle (level Vb) allows lymph node involvement of the lower two-thirds of the spinal accessory nerve chain to be differentiated from that of the transverse cervical vessel chain.7,8 A horizontal plane defined by the caudal edge of the cricoid cartilage separates these two compartments. The demarcation between the posterior end of level IIb and the uppermost part of level Va has still not been clearly defined. The American Academy for Otolaryngology–Head and Neck Surgery defined the posterior boundary of level IIb as the posterior border of the sternocleidomastoid muscle and the apex of the convergence of the sternocleidomastoid muscle and the trapezius muscles as the cranial boundary of level Va. However, the uppermost part of level Va contains superficial occipital lymph nodes and, inconsistently, one subfascial lymph node close to the occipital attachment of the sternocleidomastoid muscle.1
These lymph nodes collect lymphatics from the occipital scalp and the postauricular and nuchal regions. They are not involved in the drainage of head and neck cancers except for skin tumors. Consequently, Hamoir and colleagues9 proposed to subdivide the level Va nodes into two sublevels: the apex of level V, or level Vas (superior), and level Vai (inferior). The border between level Vas and level Vai should be the lower two-thirds of the spinal accessory nerve. From a radiologic point of view, a horizontal plane defined by the upper edge of the body of the hyoid bone appears to be a reliable landmark to separate the two sections. Dissection of the apex (level Vas) does not seem to be required in mucosal head and neck squamous cell carcinoma. It should be considered only in cases of skin cancer of the posterior scalp and posterior neck. Level V receives efferent lymphatics from the occipital and postauricular nodes and from the occipital and parietal scalp, skin of the lateral and posterior neck and shoulder, nasopharynx, and oropharynx (tonsils and base of the tongue). Level V lymph nodes are at high risk for harboring metastases from cancers of the nasopharynx and oropharynx. Nodes in level Va are more often associated with primary cancers of the nasopharynx, oropharynx, or cutaneous structures of the posterior scalp, whereas those in level Vb are more commonly associated with tumors arising in the thyroid gland.
Imaging of the Neck
The armamentarium available for the imaging workup of the metastatic cervical lymph nodes includes computed tomography (CT), magnetic resonance imaging (MRI), ultrasonography, and positron emission tomography (PET).10 Nodal imaging is mandatory in a pretreatment workup because clinical assessment of the nodal status in patients with a thick and/or small neck has a low sensitivity and because deeply located nodes remain inaccessible in all patients.11
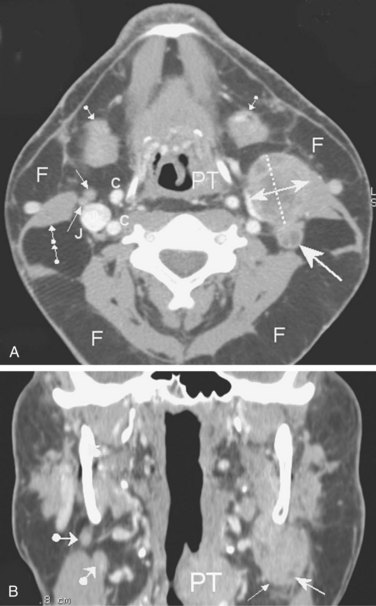
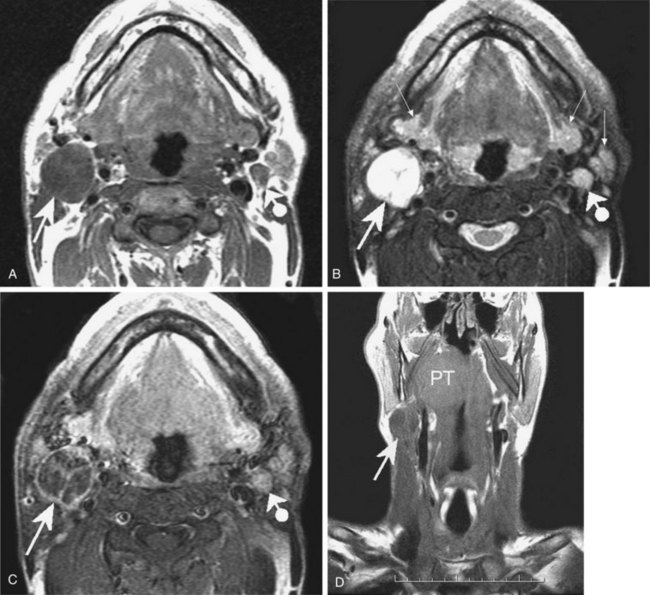
CT and MRI are standard cross-sectional imaging modalities through which anatomic “slices” of the entire neck depict the contours and internal structure of the nodes (Figs. 38-2 and 38-3). MRI may have an advantage over CT scanning because of the higher spontaneous contrast it reveals between fatty and nonfatty tissues. The multiplanar capability of MRI has been an advantage of this technique since its introduction into clinical use in the early 1980s. However, the multirow detector technology and the spiral acquisition modality of newer-generation CT systems have boosted the multiplanar reformatting capabilities of CT scans, which now equal those of MR images. The major criteria for nodal malignancy using CT and/or MRI include the size of the nodes (a short axis longer than 10 mm) and the presence of a central necrosis (hypodensity on CT images; hypointensity on T1-weighted MR images and hyperintensity on T2-weighted MR images). Central necrosis is well highlighted by intravenous contrast agent perfusion, which enhances nodal areas with arterial blood supply on both CT and MR images (see Figs. 38-2A and 38-3C). However, the two techniques share common weaknesses: the inability to detect micrometastatic deposits within normal-sized nodes (false-negative results) and the risk for inappropriate classification of malignancy in nodes that are enlarged by benign reactive changes (false-positive results). Thus far, neither MRI nor CT can provide perfect diagnostic accuracy for nodal metastatic workup. It has been shown in a large series of patients that the two techniques have an almost similar and unsatisfactory performance.12
Ultrasonography has long been regarded as a low-cost, widely available, and innocuous alternative to CT/MRI, with the additional advantages of color Doppler flow–encoded vascular architecture depiction and fine-needle aspiration guidance. However, time demands and operator skill requirements are limiting factors, as well as the unresolved technical difficulties of fusing two-dimensional ultrasound data and three-dimensional CT/MRI data for radiotherapy planning. Ultrasound is also less efficient than CT and MRI at detecting nodal necrosis,13 and deeply located nodes may be poorly accessible to the technique.
Research is underway to improve the diagnostic accuracy of MRI, including experimental lymphophilic contrast agents, magnetization transfer imaging (MTI), free water diffusion-weighted imaging (DWI), magnetic resonance spectroscopy (MRS), and bolus tracking perfusion-weighted imaging (PWI).14–16 Currently, only the DWI MR technique has made a definite breakthrough in clinical routine by yielding fast-to-acquire and easy-to-process accurate quantitative data that significantly add to pretherapeutic nodal staging attempts,17–19 early prediction of therapeutic response,20 and post-treatment early detection of residual/recurrent tumor.21 Many think that molecular imaging probes targeting either specific membrane antigens or metabolic pathways of tumor cells could be the definitive contributors to perfect diagnostic accuracy in nodal metastatic workup, in which case MRI and PET will be competitors.
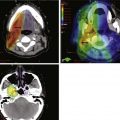
PET using fluorodeoxyglucose (FDG) as a tracer has become the most available technique for “metabolic imaging” by enhancing foci of increased glucose uptake. However, PET alone provides only restricted diagnostic accuracy. The limitations of PET can be offset by coregistering the information on anatomic CT or MR images22 (Fig. 38-4). Integrated PET/CT combines the poor anatomic localization of PET with the accurate morphologic data provided by CT. The results of a recent large, prospective study showed that FDG-PET significantly improved the staging of HNSCC because of its detection of metastatic or additional disease.23 However, a recent meta-analysis totaling 1236 patients demonstrated that the accuracy of FDG-PET was only marginally superior to that of CT or MRI; this study calls into question the routine value of FDG-PET for nodal staging.24 In addition to research on dedicated tissue-specific MR contrast agents, research is under way on PET radiopharmaceutical tracers that would allow the assessment of hypoxia, angiogenesis, apoptosis, and receptor status; these studies make up the second main field of research in oncology imaging.25 Using anatomic imaging studies to detect tumor recurrences in previously treated primary sites is unsatisfactory because extensive unspecific post-therapeutic changes may mask small foci of neoplastic recurrence.26 On the other hand, very promising data have been reported with the use of FDG-PET in this setting.27 Similar concepts apply to nodal metastases, and it may be possible that molecular and metabolic imaging methods will also become standard in nodal relapse detection. The key imaging concept for the radiation oncologist’s day-to-day practice is the capability of superimposing PET/MRI metabolic/molecular mapping onto CT/MRI anatomic images to improve the delineation of the irradiation target.28 PET-CT and PET-MRI fusions are the founding paradigms that have now emerged into the clinical routine29 (see Figs. 38-3 and 38-4).
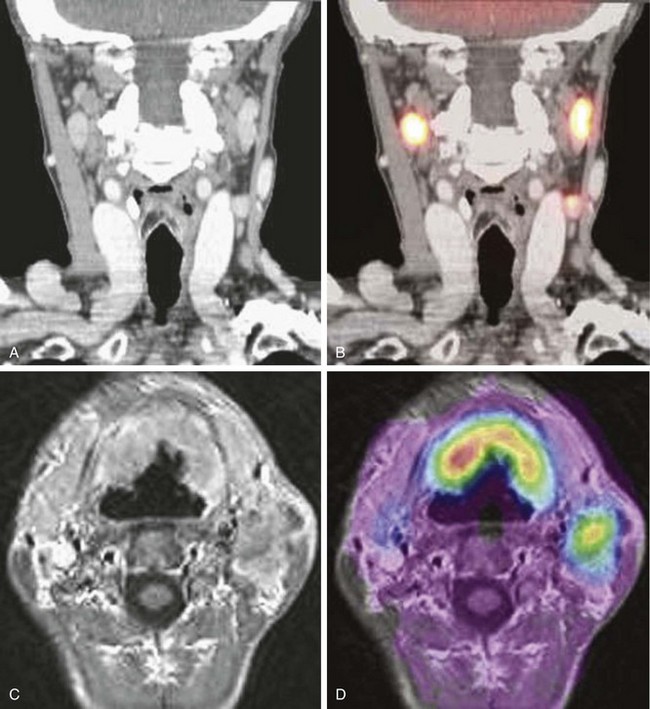
Figure 38-4 CT-MRI-PET image fusion. A, Postcontrast, reformatted CT image in the coronal plane shows bilateral, mildly enlarged metastatic nodes in the carotid-jugular chains. Tumoral involvement of the nodes remains speculative because of the borderline short-axis diameter and absence of obvious necrotic changes. B, Superimposition of 18F-fluorodeoxyglucose positron emission tomography (FDG-PET) data on a CT image demonstrates increased glucose uptake within the nodes. C, Postcontrast, T1-weighted, axial transverse MR image from three-dimensional gradient-echo acquisition using spoiled gradients (SPGR) shows bilateral anterior, horseshoe-sized oropharyngeal tumor and metastatic left-sided nodes in level II. D, Superimposition of FDG-PET data on an MR image demonstrates increased glucose uptake within the primary tumor and metastatic nodes.
Courtesy M. Lonneux, MD, PhD.
Staging of Neck Node Metastases
The seventh edition (2009) of the American Joint Committee on Cancer (AJCC) staging for neck node metastases30 is presented in Table 38-2. This classification does not apply to nasopharyngeal, thyroid, or skin cancers. The classification for nodal staging applies whether the modality used for neck assessment is clinical examination or imaging. The routine use of CT or MRI and—in expert hands—ultrasound is recommended especially for assessing nodes not clinically identifiable (e.g., retropharyngeal, intraparotid, or superior mediastinal nodes) or for patients for whom clinical palpation of the neck is less sensitive (e.g., those who have a thick or small neck).31 Last, it should be emphasized that the Nx classification applies only when the neck has not been assessed or could not be assessed.
TABLE 38-2 American Joint Committee on Cancer Staging for Neck Node Metastasis
| Category | Definition |
|---|---|
| Nx | Regional lymph nodes cannot be assessed |
| N0 | No regional lymph node metastasis |
| N1 | Metastasis in a single ipsilateral node, ≤3 cm in greatest dimension |
| N2a | Metastasis in a single ipsilateral node, >3 cm but ≤6 cm in greatest dimension |
| N2b | Metastasis in multiple ipsilateral nodes, ≤6 cm in greatest dimension |
| N2c | Metastasis in bilateral or contralateral nodes, ≤6 cm in greatest dimension |
| N3 | Metastasis in a lymph node >6 cm in greatest dimension |
From Sobin L, Gospodarowicz M, Wittekind C: UICC/TNM Classification of Malignant Tumors (7th ed.) New York, 2009, Wiley-Blackwell.
Incidence and Distribution of Neck Node Metastases
Clinical and Radiologic Assessment
The metastatic spread of head and neck tumors into the cervical lymph nodes is rather consistent and follows predictable pathways, at least in the neck that has not been violated by previous surgery or radiotherapy. In Table 38-3, the frequency of metastatic lymph nodes is expressed as a percentage of node-positive patients.32,33
TABLE 38-3 Distribution of Clinical Metastatic Neck Nodes from Oral Cavity and Pharyngolaryngeal Squamous Cell Carcinomas
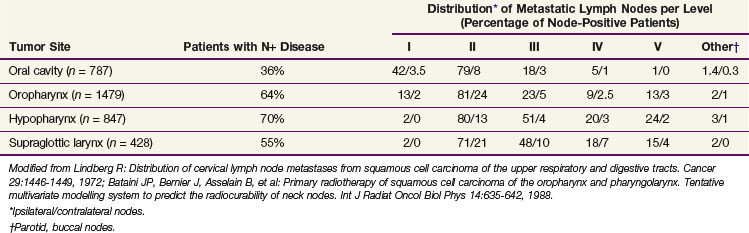
Metastatic lymph node involvement in the neck depends on the size of the primary tumor, increasing with the T category. In the series reported by Bataini and associates,32 44% of patients with a T1 tumor had clinical lymph node involvement; this increased to 70% for patients with T4 lesions. There are, however, no data suggesting that the relative distribution of involved neck levels varies with the T category.
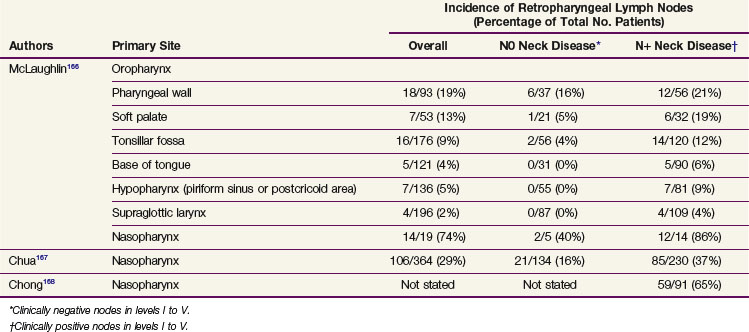
Retropharyngeal lymph nodes represent a special entity because they are usually not clinically detectable. The incidence of retropharyngeal lymph node involvement can be estimated only from series in which CT or MRI of the retropharynx has been systematically performed as part of the diagnostic procedure. Retropharyngeal node involvement occurs in primary tumors arising from (or invading) the mucosa of the occipital and cervical somites, such as the nasopharynx, pharyngeal wall, and soft palate (Table 38-4). The incidence of retropharyngeal lymph node involvement is higher in patients in whom involvement of other neck node levels has also been documented. However, in patients with clinical stage N0 nasopharyngeal tumors and, to a lesser extent, in patients with pharyngeal wall tumors, the incidence of retropharyngeal node involvement is still significant—between 16% and 40%. Also, as already described for the other lymph node levels, involvement depends on the T category and is typically lower for T1 tumors. Accurate figures are not available.
Pathologic Lymph Node Metastases
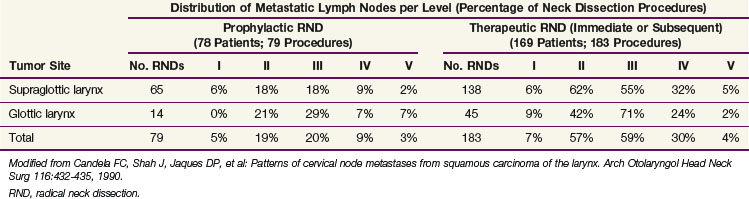
The distribution of pathologic lymph node metastasis in patients with primary tumors of the oral cavity, oropharynx, hypopharynx, and larynx can be derived from retrospective series in which a systematic radical neck node dissection was proposed as part of the initial treatment procedures.34–37 Retrospective series are essentially biased regarding patient and treatment selection, but these series from the Head and Neck Department at MSKCC are the largest and most consistent data ever published on that matter. The results of these retrospective studies are shown in Tables 38-5 to 38-8. The data are presented in terms of the number of neck dissections with positive lymph nodes divided by the total number of neck dissection procedures and expressed as a percentage. Most patients (>99% for patients with N0 tumors and 95% for patients with N+ tumors) had unilateral treatment only, and no distinction between the ipsilateral and contralateral neck was made.
TABLE 38-5 Incidence of Pathologic Lymph Node Metastasis in Squamous Cell Carcinomas of the Oral Cavity
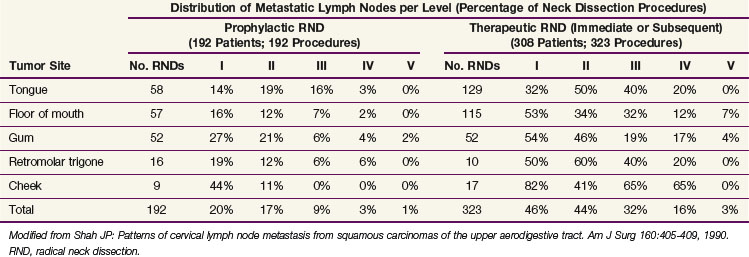
TABLE 38-6 Incidence of Pathologic Lymph Node Metastasis in Squamous Cell Carcinomas of the Oropharynx
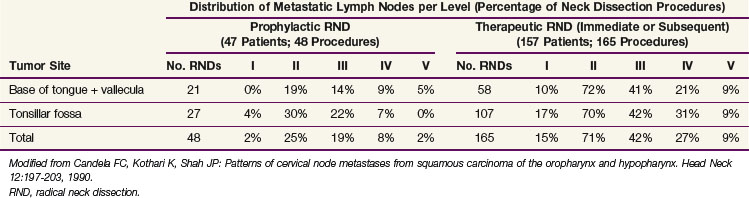
TABLE 38-7 Incidence of Pathologic Lymph Node Metastasis in Squamous Cell Carcinomas of the Hypopharynx
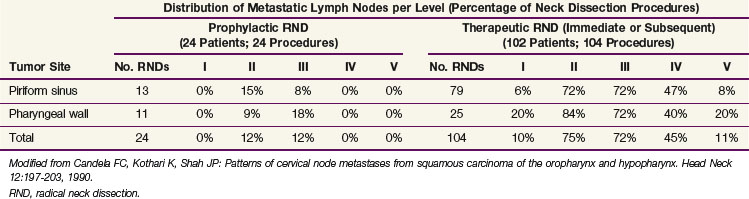
The pattern of metastatic node distribution in patients who underwent therapeutic neck dissection was similar to that observed in patients with N0 tumors, with the difference that significant pathologic infiltration of an additional nodal level was typically observed—level IV for oral cavity tumors and levels I and V for oropharyngeal, hypopharyngeal and, to a lesser extent, laryngeal tumors. Overall, this observation illustrates the gradual infiltration of node levels in the neck. This concept is well illustrated by the prevalence of metastases in level V. In the MSKCC series,38 the prevalence of pathologic infiltration in level V was quite low, averaging 3% in 1277 neck dissections in patients with oral cavity, oropharyngeal, hypopharyngeal, and laryngeal tumors. The prevalence peaked at 11% for hypopharyngeal tumors with pathologically positive nodes (see Table 38-7). A thorough analysis of level V infiltration showed that for all tumor sites pooled together, infiltration of level V without metastases in levels I to IV was observed in only one patient (0.2%). This patient had a hypopharyngeal tumor. Infiltration in level V remained below 1% when a single pathologically confirmed positive node was also observed in levels I to III, but reached 16% when a single pathologically confirmed positive node was also observed in level IV. When more than one level was infiltrated, the probability of level V involvement progressively increased, reaching 40% when levels I to IV were all involved. The pattern of involvement of level I is also a good illustration of the concept of gradual node infiltration. In the MSKCC series, pathologic involvement of level I was found in only 2% of patients with clinical stage N0 oropharyngeal tumors (see Table 38-6) and was not observed in patients with clinical stage N0 hypopharyngeal tumors (see Table 38-7). On the other hand, in patients with clinically positive nodes, metastases in level I were reported in 15% and 10% of patients with oropharyngeal and hypopharyngeal tumors, respectively.
Incidence of Skip Metastases in the Neck
Skip metastases are metastases that do not progress in an orderly manner from one level to the next (e.g., from level I to level II). Depending on their frequency, skip metastases in patients with clinical stage N0 tumors may have a profound implication for the therapeutic management of the neck. In the series from the MSKCC,37 8 of 343 patients with clinical stage N0 tumors (2.5%) developed skip metastases. Seven of these patients had oral cavity tumors that metastasized in level IV or V only. One patient had a laryngeal tumor. These low figures are in good agreement with a rate of neck failure outside the dissected levels of 3% (2 of 64 lesions) observed in patients with pathologic N0 lesions treated at the same institution by supraomohyoid neck dissection.39 Most of these patients had tumors of the oral cavity. None of them received postoperative radiation therapy because they were all free of metastases. Byers and colleagues40 carefully evaluated the frequency of skip metastases in 270 patients primarily treated by surgery at the M.D. Anderson Cancer Center from 1970 to 1990 for squamous cell carcinoma of the oral tongue. Of these patients, 12 had metastases in level III only, 9 had metastases in level IV only, and 2 had metastases in level IIb (i.e., nodes that are far enough posterior to the internal jugular vein). In addition, in 90 of the patients who had pathologic stage N0 tumors after selective neck dissection of levels I to III and who did not receive postoperative radiation therapy, 9 subsequently developed recurrence in level IV Altogether (in levels IIb, III, and IV), the frequency of skip metastases reached 12% (32 of 270 lesions). If one excludes the skip metastases in level IIb and III, the frequency reached only 7% (18 of 270 lesions).
Incidence and Pattern of Node Distribution in the Contralateral Neck
There are very few data available on the pattern of pathologic node distribution in the contralateral neck. Bilateral neck dissection was performed only when the surgeon thought there was a high risk of contralateral node involvement (e.g., with tumors of the oral cavity or oropharynx reaching the midline or extending beyond it, or with hypopharyngeal and supraglottic tumors). Obviously, in such cases bilateral radical neck dissection was never performed, so an accurate estimate of the pattern of node involvement in levels I to V of the contralateral neck is not possible. Furthermore, in almost every study, data on both sides of the neck were pooled for presentation. Kowalski41 presented data on 90 patients who underwent bilateral supraomohyoid neck dissection and in whom the pattern of node distribution in each side of the neck was reported separately. Most of these patients had squamous cell carcinoma of the lip or oral cavity. In the ipsilateral neck, pathologic infiltration in levels I, II, and III reached 20%, 15%, and 15%, respectively. In the contralateral neck, corresponding values reached 13%, 11%, and 0%, respectively. These figures are in good agreement with data on clinical node distribution showing that both sides of the neck exhibited a similar pattern of node distribution but with a lower incidence in the contralateral neck.
Foote and colleagues42 reported the rate of contralateral neck failure in a limited series of 46 patients with clinical stage N0 base of the tongue tumors treated by some form of glossectomy and ipsilateral neck dissection. None of these patients received postoperative radiation therapy. Ten patients (22%) had contralateral neck recurrence, and the most common sites were levels II, III, and IV. It appears that in two of these patients, recurrence was also observed at the primary site. The development of delayed contralateral neck metastases was not related to the clinical or pathologic extent of the base of the tongue tumor. O’Sullivan and associates43 reported a retrospective series of 228 patients with tonsillar carcinoma who were treated for the primary tumor and in the ipsilateral neck only with radiation therapy. The vast majority of these patients had T1 to T2 and N0 to N1 disease. Contralateral recurrence in the neck was observed in only eight patients (2%), including five patients with local recurrence as well. None of these neck failures occurred in the 133 patients with stage N0 tumors. Although not significant because of the small number of events, involvement of a midline structure (i.e., soft palate and base of the tongue) appeared to be a prognostic factor for contralateral neck recurrence. Similar results were reported in a series of 101 node-negative tonsil carcinoma (mainly, stage T1 to T3) cases treated unilaterally.44 Only two neck recurrences were observed in the contralateral neck.
Recommendations for Selection of Target Volumes in the Neck
Metastatic lymph node involvement of primary squamous cell carcinoma of the oral cavity, pharynx, and larynx typically follows a predictive pattern. Data on clinical and pathologic neck node distribution as well as on neck recurrence after selective dissection procedures support the concept that not all neck node levels should be treated as part of the initial management strategy of head and neck primaries of squamous cell origin.45,46 However, the data on which such a concept is based have come from retrospective series and so may include possible biases (e.g., in patient selection, use of a series from the preimaging area, and so on) that could limit their validity.
Tables 38-9 to 38-12 present recommendations for the selection of clinical target volumes in the neck for pharyngolaryngeal squamous cell carcinomas. These guidelines can be applied whether the treatment modality is surgery or radiotherapy. A complete discussion on choosing between these two modalities is beyond the scope of this chapter, but factors to consider include the neck stage, the treatment option for the primary tumor, the performance status of the patient, and the institutional policy agreed on by a multidisciplinary head and neck tumor board.
TABLE 38-9 Recommendations for Selection of Clinical Target Volume in the Neck for Oral Cavity Tumors
| Nodal Category (AJCC) | Levels to Be Included in CTV | |
|---|---|---|
| Ipsilateral Neck | Contralateral Neck | |
| N0-1 (in level I, II, or III) | I, II,* III, + IV† | I, II,* III, + IV† |
| N2a-b | I, II, III, IV, V‡ | I, II,* III, + IV for anterior tongue tumor |
| N2c | According to N stage on each side of the neck | According to N stage on each side of the neck |
| N3 | I, II, III, IV, V ± adjacent structures according to clinical and radiologic data | I, II,* III, + IV for anterior tongue tumor |
AJCC, American Joint Committee on Cancer; CTV, clinical target volume.
* Level IIb could be omitted for stage N0 tumors.
† For anterior tongue tumor and any tumor with extension to the oropharynx (e.g., anterior tonsillar pillar, tonsillar fossae, base of tongue).
‡ Level V could be omitted if only levels I to III are involved.
TABLE 38-10 Recommendations for Selection of Clinical Target Volume in the Neck for Oropharyngeal Tumors
| Nodal Category (AJCC) | Levels to Be Included in the CTV | |
|---|---|---|
| Ipsilateral Neck | Contralateral Neck | |
| N0-1 (in level II, III, or IV) | (Ib),* II, III, IV, + RP for posterior pharyngeal wall tumor | II, III, IV, + RP for posterior pharyngeal wall tumor |
| N2a-b | Ib, II, III, IV, V, + RP | II, III, IV, + RP for posterior pharyngeal wall tumor |
| N2c | According to N stage on each side of the neck | According to N stage on each side of the neck |
| N3 | I, II, III, IV, V, + RP ± adjacent structures according to clinical and radiologic data | II, III, IV, + RP for posterior pharyngeal wall tumor |
AJCC, American Joint Committee on Cancer; CTV, clinical target volume; RP, retropharyngeal nodes.
* Any tumor with extension to the oral cavity (e.g., retromolar trigone, mobile tongue, inferior gum, oral side of anterior tonsillar pillar).
TABLE 38-11 Recommendations for Selection of Clinical Target Volume in the Neck for Hypopharyngeal Tumors
| Nodal Category (AJCC) | Levels to Be Included in the CTV | |
|---|---|---|
| Ipsilateral Neck | Contralateral Neck | |
| N0 | II,* III, IV, + RP for posterior pharyngeal wall tumor + VI for apex of piriform sinus or esophageal extension | II,* III, IV, + RP for posterior pharyngeal wall tumor + VI for esophageal extension |
| N1N2a-b | Ib, II, III, IV, V, + RP + VI for piriform sinus or esophageal extension | II,* III, IV, + RP for posterior pharyngeal wall tumor + VI for esophageal extension |
| N2c | According to N stage on each side of the neck | According to N stage on each side of the neck |
| N3 | I, II, III, IV, V, + RP + VI for piriform sinus or esophageal extension ± adjacent structures according to clinical and radiologic data | II,* III, IV, + RP for posterior pharyngeal wall tumor + VI for esophageal extension |
AJCC, American Joint Committee on Cancer; CTV, clinical target volume; RP, retropharyngeal (nodes).
* Level IIb could be omitted for stage N0 tumors.
TABLE 38-12 Recommendations for Selection of Clinical Target Volume in the Neck for Laryngeal Tumors (Stage T1 N0 Glottic Carcinoma Excluded)
| Nodal Category (AJCC) | Levels to Be Included in the CTV | |
|---|---|---|
| Ipsilateral Neck | Contralateral Neck | |
| N0-1 (in level II, III, or IV) | II,* III, IV, + VI for transglottic or subglottic extension | II,* III, IV, + VI for transglottic or subglottic extension |
| N2a-b | II, III, IV, V, + VI for transglottic or subglottic extension | II,* III, IV, + VI for transglottic or subglottic extension |
| N2c | According to N stage on each side of the neck | According to N stage on each side of the neck |
| N3 | Ib, II, III, IV, V, + VI for transglottic or subglottic extension ± adjacent structures according to clinical and radiologic data | II,* III, IV, + VI for transglottic or subglottic extension |
AJCC, American Joint Committee on Cancer; CTV, clinical target volume.
* Level IIb could be omitted for stage N0 tumors.
Selective treatment of the neck is appropriate for patients with clinical N0 HNSCC of the oral cavity, oropharynx, hypopharynx, and larynx.39,46,47 Typically, level I to III nodes should be treated for oral cavity tumors, and level II to IV nodes should be treated for oropharyngeal, hypopharyngeal, and laryngeal tumors. Robbins7 suggested that elective treatment of level IIb nodes is probably not necessary for patients with clinical stage N0 primary tumors of the oral cavity, larynx, or hypopharynx. However, Byers and associates40 suggested that level IV nodes be included in the treatment of the mobile tongue because of the high incidence (10%) of skip metastases. Retropharyngeal nodes should be treated in tumors of the posterior pharyngeal wall. For subglottic tumors, tumors with subglottic or transglottic extension, or hypopharyngeal tumors with esophageal extension, level VI nodes should also be included in the treatment volume.
As proposed by Byers,47 similar guidelines could be recommended for patients who have N1 tumors without radiologic evidence of extracapsular infiltration. However, when an involved lymph node is located at a boundary of a level that has not been selected for the target volume, it is recommended to extend the selection to include the adjacent level.48 Typically, this applies only for oropharyngeal tumors with a single lymph node involved in level II at the boundary with level Ib or for an oral cavity tumor with an N1 node in level III at the boundary with level IV.
For patients with multiple nodes (N2b), the available data suggest that adequate treatment should include nodes in levels I to V. Level I nodes could, however, be omitted for laryngeal tumors, and level V nodes omitted for oral cavity tumors with neck involvement limited to levels I to III. Prophylactic treatment of the retropharyngeal nodes should be systematically performed for oropharyngeal and hypopharyngeal tumors. Patients with N0 disease should have level VI nodes treated for subglottic tumors, tumors with subglottic or transglottic extension, or hypopharyngeal tumors with esophageal extension. It has been proposed that patients with nodes in the upper neck (i.e., upper level II nodes) have the upper limit of the target volume extended to include the retrostyloid space.48 Similarly, the subclavicular fossae should be included in the target volume in cases of lower neck involvement (i.e., level IV or Vb nodes).48
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree