Patients and families struggling with cancer fear pain more than any other physical symptom. There are also significant barriers to optimal pain management in the emergency setting, including lack of knowledge, inexperienced clinicians, myths about addiction, and fears of complications after discharge. In this article, we review the assessment and management options for cancer-related pain based on the World Health Organization (WHO) 3-step approach.
Patients and families struggling with cancer fear pain more than any other physical symptom. With the treatment of malignant pain remaining a challenge in the practice of oncology, the emergency department (ED) is often a place of refuge. There are significant barriers to optimal pain management in the emergency setting, including lack of knowledge, inexperienced clinicians, myths about addiction, and fears of complications after discharge. These factors contribute to unnecessary suffering not only for the patient but also for family and caregivers. Malignant pain is highly responsive to medication. Adequate malignant pain control is possible in more than 90% of patients if established therapeutic approaches are applied systematically in any practice setting, including the ED. It has been suggested that management of an acute pain crisis in a patient with advanced cancer “is as much a crisis as a code,” and emergency clinicians should, and can, become comfortable caring for patients with cancer in acute pain.
Patients with cancer often present to the ED because their pain is unmanageable. Although there are multiple physiologic possibilities for inadequate pain control, the emergency clinician should also be aware of the many psychosocial factors contributing to oligoanalgesia in the cancer patient. Depression, unresolved spiritual or social concerns, and misconceptions of prescribed medications may interfere with adequate treatment. With a properly focused evaluation, the treatment of unresolved pain in the cancer patient can be performed rapidly and effectively in the ED.
Assessment of malignant pain
General principles of good pain assessment are particularly important in the patient presenting to the ED with malignancy. A rapid assessment of severity, character, likely etiology, timing and location, exacerbating and relieving factors, and associated symptoms provides essential information for proper management. In addition, the details of the history may reveal particular cancer pain syndromes, some of which require urgent diagnosis and intervention to prevent permanent functional impairment. With an adequate assessment, effective therapy can be quickly implemented in the ED.
The assessment of pain severity in cancer is the same as that of nonmalignant pain. There are several validated measures of a patient’s pain experience. Although any scale is useful for a given patient as long as it is applied consistently, the preferred scale for most patients is the numerical rating scale (NRS). Most commonly, this is an 11-point scale from 0 = “no pain” to 10 = “worst possible pain.” For small children or patients with limited literacy, a picture scale is more successful, with the Faces Pain Scale being a well-accepted choice. In the cognitively impaired patient, the 5-time observational Pain Assessment in Advanced Dementia Scale may be used. All of these scales have been validated and have utility in the ED for the assessment of pain. It should be emphasized that pain scales are intended to provide objectivity to the experience of the patient’s pain. Skepticism has no place in the assessment of suffering and may directly impair proper diagnosis and treatment. Pain can be complex, and these scales provide an objective method of evaluation to gauge treatment success. This is particularly true in acute pain.
The character and etiology of pain are described physiologically as either nociceptive or neuropathic. Cancer pain can be either or both. Nociceptive pain is a response to damaged tissue and can further be classified as either somatic (musculoskeletal/cutaneous) or visceral. Somatic pain is often described as sharp or aching and localized to the area of tissue damage. Pain secondary to bone metastasis is a classic example of somatic pain. Visceral pain is more poorly localized and can be intermittent, sometimes described as dull or cramping. Abdominal pain associated with ovarian or pancreatic cancers is characteristic. Neuropathic pain is primarily caused by nerve injury. The injury may be mechanical (eg, amputation), metabolic (eg, diabetes), inflammatory (eg, radiation), or toxic (eg, chemotherapy). Neuropathic pain is typically persistent and sometimes paroxysmal and shock-like. Normal stimulus may elicit abnormal pain responses (allodynia). A light touch, for example, may elicit searing pain. There can also be autonomic instability in the affected area, including edema or localized sweating such as that which occurs with complex reflex sympathetic dystrophy. An important treatment distinction between these types of pain is that patients with nociceptive pain are generally more responsive to opioids than are patients with neuropathic pain. Neuropathic pain often requires adjunctive nonopioid therapies for successful treatment.
Pain may rapidly change either in quality or location or may be chronic and slowly progressive. Although the alleviation of the pain crisis should always be the first priority, a search for the cause of the underlying pain ensures the most definitive treatment. Specific types of acute pain may require particular therapies for effective treatment, such as radiation therapy for bone metastasis. Likewise, a new location of pain may be the first sign of a dangerous progression of disease requiring diagnostic evaluation, such as new back pain preceding functional deficit in malignant epidural spinal cord compression. In addition to tumor progression, the aggressive treatments for malignancy may also be a cause for the patient’s pain presentation. Surgical tumor resection may have predictable and self-limited associated pain, whereas chemotherapy-induced neuropathy may be less predictable and more persistent. The approach to treatment of these distinct types of pain will be quite different.
The assessment and management of chronic cancer pain (generally regarded as >3 months) can be challenging. Although similar to acute cancer pain in that either disease progression or treatment is typically responsible for the pain, these patients often carry a heavier global burden of suffering. The approach to treatment is more complex and must consider existing medications as well as other factors that may influence the approach to treatment.
Prior to diagnostic and therapeutic efforts in the ED, treatment must be guided by a clear understanding of the patient’s goals of care. Some patients may not wish detailed investigations but may simply require pain treatment. Both acute and chronic cancer pain may be caused by disease progression (62%–78%), treatment (19%–25%), or unrelated (3%–10%) causes. Patients who develop new pain are, therefore, reasonably anxious about disease progression. Communication should be sensitive to these concerns. The highly functional patient might have a goal of aggressively preserving function and longevity through early and aggressive diagnosis and management, whereas comfort alone may be the goal in an imminently dying patient.
The inescapable physical symptoms and the relentless awareness of the progression of the cancer contribute to physical, spiritual, social, and psychological strife. These factors all have the capacity to exacerbate the underlying pain. In addition, patients with pre-existing nonmalignant pain may come to the diagnosis of cancer already experiencing a sense of overwhelming suffering. Cancer patients with pain are twice as likely to develop a psychiatric disorder, and as the disease progresses, the risk increases. The causes are multifactorial, and like pain, may be related to disease progression or treatment. Many of these disorders are amenable to treatment, which should be implemented as early as possible through proper referral and follow-up. An interdisciplinary palliative care team, potentially hospice, should be involved as early as possible. Early palliative care intervention improves patient outcomes and should be initiated by the emergency clinician when the need is identified. Depending on the institution and the urgency of the situation, palliative care consultation may occur in the ED, during hospitalization, or in the outpatient setting.
Treatment strategies
The WHO Stepladder
With a clear assessment of the details of the patient’s pain, effective treatment can be rapidly implemented in the ED. In 1986 the WHO developed a 3-step ladder to guide the management of cancer pain. It was originally developed to address nociceptive pain (both somatic and visceral) but has proved useful to some degree for neuropathic pain as well. This simple and well-tested approach provides the clinician with a rational guide for the use of selected analgesics. Today, there is general consensus favoring the use of this model for all pain associated with serious illness. Management is based on the initial assessment of pain and should start at the step that corresponds to the patient’s reported severity based on an NRS (0–10). Mild pain is defined as NRS 1 to 3 (step 1), moderate pain as NRS 4 to 6 (step 2), and severe pain as NRS 7 to 10 (step 3).
Step 1 analgesics
All of the nonopioid analgesics that characterize step 1 of the WHO ladder have a ceiling effect to their analgesia (a maximum dose that, if exceeded, yields no further analgesia). Acetaminophen is an effective step 1 analgesic and may be a useful coanalgesic in many situations, including headache. Its site and mechanism of action are not entirely known. It does not have significant anti-inflammatory effects and is presumed to have a central cyclo-oxygenase (COX) related mechanism. Chronic doses more than 4.0 g/24 h or acute doses more than 6.0 g/24 h are not recommended because they may cause hepatotoxicity. Hepatic disease or heavy alcohol use increases the risk further, and the maximum daily dosage may be reduced to 3.0 g/24 h.
Nonsteroidal anti-inflammatory drugs (NSAIDs, including aspirin) are also effective step 1 analgesics and may be useful coanalgesics. They work, at least in part, by inhibiting COX, the enzyme that converts arachidonic acid to prostaglandins. There are several classes of NSAIDs. Some patients respond better to one class of NSAIDs than to another, and serial “n of 1” trials may be needed to find one that is efficacious for a given patient. NSAIDs with longer half-lives are likely to enhance compliance. NSAIDs can have significant adverse effects. Gastropathy, renal failure, and inhibition of platelet aggregation can occur with any of the nonselective medications, irrespective of the route of administration. The likelihood of these adverse effects will vary among NSAID classes and may be due, in part, to their relative COX-2 selectivity. It is important to ensure adequate hydration and good urine output in patients on NSAIDs to minimize the risk of renal vasoconstrictive injury, including papillary necrosis. Nonselective medications are relatively contraindicated in the setting of significant pre-existing renal insufficiency. NSAIDs may be contraindicated if bleeding is a problem or coagulation or platelet function is impaired. Gastric cytoprotection with misoprostol or omeprazole may be needed in patients with significant risk of gastrointestinal (GI) problems. Significant risk factors include a history of gastric ulcers or bleeding, current nausea/vomiting, protein wasting, cachexia, and advanced age.
There are parenteral forms of NSAIDs now available for use. A new transdermal form of diclofenac is now available in the United States. Its efficacy has been demonstrated in osteoarthritis but has not yet been studied in localized somatic cancer pain. Ketorolac is available in intravenous (IV) or intramuscular formulations. Short-term (<5 days is considered safe in healthy patients) parenteral use of this potent agent provides excellent analgesia, particularly with visceral pain, and avoids the common central nervous system (CNS) side effects of the opioid analgesics. These advantages must be carefully weighed against the GI, renal, cardiovascular, and bleeding risks for each patient before use.
Step 2 and step 3 analgesics
Step 2 and 3 analgesics involve opioid use. The clinician must have an excellent command of opioid pharmacology when using these analgesics. Step 2 agents all have aspirin or acetaminophen present in amounts that limit their dosages to 10 to 12 tablets a day. These agents have a role in moderate pain (4–7/10), but each also has side effects. Codeine derivatives tend to be constipating, and nausea is not infrequent. There are patients who lack the necessary enzyme to convert codeine to its active (morphine) moiety. Therefore, be aware of the need to change to morphine or a step 3 agent if no analgesia is seen. Effective treatment in the ED requires a clear understanding of the pharmacology, clinical setting, and adverse effects of the analgesics prescribed and knowledge of how these may vary from patient to patient.
Treatment strategies
The WHO Stepladder
With a clear assessment of the details of the patient’s pain, effective treatment can be rapidly implemented in the ED. In 1986 the WHO developed a 3-step ladder to guide the management of cancer pain. It was originally developed to address nociceptive pain (both somatic and visceral) but has proved useful to some degree for neuropathic pain as well. This simple and well-tested approach provides the clinician with a rational guide for the use of selected analgesics. Today, there is general consensus favoring the use of this model for all pain associated with serious illness. Management is based on the initial assessment of pain and should start at the step that corresponds to the patient’s reported severity based on an NRS (0–10). Mild pain is defined as NRS 1 to 3 (step 1), moderate pain as NRS 4 to 6 (step 2), and severe pain as NRS 7 to 10 (step 3).
Step 1 analgesics
All of the nonopioid analgesics that characterize step 1 of the WHO ladder have a ceiling effect to their analgesia (a maximum dose that, if exceeded, yields no further analgesia). Acetaminophen is an effective step 1 analgesic and may be a useful coanalgesic in many situations, including headache. Its site and mechanism of action are not entirely known. It does not have significant anti-inflammatory effects and is presumed to have a central cyclo-oxygenase (COX) related mechanism. Chronic doses more than 4.0 g/24 h or acute doses more than 6.0 g/24 h are not recommended because they may cause hepatotoxicity. Hepatic disease or heavy alcohol use increases the risk further, and the maximum daily dosage may be reduced to 3.0 g/24 h.
Nonsteroidal anti-inflammatory drugs (NSAIDs, including aspirin) are also effective step 1 analgesics and may be useful coanalgesics. They work, at least in part, by inhibiting COX, the enzyme that converts arachidonic acid to prostaglandins. There are several classes of NSAIDs. Some patients respond better to one class of NSAIDs than to another, and serial “n of 1” trials may be needed to find one that is efficacious for a given patient. NSAIDs with longer half-lives are likely to enhance compliance. NSAIDs can have significant adverse effects. Gastropathy, renal failure, and inhibition of platelet aggregation can occur with any of the nonselective medications, irrespective of the route of administration. The likelihood of these adverse effects will vary among NSAID classes and may be due, in part, to their relative COX-2 selectivity. It is important to ensure adequate hydration and good urine output in patients on NSAIDs to minimize the risk of renal vasoconstrictive injury, including papillary necrosis. Nonselective medications are relatively contraindicated in the setting of significant pre-existing renal insufficiency. NSAIDs may be contraindicated if bleeding is a problem or coagulation or platelet function is impaired. Gastric cytoprotection with misoprostol or omeprazole may be needed in patients with significant risk of gastrointestinal (GI) problems. Significant risk factors include a history of gastric ulcers or bleeding, current nausea/vomiting, protein wasting, cachexia, and advanced age.
There are parenteral forms of NSAIDs now available for use. A new transdermal form of diclofenac is now available in the United States. Its efficacy has been demonstrated in osteoarthritis but has not yet been studied in localized somatic cancer pain. Ketorolac is available in intravenous (IV) or intramuscular formulations. Short-term (<5 days is considered safe in healthy patients) parenteral use of this potent agent provides excellent analgesia, particularly with visceral pain, and avoids the common central nervous system (CNS) side effects of the opioid analgesics. These advantages must be carefully weighed against the GI, renal, cardiovascular, and bleeding risks for each patient before use.
Step 2 and step 3 analgesics
Step 2 and 3 analgesics involve opioid use. The clinician must have an excellent command of opioid pharmacology when using these analgesics. Step 2 agents all have aspirin or acetaminophen present in amounts that limit their dosages to 10 to 12 tablets a day. These agents have a role in moderate pain (4–7/10), but each also has side effects. Codeine derivatives tend to be constipating, and nausea is not infrequent. There are patients who lack the necessary enzyme to convert codeine to its active (morphine) moiety. Therefore, be aware of the need to change to morphine or a step 3 agent if no analgesia is seen. Effective treatment in the ED requires a clear understanding of the pharmacology, clinical setting, and adverse effects of the analgesics prescribed and knowledge of how these may vary from patient to patient.
Principles of opioid therapy
Opioid Pharmacology
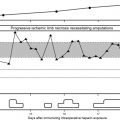
Opioid analgesic effect correlates with maximal plasma concentration (Cmax) ( Table 1 ). Once Cmax is reached, both the maximum analgesic effect and the maximum side-effect profile have been attained. All pure opioids (except methadone) follow first-order kinetics and act in a very similar pharmacologic manner. They reach their time to peak plasma concentration (Tmax) approximately 60 to 90 minutes after oral (including enteral feeding tube) administration, 30 minutes after subcutaneous or intramuscular injection or rectal administration, and 6 to 10 minutes after intravenous injection. They are eliminated from the body in a linear and predictable way, proportional to the dose. They are first conjugated in the liver, and then the kidneys excrete 90% to 95% of the metabolites. Their metabolic pathways do not become saturated. Because of its complicated cytochrome metabolism, methadone does not follow the first-order kinetics and should not be initiated or titrated in the ED without the consultation of the patient’s primary care physician or a specialist in pain or palliative medicine. Each opioid metabolite has a half-life (t½) that depends on its rate of renal clearance. When renal function is normal, codeine, hydrocodone, hydromorphone, morphine, oxycodone, and their metabolites all have effective half-lives of approximately 3 to 4 hours. When dosed repeatedly, their plasma concentrations approach a steady state after 4 to 5 half-lives. Thus, steady-state plasma concentrations are usually attained within a day.
| Route | Time to Maximal Concentration |
|---|---|
| Intravenous | 6–10 min |
| Rectal/subcutaneous | 30 min |
| Oral | 60–90 min |
Opioids and their metabolites are primarily excreted renally (90%–95%). Care should be taken when dosing these agents in patients with renal impairment. The clinician should take care in selecting appropriate agents in patients with renal impairment and be prepared to reduce the dose ( Tables 2 and 3 ). Morphine has 2 principal metabolites: morphine-3-glucuronide and morphine-6-glucuronide. Morphine-6-glucuronide is active and has a longer half-life than that of the parent drug morphine. Consequently, when dehydration or acute or chronic renal failure impairs renal clearance, the dosing interval for morphine must be increased or the dosage size decreased to avoid excessive accumulation of active drug and metabolites. If urine output is minimal (oliguria) or none (anuria), routine dosing should be stopped, and morphine should be administered only as needed. This is particularly important when patients are dying. Renal excretion is somewhat less of a concern with hydromorphone, but fentanyl and methadone are considered the safest choices in renal failure. Opioid metabolism is not as sensitive to hepatic compromise. However, if hepatic function becomes severely impaired, the dosing interval should be increased or the dose decreased.
| Dialyzable | |||
|---|---|---|---|
| Opioid | Renal Failure | Parent Drug | Metabolites |
| Methadone | Appears safe | + | + |
| Fentanyl | Appears safe | +/− | none |
| Morphine | Use with caution/dose adjust | + | + |
| Hydromorphone | + | +/− | |
| Hydrocodone | + | +/− | |
| Oxycodone | Inadequate data | Inadequate data | |
| Codeine | Do not use | Inadequate data | Inadequate data |
| Meperidine | Inadequate data | Inadequate data | |
| Propoxyphene | – | – | |
| Creatinine Clearance | Dose Reduction of Normal Dose |
|---|---|
| >50 mL/min; normal dosing | Normal |
| 10–50 mL/min | 75% dosing |
| <10 mL/min | 50% dosing |
Opioid-Naïve Patients
Patients with severe pain who have never been on opioids will need a trial of short-acting opioids to establish their opioid needs and any possible respiratory depressive effect. Oral agonist opioids are appropriate for severe pain if time and circumstance allow. On an outpatient basis, severe pain may be treated with WHO step 3 analgesics as a reasonable first choice. If an immediate-release oral opioid is selected, and the pain is persistent or nearly so, the medication should be given every 4 hours. Once steady state has been reached, the best possible pain control for the dose will be achieved within a day (4–5 half-lives). The patient should see his or her primary physician within the next 24 to 48 hours, and he or she should be started on long-acting, continuous-release medications with breakthrough doses as needed.
Opioid-Tolerant Patients
Opioid-tolerant patients may come to the ED experiencing oligoanalgesia. They often say that their medications are no longer effective. This can be a function of physiologic tolerance, disease progression, or ineffective use of the medications (for example, taking continuous-release opioids only once per day when they were intended for 12-hour use). Opioid-tolerant patients presenting to the ED with severe pain will often need to have increases made in their baseline opioid dosing to achieve pain control.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree