Superior vena cava syndrome is a common complication of malignancy. The epidemiology, presentation, and diagnostic evaluation of patients presenting with the syndrome are reviewed. Management options including chemotherapy and radiation therapy and the role of endovascular stents are discussed along with the evidence for each of the therapeutic options.
Superior vena cava syndrome (SVCS) is a common complication of malignancy, especially of lung cancer and lymphoma. The frequency of SVCS varies depending on the specific malignancy. Approximately 2% to 4% of all patients with lung cancer develop SVCS at some time during their disease course. The incidence is higher in small cell lung cancer (SCLC), given its predilection for mediastinal involvement and rapid growth; the incidence approaches 10%. SVCS develops in approximately 2% to 4% of non-Hodgkin’s lymphoma (NHL) but is relatively rare in Hodgkin’s lymphoma despite the presence of mediastinal lymphadenopathy. For primary mediastinal large B-cell lymphomas with sclerosis, the incidence has been reported as high as 57% in one series of 30 patients. Together, lung cancer and lymphoma are responsible for over 90% of malignant causes of SVCS. In the modern era, 60% to 90% of cases of SVCS are caused by malignant tumors, with the remaining cases accounted for largely by fibrosing mediastinitis and thrombosis of indwelling central venous devices and/or pacemaker leads. The focus of this article is on the management of malignant causes of SVCS.
Anatomy and physiology
The superior vena cava (SVC) is the major vessel collecting venous return to the heart from the head, arms, and upper torso. Compression of the SVC in malignancy is usually due to extrinsic masses in the middle or anterior mediastinum, right paratracheal or precarinal lymph node stations, and tumors extending from the right upper lobe bronchus. As the tumors increase in size and produce compression of the SVC, there is increased resistance to venous blood flow, which is then diverted through collateral networks that may develop. Collateral vessels that are commonly found include azygos, intercostal, mediastinal, paravertebral, hemiazygos, thoracoepigastric, internal mammary, thoracoacromioclavicular, and anterior chest wall veins. The severity of SVCS is worse if the level of obstruction is below the azygos vein, underscoring the importance of this vessel in providing an alternate route for blood flow. The severity of the obstruction is also dependent on the rapidity of onset of the obstruction. Collateral vessels often take several weeks to dilate sufficiently to accommodate the diverted blood flow of the SVC. The presence of collateral vessels with compression of SVC on computed tomography (CT) is a reliable indicator of the presence of SVCS with a sensitivity of 96% and specificity of 92%.
Presentation
Patients often complain of a variety of symptoms. The most common of these are facial or neck swelling (82%), arm swelling (68%), dyspnea (66%), cough (50%), and dilated chest veins (38%). Patients may also report chest pain, dysphagia, hoarseness, headache, confusion, dizziness, and syncope. Orthopnea is commonly noted, since a supine position will increase the amount of blood flow to the upper torso. Attention should be given to the duration of symptoms, previous diagnosis of malignancy, or previous intravascular procedures for clues to the etiology of the syndrome. In most cases, symptoms develop over the course of several weeks allowing for collateral circulations to develop.
Worrisome signs include stridor, as this is usually indicative of laryngeal edema, as well as confusion and obtundation, since these may indicate cerebral edema. Although SVCS is now known not to be a major threat to life in most clinical scenarios, evidence of respiratory and neurologic compromise can be associated with serious or fatal outcomes. In addition, patients may have other cancer-related symptoms, such as extrinsic compression of major airway by tumor (which may be an alternate explanation for the stridor), hemoptysis, or thrombosis associated with malignant SVCS, which may need to be addressed urgently and may be more life threatening. Patients may also have B symptoms (eg, drenching night sweats, weight loss, or fevers usually associated with lymphomas) or other constitutional symptoms.
In the past, SVCS was considered to be a medical emergency. However, multiple retrospective reviews have shown that this is not the case in the absence of laryngeal/bronchial or cerebral edema. Accurate diagnosis via imaging and biopsy should be obtained, since treatment approaches can vary widely depending on the histology of the malignancy. Staging investigations should be completed before initiating treatment if possible, because a decision will need to be made regarding a definitive curative approach as opposed to a palliative course of treatment.
Although no standardized grading system exists for the evaluation of SVCS, the group from Yale University have recently proposed a classification system for grading the severity of SVCS as asymptomatic (grade 0), mild (grade 1), moderate (grade 2), severe (grade 3), life-threatening (grade 4), or fatal (grade 5). Cerebral edema, laryngeal edema, stridor, and hemodynamic compromise would constitute grade 3 (if mild/moderate) or grade 4 (if significant) SVCS. The authors recommend more urgent treatment be initiated in the presence of grade 3 or 4 symptoms. The proposed system has not been validated but does provide a rational framework of how to approach and triage these patients.
The diagnosis of SVCS is made on the basis of clinical signs and symptoms and confirmed by imaging studies.
Presentation
Patients often complain of a variety of symptoms. The most common of these are facial or neck swelling (82%), arm swelling (68%), dyspnea (66%), cough (50%), and dilated chest veins (38%). Patients may also report chest pain, dysphagia, hoarseness, headache, confusion, dizziness, and syncope. Orthopnea is commonly noted, since a supine position will increase the amount of blood flow to the upper torso. Attention should be given to the duration of symptoms, previous diagnosis of malignancy, or previous intravascular procedures for clues to the etiology of the syndrome. In most cases, symptoms develop over the course of several weeks allowing for collateral circulations to develop.
Worrisome signs include stridor, as this is usually indicative of laryngeal edema, as well as confusion and obtundation, since these may indicate cerebral edema. Although SVCS is now known not to be a major threat to life in most clinical scenarios, evidence of respiratory and neurologic compromise can be associated with serious or fatal outcomes. In addition, patients may have other cancer-related symptoms, such as extrinsic compression of major airway by tumor (which may be an alternate explanation for the stridor), hemoptysis, or thrombosis associated with malignant SVCS, which may need to be addressed urgently and may be more life threatening. Patients may also have B symptoms (eg, drenching night sweats, weight loss, or fevers usually associated with lymphomas) or other constitutional symptoms.
In the past, SVCS was considered to be a medical emergency. However, multiple retrospective reviews have shown that this is not the case in the absence of laryngeal/bronchial or cerebral edema. Accurate diagnosis via imaging and biopsy should be obtained, since treatment approaches can vary widely depending on the histology of the malignancy. Staging investigations should be completed before initiating treatment if possible, because a decision will need to be made regarding a definitive curative approach as opposed to a palliative course of treatment.
Although no standardized grading system exists for the evaluation of SVCS, the group from Yale University have recently proposed a classification system for grading the severity of SVCS as asymptomatic (grade 0), mild (grade 1), moderate (grade 2), severe (grade 3), life-threatening (grade 4), or fatal (grade 5). Cerebral edema, laryngeal edema, stridor, and hemodynamic compromise would constitute grade 3 (if mild/moderate) or grade 4 (if significant) SVCS. The authors recommend more urgent treatment be initiated in the presence of grade 3 or 4 symptoms. The proposed system has not been validated but does provide a rational framework of how to approach and triage these patients.
The diagnosis of SVCS is made on the basis of clinical signs and symptoms and confirmed by imaging studies.
Evaluation
Physical examination should document the extent of facial, neck, and/or arm swelling, elevation of neck veins, the extent of collateral veins on the chest, and any evidence of respiratory compromise. Facial swelling and plethora are typically exacerbated when patient is supine; the resultant cyanosis can be quite dramatic. Particular attention should be given to any palpable nodes, as they may provide an easily accessible site for tissue biopsy. Routine blood work should be obtained, including complete blood counts, renal function, and liver enzymes. Abnormalities in blood work may indicate other possible sites of biopsy, such as bone marrow or liver lesions, and may influence the subsequent therapy.
Imaging Studies
The majority of patients will have an abnormal chest radiograph (84%), with the most common findings being mediastinal widening (64%) and pleural effusion (26%). Fig. 1 is an example of a chest radiograph from a patient with SVCS. The most useful imaging study is computed tomography (CT) of the chest with contrast (needed to evaluate the SVC). CT imaging allows the level and extent of the blockage to be defined as well as an evaluation of collateral pathways of drainage. It also permits identification of the cause of the obstruction, since a malignant mass is responsible for up to 90% of SVCS. Common findings on CT include enlarged paratracheal lymph nodes with or without additional lung or pleural abnormalities. A classic example of SVCS is shown in Fig. 2 , where contrast clearly delineates compression of the SVC and the development of collateral vessels.
Venography is primarily used if an interventional stent is planned. Radionuclide Tc-99 m venography fails to provide the diagnostic information that is supplied by chest CT regarding location and characteristics of extrinsic masses. However, this technique can be useful for identifying thrombotic obstructions within the SVC. Magnetic resonance imaging may be useful for patients who cannot tolerate CT contrast for any reason to assess mediastinal veins.
In addition to imaging of the chest, a full diagnostic workup for the suspected cancer may be appropriate either at this time or after the tissue diagnosis is obtained. For lung cancer, this typically includes imaging of the abdomen, brain, and bone; for lymphomas, this includes imaging of the abdomen and pelvis, possibly a bone marrow biopsy and a gallium and/or fluorodeoxyglucose positron emission tomographic scan, if appropriate.
Diagnostic Interventions
A tissue diagnosis is necessary to confirm the presence of a malignancy. In the absence of acute airway compromise or progressive neurologic decline from cerebral edema, initiation of therapy before obtaining a diagnosis is unwarranted given only infrequent reports of mortality from SVCS in multiple series. However, the diagnostic workup should be expedited as patients may deteriorate quickly if collateral vessels are not well established. The importance of a proper diagnosis and staging of the patient cannot be overstressed. The treatment approaches vary widely depending on the type of malignancy present and whether an attempt will be made at definitive curative treatment as opposed to palliative approaches. Interventions such as radiation, chemotherapy, and/or steroids may obscure a histologic diagnosis at a later date. Radiation in particular can obscure a diagnosis in up to 42% of biopsy specimens obtained from the irradiated area after treatment.
Careful clinical assessment of peripheral sites, such as supraclavicular nodes, that are easily accessible must be made before proceeding to more invasive procedures, such as bronchoscopy, mediastinoscopy, or endobronchial ultrasound guided biopsies (EBUS). Pleural effusions are also commonly found and are often accessible to thoracocentesis, although the diagnostic yield may be suboptimal. Bronchoscopy has a diagnostic yield of 50% to 70% (depending on the presence of a centrally located lung mass), and transthoracic needle aspiration has a yield of 75%, whereas mediastinoscopy has a diagnostic yield of 90% to 100% in determining the cause of SVCS. The risks associated with mediastinoscopy, predominantly bleeding and infection, are in the order of 0% to 7% in selected series. No specific data exist with regard to the use of EBUS in obtaining a diagnosis in patients with SVCS, although randomized data suggest that EBUS is superior to conventional transbronchial needle aspiration in obtaining a diagnosis should mediastinoscopy be unavailable.
Management
Management of superior cava syndrome due to malignancy depends on the etiology of the cancer, the extent of the disease, the severity of symptoms, and the prognosis of the patient. Median life expectancy in patients with SVCS is approximately 6 months with a range of 1.5 to 9.5 months; however, estimates vary widely and are dependent on the underlying malignant condition. Intervention needs to consider both treatment of the cancer and relief of the symptoms of the obstruction. Treatment of the cancer may be directed with curative intent or for palliation of symptoms alone. The intent of treatment is not always immediately clear, and therapy may need to be initiated before a full staging workup. For these reasons, the physician may wish to allow for a flexible treatment approach that would allow for conversion from a palliative approach to definitive management of the disease as the patient’s status improves.
Data from randomized trials are scarce, and most evidence guiding treatment decisions are from case series. The treatment options include supportive measures, RT, chemotherapy, and stent insertion. Surgery is virtually never an option, as the presence of SVCS almost always signifies unresectable tumor within the mediastinum. Although there may be a role for surgery after induction treatment for selected patients with mediastinal nodal disease from lung cancer, it would be unlikely that a patient who presented with SVCS would have potentially resectable nodal disease. However, if in doubt, surgical input as part of multidisciplinary assessment may be sought, although the most efficient approach would be to refer to a specialist who is most likely to initiate appropriate therapy for the patient.
Interventions for Symptom Relief
Initial interventions should be directed toward supportive care and medical management. Although there are no data documenting the effectiveness of such maneuvers, these measures can be performed with minimal risk and may provide initial relief of the symptoms of SVCS. Oxygen support and attempts to minimize the hydrostatic pressure in the upper torso, such as fluid limitation, head elevation, and diuretics, may be useful in reducing symptoms in the short term.
Recognition of life-threatening symptoms suggestive of airway compromise and/or cerebral edema is essential. Evidence of severe airway compromise, such as stridor, accompanied by findings of laryngeal edema or tracheal obstruction on CT should be addressed emergently with interventions to protect the airway, such as an endotracheal tube. Management of cerebral edema associated with SVCS has not been described in the literature. Standard resuscitation techniques should be considered, such as head elevation, hyperventilation, and use of osmotic diuretics such as mannitol, if the patient presents with symptoms suggestive of cerebral edema. Imaging for an intracranial cause of cerebral edema should be obtained as well. In both cases, the patient should be hospitalized, monitored closely, and treated urgently to relieve the SVCS.
Steroids are often used as a temporary measure to reduce edema and associated symptoms, but there is an absence of data documenting the effectiveness and dose of steroids in this setting. There is also a risk of obscuring the tissue diagnosis, especially if lymphoma is suspected. In one retrospective review of 107 patients, the use of steroids and diuretics or neither therapy had a similar rate of clinical improvement of 84%. However, in a symptomatic patient in whom airway edema is believed to contribute to the symptoms, steroids can be an effective intervention. No standard dosing or guidelines exist with regard to the dose of steroids to be used. At our institution, dexamethasone 4 mg orally twice a day or 4 mg orally four times a day is often initiated.
It should be emphasized that steroids should only be used as an initial temporizing measure. Chronic use of high doses of steroids can result in significant side effects, including facial swelling (cushingoid facies), and promote fluid retention, both of which could aggravate the symptoms of SVCS. Prolonged use of high doses of corticosteroids can also complicate assessment of therapeutic effectiveness, as the side effects of steroids can overlap with the symptoms of SVCS.
One should also be acutely aware that thrombosis may contribute to the severity of the SVCS as well as pose a major threat to life should pulmonary embolus or further thrombotic events occur. The incidence of thromboembolic events in patients with malignant SVCS has been reported as high as 38% in a group of prospectively followed patients. There are less data guiding the decision to anticoagulate patients with malignant SVCS (without documented thrombus), with only an older, small, randomized trial that showed no difference in survival between patients anticoagulated versus those who were not. Unfortunately, this trial did not report the incidence of pulmonary embolism. In summary, there is no evidence to support routine anticoagulation in patients with malignant SVCS in the absence of thrombosis. It appears reasonable to anticoagulate patients with demonstrable thrombus on imaging.
After a tissue diagnosis has been obtained and the extent of the disease has been determined, a decision should be made to address control of the malignant process in either a curative fashion or palliatively. Radiation, chemotherapy, or stent placement, or a combination of these modalities will play a role as the definitive intervention of SVCS, depending on the sensitivity of the specific tumor.
Radiation
Radiotherapy (RT) is an effective modality in the treatment of SVCS due to malignancy. A systemic review of the literature, conducted by Rowell and Gleeson, documented that radiation was effective at providing overall relief in approximately three-quarters of SVCS due to SCLC and in two-thirds of SVCS due to non-small cell lung cancer (NSCLC).
The rapidity of response is in the range of 7 to 15 days but may be seen as early as 72 hours after initiation of therapy. Relative contraindications to RT include previous treatment with radiation in the same region, certain connective tissue disorders such as scleroderma, and known radioresistant tumor types (eg, sarcoma). Response rates in the literature are often clinical, and there can be a significant discordance with objective response rates as measured by imaging. In one report, evaluation with serial venography documented complete relief in 31% and partial relief in 23% for a total objective response rate of 54%, which is somewhat lower than clinically reported response rates.
The radiation treatment plan can vary based on the histology of the tumor as well as the intent of treatment. For example, a definitive course of radiation for SCLC can involve 3 to 6 weeks of daily or twice-a-day treatments (eg, 40 Gy in 15 daily fractions, 50 Gy in 25 fractions, 60 Gy in 30 fractions, or 45 Gy at fraction sizes of 1.5 Gy twice a day over 3 weeks). In NSCLC, definitive treatment takes 6 to 7 weeks to administer in daily fractions of 2 Gy. Palliative treatments are typically administered over a course of 1 to 2 weeks with larger fraction sizes of 3 Gy to 5 Gy (eg, 20 Gy in 5 fractions, 30 Gy in 10 fractions), with the goal of achieving a more rapid response by using larger daily doses. Abbreviated treatments of 2 6-Gy fractions (12 Gy/2 fractions) have been reported to be effective in older patients with poorer performance status.
Radiation treatment planning usually involves CT-based simulation for designing RT fields. The fields should encompass the gross tumor volume and involved nodal regions and attempt to shield involved normal organs in the proximity of the tumor, particularly lung and esophagus, to minimize the risk of side effects. The size and configuration of the fields may be altered during the treatment course, as patients may improve symptomatically, and tumor may shrink to allow for a higher curative dose to be delivered.
Careful assessment of the patient is needed during the radiation treatment to monitor for side effects as well as progression of radioresistant tumors necessitating alternative interventions, such as stent placement and/or a protective airway if symptoms worsen. Occasionally, worsening of symptoms can be due to development of a thrombus, in which case vascular imaging and anticoagulation should be considered.
Chemotherapy
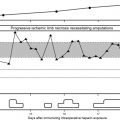
Lymphomas, SCLCs, and germ cell tumors are widely regarded as chemotherapy-sensitive tumors, with high rates of response and quick onset of tumor shrinkage. Thus, chemotherapy is often used as the initial treatment for SVCS from such tumors. RT alone can be used and can provide prompt responses as well for these malignancies; but it usually yields poorer long-term results and is used only in patients who are not candidates for chemotherapy. Chemotherapy can relieve the symptoms of SVCS in up to 80% of patients with NHL and 77% with SCLS. The response rate of relief from SVCS treated with chemotherapy is similar to that of RT and ranges from 7 to 15 days. Fig. 3 demonstrates the response of a patient with a chemotherapy-sensitive tumor. After several cycles of chemotherapy, the patient recovered patency of his SVC with good symptomatic relief and reduction in tumor burden.