Fig. 3.1
(a, b) Comparison of two craniocaudal (CC) views: nipple in profile (a) versus nipple not in profile, with the nipple mimicking a retroareolar mass (b)
Box 3.1 Mammography Film Labeling
Patient’s full name |
Unique patient identification number |
Name and address of facility |
Mammography unit |
Date of examination |
Laterality and view |
Technologist’s initials |
Screening Mammography
Screening mammograms are performed on asymptomatic women who have periodic mammograms to detect early breast cancer. The American College of Radiology (ACR) and other organizations recommend screening mammography for asymptomatic women 40 years of age and to continue annually. Screening mammography can be started before age 40 for high-risk women [5, 6]. However, there is controversy concerning the start of screening mammography as well as its frequency, which is discussed in other chapters. The screening mammogram is generally a two-view study. These standard views are described next.
Standard Mammographic Projections
Two projections are the basic components of the standard routine mammogram: the craniocaudal (CC) and the mediolateral oblique (MLO) views (Fig. 3.2a–d). This allows for maximum visualization of the breast tissues while obtaining the information required in order to gain a three-dimensional understanding of the visualized structures. This three-dimensional understanding is paramount to accomplish two objectives: (1) minimize the patient recall that would result from normal overlapping structures if only a single projection was obtained and (2) improved breast cancer detection by increasing the amount of breast tissues being imaged [5]. Additional views may be necessary for evaluation of women with breast implants (standard views as well as implant displaced or pushback views).
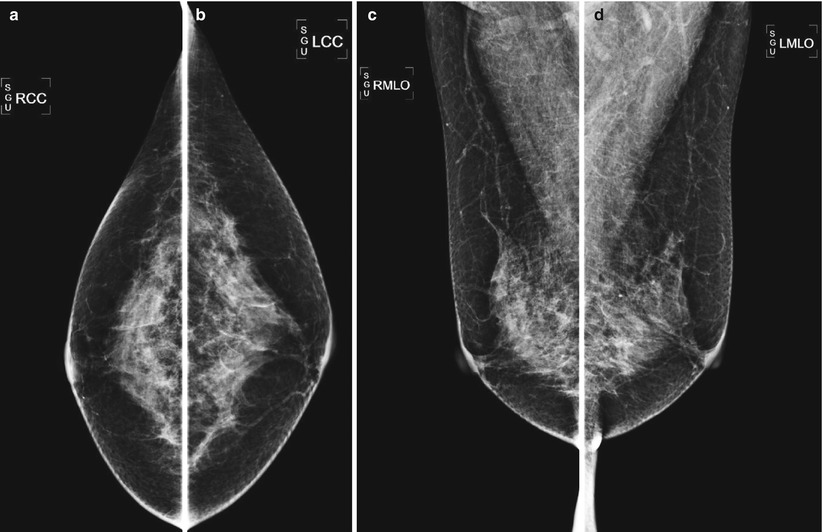
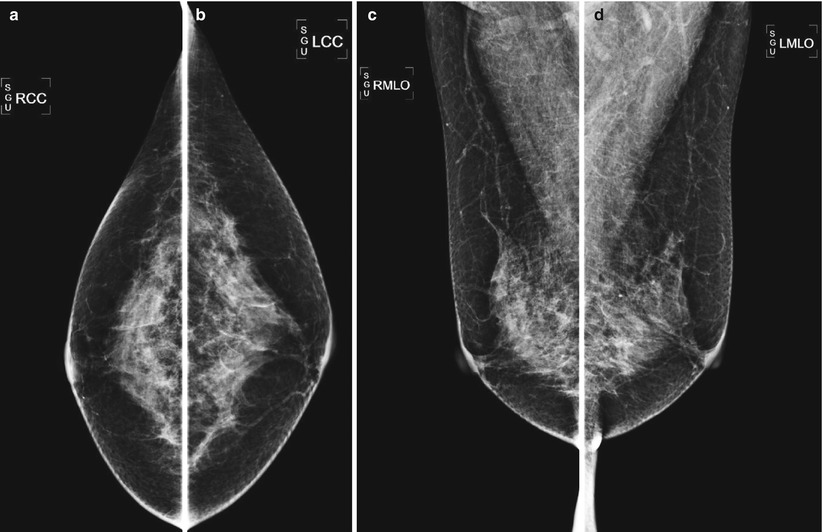
Fig. 3.2
(a–d) Standard images obtained for screening mammography
Craniocaudal (CC) View
An adequately positioned CC view maximizes the amount of tissue imaged (Fig. 3.3). Every effort should be made by the technologist in order to include all the medial and lateral breast tissues on the CC view. This is a more challenging task than on the MLO view since more breast tissue can be included in the latter as a result of the normal chest wall anatomy. The distance from the mid-nipple to the most medial and lateral skin line should be about equal. Every effort should be made by the technologist so that the medial tissues are included on the CC view. This may result in limited visualization of the lateral tissues. Additional imaging occasionally may be necessary as determined by the mammography technologist to ensure adequate visualization of all the breast tissues. The most frequent additional imaging needed is an exaggerated laterally CC view (also known as XCCL) so that there is visualization of fat behind the lateral portion of the fibroglandular tissues (Fig. 3.4a, b).
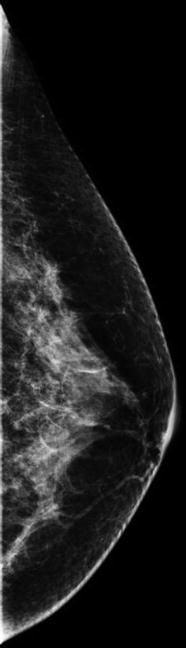
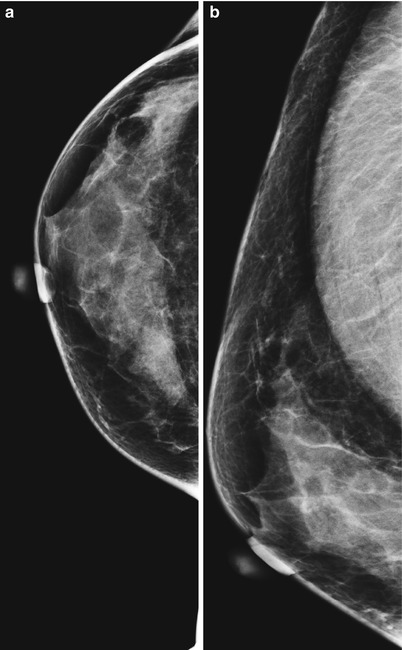
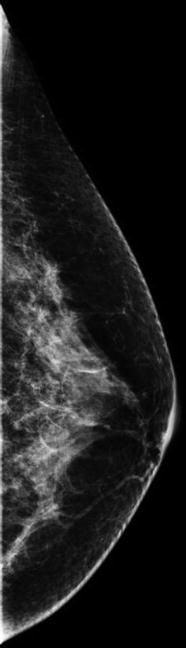
Fig. 3.3
Technically adequate craniocaudal (CC) view of both breasts
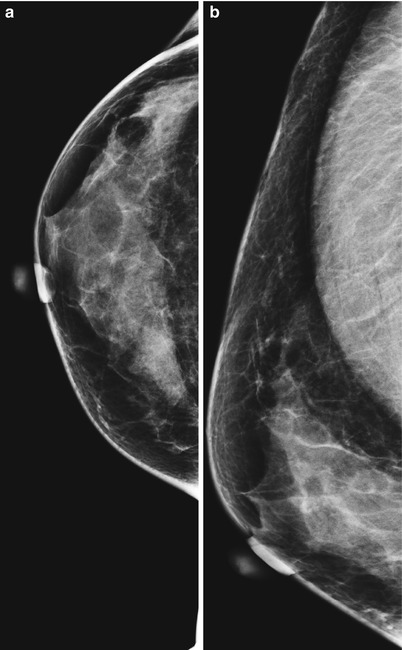
Fig. 3.4
(a, b) Example of standard craniocaudal (CC) view and exaggerated craniocaudal view laterally (XCCL) images, respectively. Note the increased amount of lateral breast tissues imaged
To determine the adequacy of the amount of breast tissue seen on the craniocaudal (CC) view, one should measure the distance starting from just underneath the nipple to the posterior edge of the image or the anterior edge of the pectoralis muscle in this projection. This distance is also known as the posterior nipple line (PNL). This distance should not differ by more than one centimeter when compared to the distance from just underneath the nipple to the pectoralis muscle at the level of the nipple on the mediolateral oblique (MLO) projection (Fig. 3.5a, b).
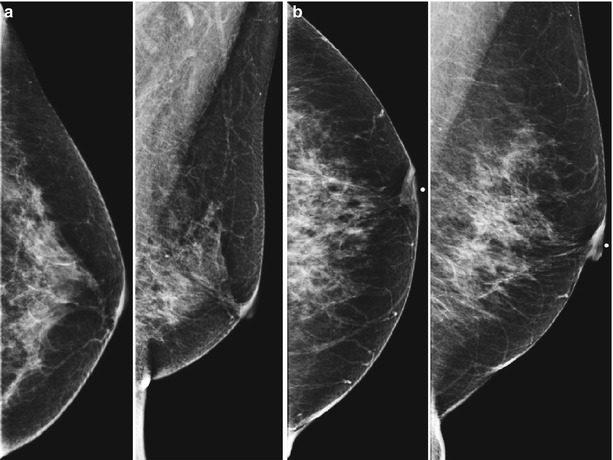
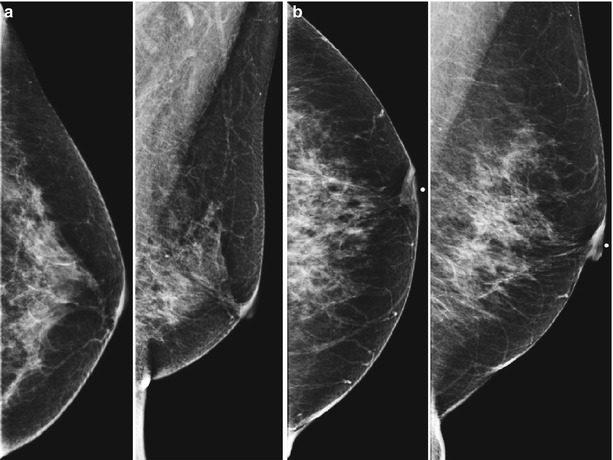
Fig. 3.5
(a) Adequate posterior nipple line (PNL) measurement differences between the craniocaudal (CC) and mediolateral oblique (MLO) views. The difference in this distance between the two views is less or equal to 1 cm. (b) Inadequate posterior nipple line (PNL) measurement differences between the craniocaudal (CC) and mediolateral oblique (MLO) views. The difference in this distance between the two views is greater than 1 cm. Nipple markers are present in these images
Mediolateral Oblique (MLO) View
An adequately positioned MLO view allows visualization of the tissues from the inframammary fold (IMF) in the upper abdominal wall to the axillary tail. The pectoralis muscle should extend in a convex curve obliquely in the upper half of the image and extend inferiorly to or below the level of the nipple while tapering during this course. This maximizes the amount of breast tissue that is imaged resulting in improved visualization and resultant cancer detection. The x-ray tube should be moved so that the detector plane is directly paralleling the muscle fibers. This way, pulling the breast away from the chest wall and achieving effective compression is easier for the imaging technologist and more comfortable for the patient. The degree of x-ray tube rotation will vary as appropriately from patient to patient depending on the different body habitus of the individual imaged. As mentioned earlier, the inframammary fold (IMF) should be included on the image. In particular, the inferior aspect of the breast and the upper abdomen do not overlap, opening up this area (Fig. 3.6).
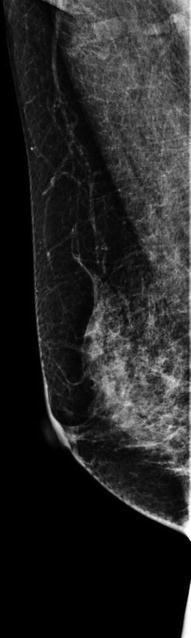
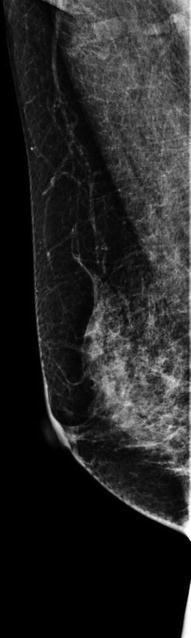
Fig. 3.6
Technically adequate right mediolateral oblique (MLO) view
One can measure the length of the posterior nipple line (PNL) from underneath the nipple to the pectoralis muscle. This line should be perpendicular to the pectoralis muscle line. The length of the PNL can be utilized, and the adequacy of the amount of breast tissue included in the craniocaudal (CC) projection (Fig. 3.7a, b).
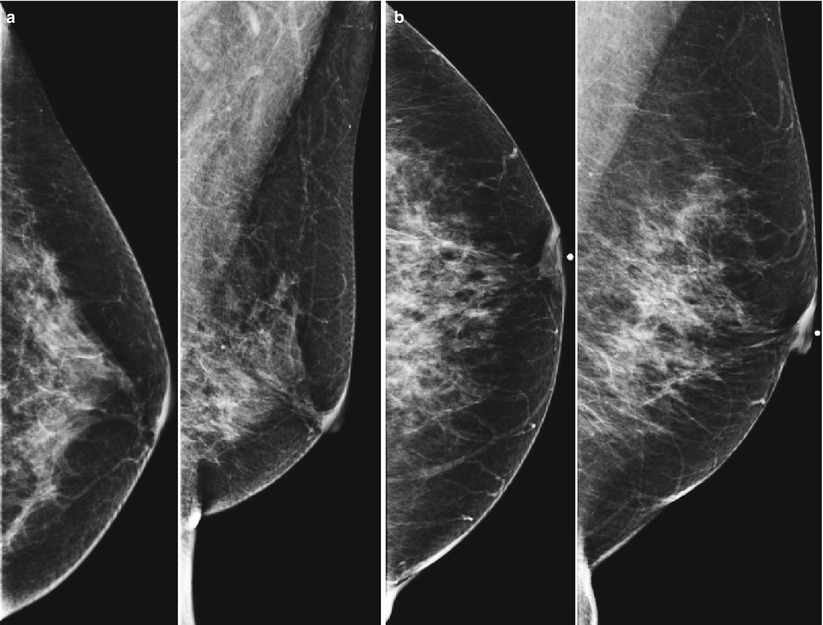
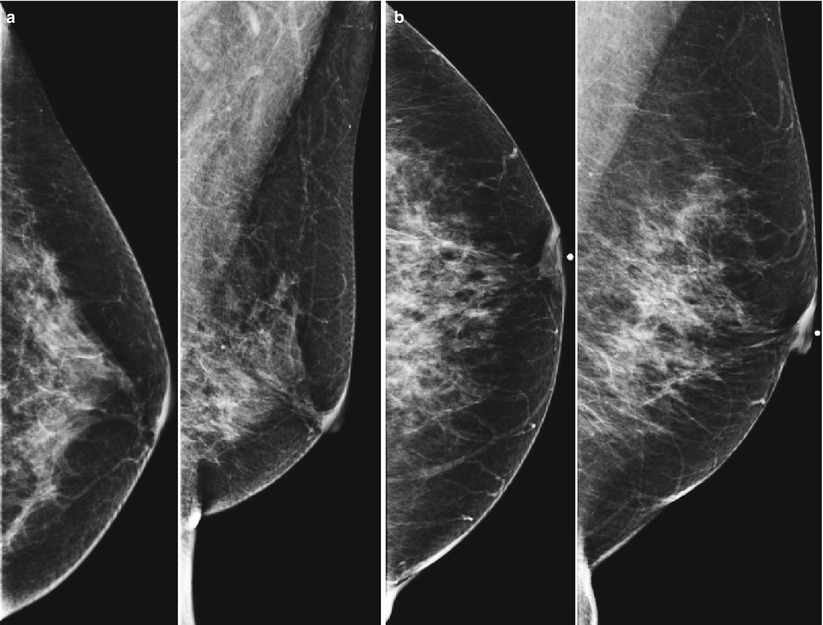
Fig. 3.7
(a) Adequate posterior nipple line (PNL) measurement differences between the craniocaudal (CC) and mediolateral oblique (MLO) views. The difference in this distance between the two views is less or equal to 1 cm. (b) Inadequate posterior nipple line (PNL) measurement differences between the craniocaudal (CC) and mediolateral oblique (MLO) views. The difference in this distance between the two views is greater than 1 cm. Nipple markers are present in these images
Additional Views
Since every individual has a different anatomy, there will likely be breast tissues that are not included in the standard projections, particularly the more mobile upper inner quadrant. Additional projections can be performed on a case-by-case basis according to the different anatomy of the patients being imaged. Additional views can be obtained to maximize visualization of a region of interest. Some examples include:
Lateral tissues: Exaggerated craniocaudal view laterally (XCCL) or the axillary tail (AT) view (Fig. 3.8a, b)
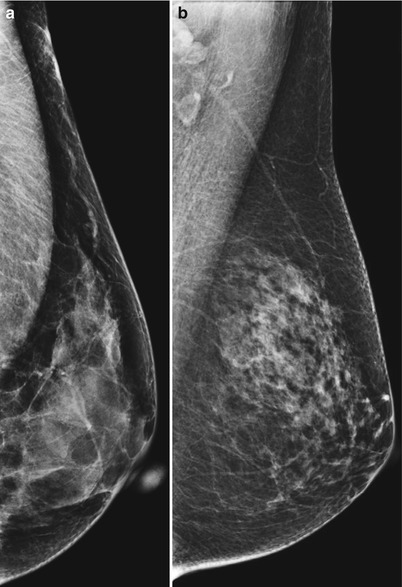
Fig. 3.8
(a) Example of improved visualization of the lateral tissues using an exaggerated craniocaudal view laterally (XCCL). (b) Example of improved visualization of the lateral tissues using an axillary tail view
Medial tissues: Exaggerated craniocaudal view medially (XCCM), cleavage (CV) view, or mediolateral (ML) view (Fig. 3.9a, b)
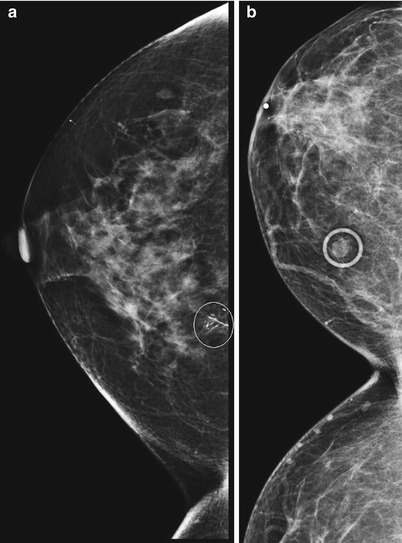
Fig. 3.9
(a) Example of improved visualization of the medial tissues using an exaggerated craniocaudal view medially (XCCM). In this example, the circled highly suspicious calcifications are biopsy-proven ductal carcinoma in situ (DCIS). (b) Example of improved visualization of the medial tissues using a cleavage view
Superior tissues: Caudocranial view
These will be discussed in more detail in the section later in this chapter titled “Additional views.”
Diagnostic Mammography
Overview
There are numerous indications to perform diagnostic mammograms. These include:
1.
Signs and/or symptoms indicated by the patient and/or the health care provider. Examples include palpable complaints, nipple or skin changes (retraction, induration), nipple discharge, or axillary adenopathy. The ACR guidelines also include persistent focal areas of pain or tenderness. In the author’s (ABW) 35 years of practice in mammography, this symptom is rarely secondary to breast cancer.
2.
Further evaluation of a finding noted on screening mammography.
3.
Short-interval follow-up of a probably benign mammographic finding as described by the ACR Breast Imaging Reporting and Data System (BI-RADS®) to assess stability [7].
4.
Patients treated for breast cancer. These patients, if asymptomatic, can undergo screening or diagnostic mammography [8].
5.
Examinations requiring direct supervision by the radiologist such as consultation, direct breast examination, or directed additional views.
Additional Views
Spot Compression Views
Another technique that is employed in the work-up of breast lesions is obtaining spot views. The effective pressure generated in standard imaging is less than on spot imaging, as the pressure generated on standard imaging covers a larger area by using a larger paddle. When a smaller compression paddle is used, the pressure is then applied over a smaller area. This serves a dual purpose: (1) it spreads overlapping structures that may form a “pseudomass” on the original images, and (2) it helps to better define the morphological features of the lesion of interest.
The preferred compression device is the round spot compression paddle. This device is utilized for mid to large masses and small area of asymmetries (Fig. 3.10a). The larger square spot compression devices are best utilized for mid to large areas of asymmetry and very large masses (Fig. 3.10b). The smaller round spot compression device provides better compression with better resolution of the area of interest.
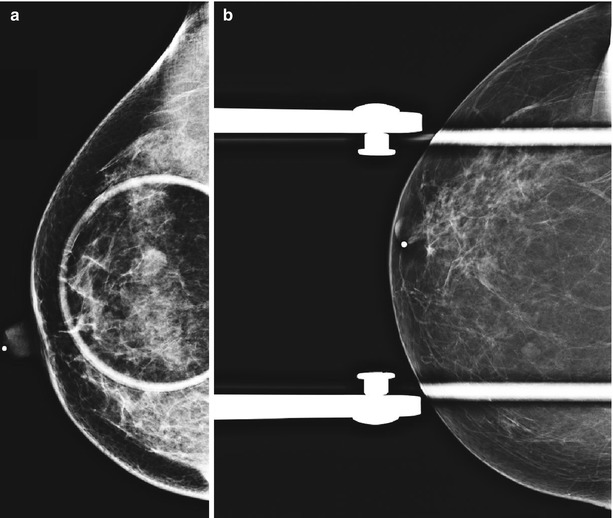
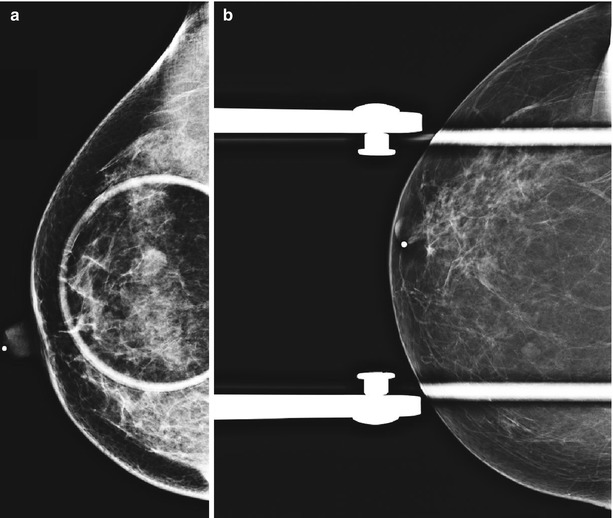
Fig. 3.10
(a, b) The round spot compression paddle (a) provides better characterization of the morphological features of the lesion of interest when compared to the larger square compression paddle (b). Images correspond to different cases, as in our institution we do not routinely use the larger square paddle
Magnification Views
Magnification mammography is most used for the analysis of morphology and distribution of microcalcifications. However, it can also be used in the analysis of the margins and internal architecture of masses.
The breast is elevated off the normal platform to obtain 1.5–2x magnification of the area of concern. Standard mammography uses a small focal spot size (traditionally, a nominal 0.4 mm focal spot). By using a smaller focal spot size (specifically, a 0.2 mm for 1.5× magnification and smaller) and elevating the breast above the receptor, magnification mammography can be performed. This allows for improved resolution due to a reduction in scatter and noise. This improved resolution comes at a cost, which are a higher patient dose as well as the exposure time. This can result in increased motion blur, which degrades the examination. Therefore, magnification views should be used appropriately realizing that what is obtained in increased resolution may be nullified by motion artifact from the longer exposure time.
Both small round (Fig. 3.11a, b) and larger square (Fig. 3.11c, d) magnification devices can be used. Again, the smaller round spot device provides better resolution of the area of interest, as seen in the corresponding figures.
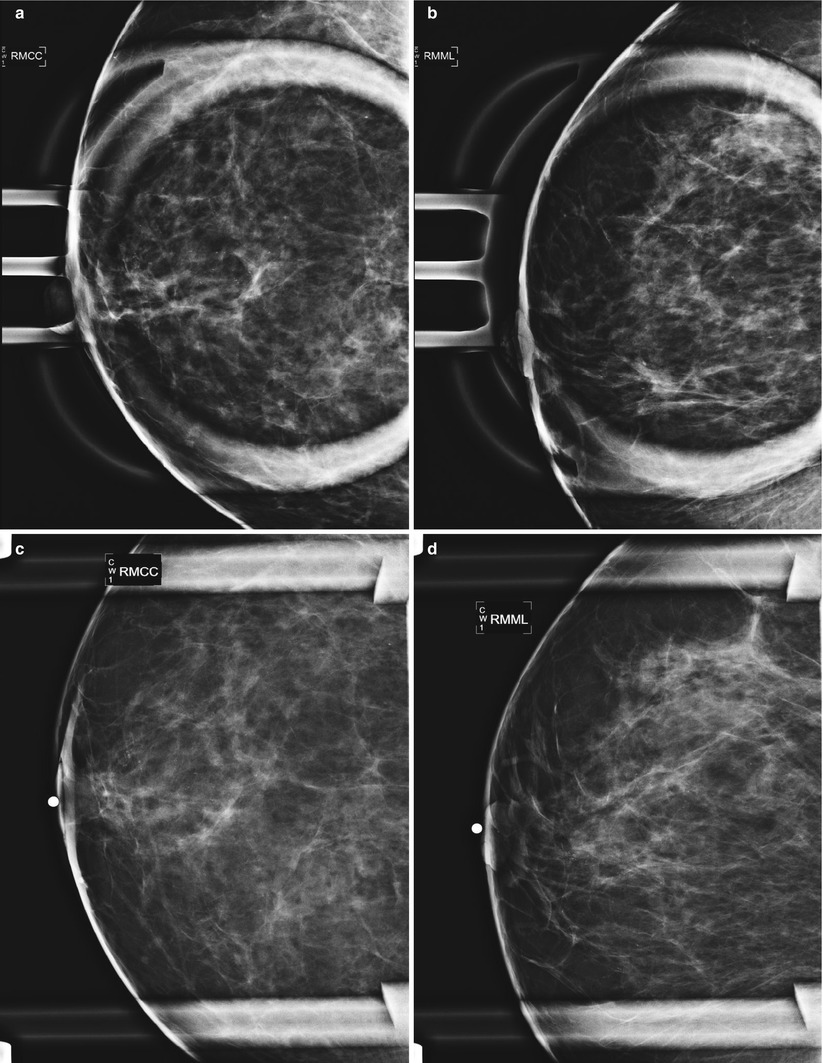
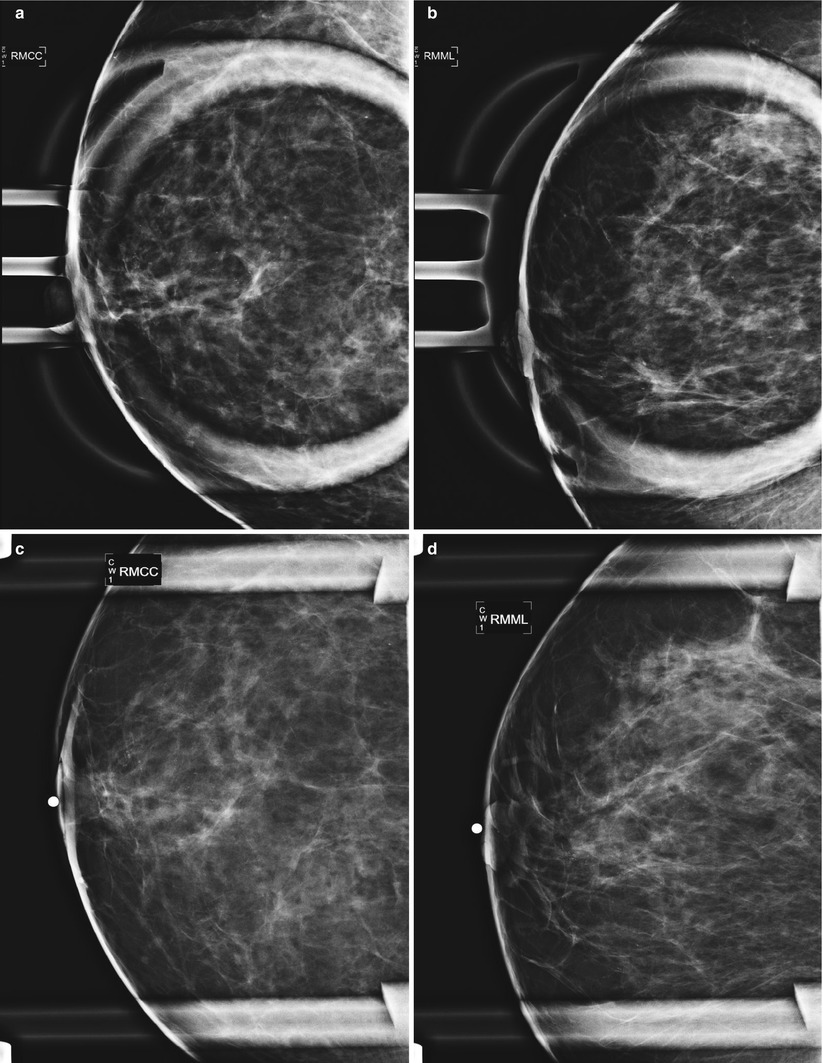
Fig. 3.11
(a–d) The small round magnification paddle (a, b) provides better visualization of the microcalcifications versus the larger square paddle (c, d). The use of the smaller magnification paddle aids in improved characterization of their morphology and distribution
Mediolateral (ML) and Lateromedial (LM) Views
The mediolateral (ML) or lateromedial (LM) views are utilized to better evaluate the morphology of lesions and assist in localizing lesions (Fig. 3.12a, b). The decision as to which view to use is mainly based on the medial or lateral location of a finding on the CC view so the abnormality is placed closest to the image receptor. If the area of concern is located in the lateral aspect of the breast, then a mediolateral (ML) view is obtained, and if it is located in the medial aspect, then a lateromedial (LM) view is obtained.
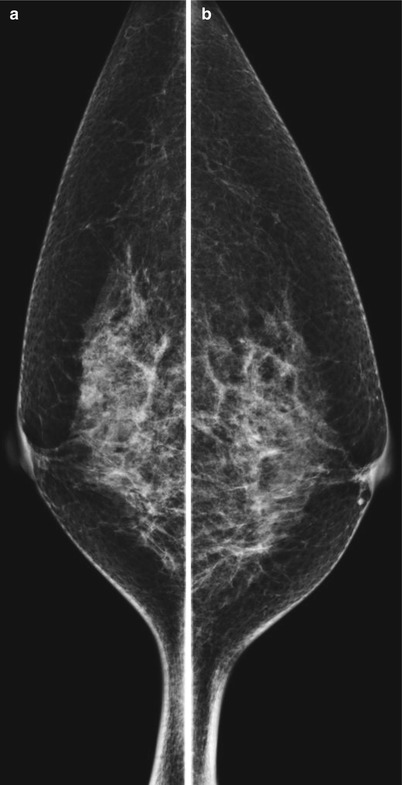
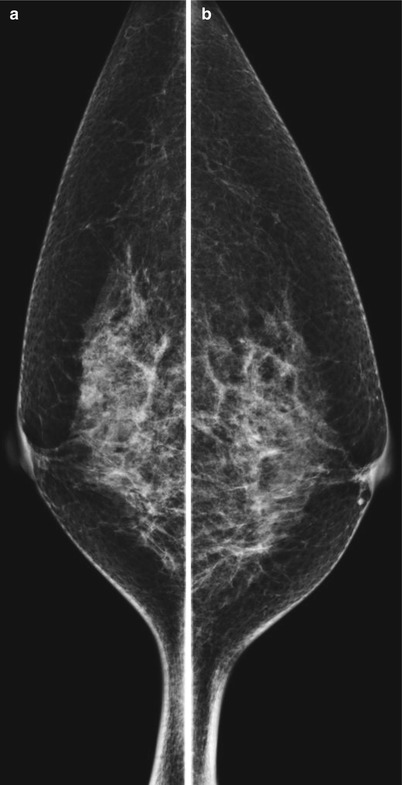
Fig. 3.12
(a, b) Technically adequate bilateral mediolateral (ML) views
There is better compression on the ML or LM views than the MLO view because the pectoralis muscle is not included in the image. The ML or LM views also allow for more accurate prediction of the location of a mass or calcifications in the superior or inferior aspect of the breast by measuring its distance from the nipple. This is particularly beneficial when one is correlating a mammography finding to perform a focused breast ultrasound examination or when performing a second-look ultrasound in anticipation of biopsy of a breast magnetic resonance imaging (MRI) finding.
Another use of the ML or LM views is in the evaluation of microcalcifications. These are particularly useful for making the diagnosis of milk of calcium (MOC), which have a distinctive appearance in the lateral views versus on the CC view and constitute a benign process. This entity is discussed in more detail in other chapters in this book.
In addition, if a lesion is seen on the MLO view and not on the CC view, one can further help localize the lesion by performing an ML or LM view. This concept is discussed in more detail under the section “Localization Techniques” found later in this chapter.
Exaggerated Craniocaudal View Laterally (XCCL View)
This view is to further evaluate lesions that are in the extreme lateral/axillary part of the breast that are not seen or partially seen on the routine CC view. On the XCCL view, the nipple is off center and located in the medial aspect of the view with extra tissue visualized in the lateral aspect of the breast (Fig. 3.13a, b). This view is commonly utilized as it better visualizes lesions where cancer occurs more frequently, the upper outer quadrant of the breast. One can also utilize this view with magnification techniques to better evaluate small masses and calcifications.
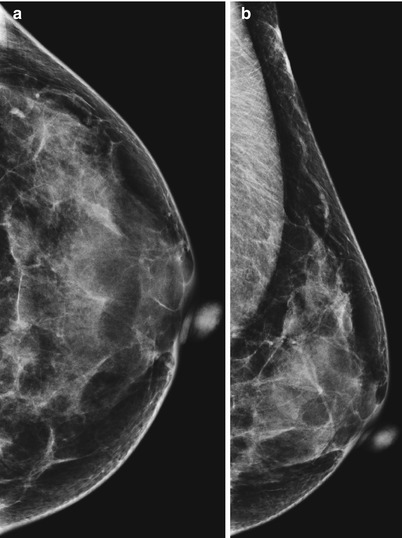
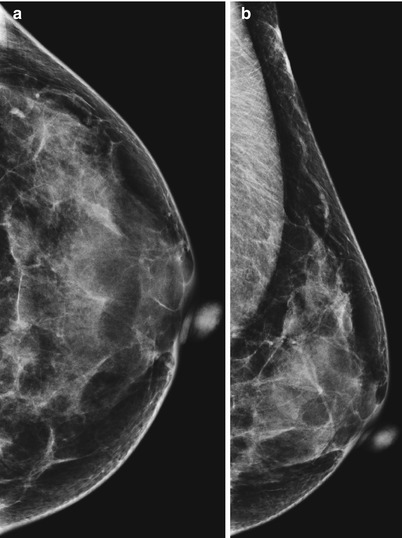
Fig. 3.13
(a, b) Example of exaggerated craniocaudal view laterally (XCCL). Note the increased amount of lateral breast tissues imaged on the XCCL view (b) compared to the CC view (a)
Exaggerated Craniocaudal View Medially (XCCM View)
This view is used to further evaluate lesions that are located in the extreme medial part of the breast and therefore not seen or partially seen on the routine CC view. On the XCCM view, the nipple is off center and located in the lateral aspect of the view with extra tissue visualized in the medial aspect of the breast (Fig. 3.14).
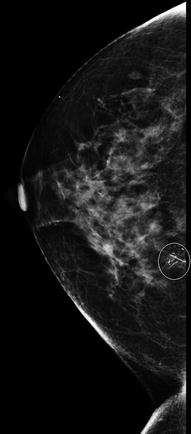
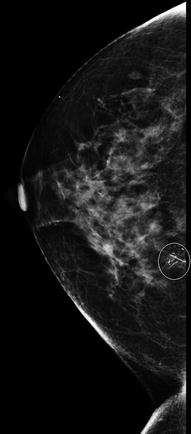
Fig. 3.14
Example of exaggerated craniocaudal view medially (XCCM). Note the increased amount of medial breast tissues imaged. In this example, the circled highly suspicious calcifications are biopsy-proven ductal carcinoma in situ (DCIS)
Cleavage View
The cleavage (CV) view is an alternate method to the XCCM view for imaging the most medial aspect of both breasts (Fig. 3.15).
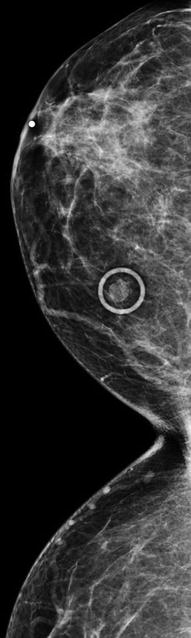
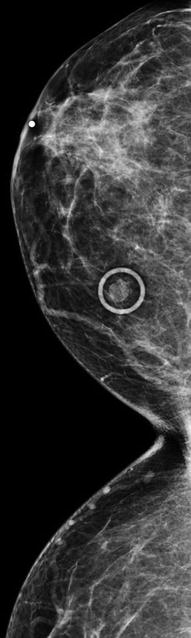
Fig. 3.15
Example of cleavage view. This is an alternate method to the XCCM view for imaging the most medial aspect of both breasts
Rolled Medial and Rolled Lateral Views
The rolled medial CC and/or rolled lateral CC views (also known as RM or RL views) are utilized to further evaluate a finding seen only on the CC view (Fig. 3.16a) and not the MLO or lateral views (Fig. 3.16b, c). The finding may represent a “pseudomass” from overlapping tissue or a real mass that is not visualized on the MLO or lateral views. If the finding is secondary to a “pseudomass” from overlapping tissue, the process of rolling the breast medially (Fig. 3.16d) and laterally (Fig. 3.16e) will separate the overlapping tissue and the mass disappears. One can add spot compression views to the full rolled views to further evaluate the questionable finding (Fig. 3.16f).
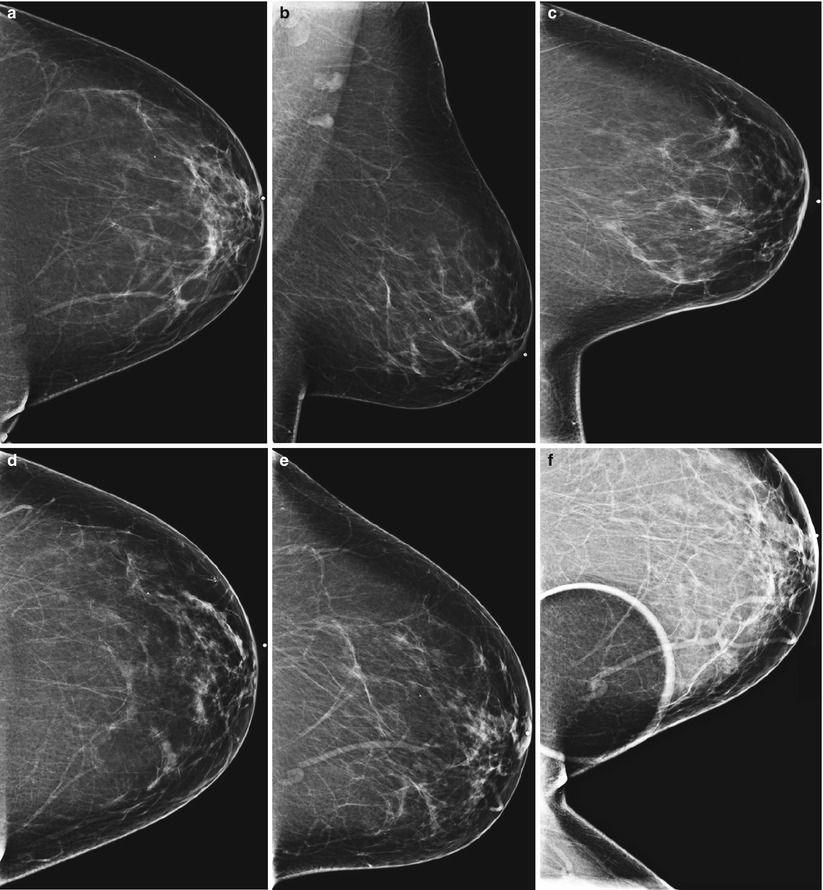
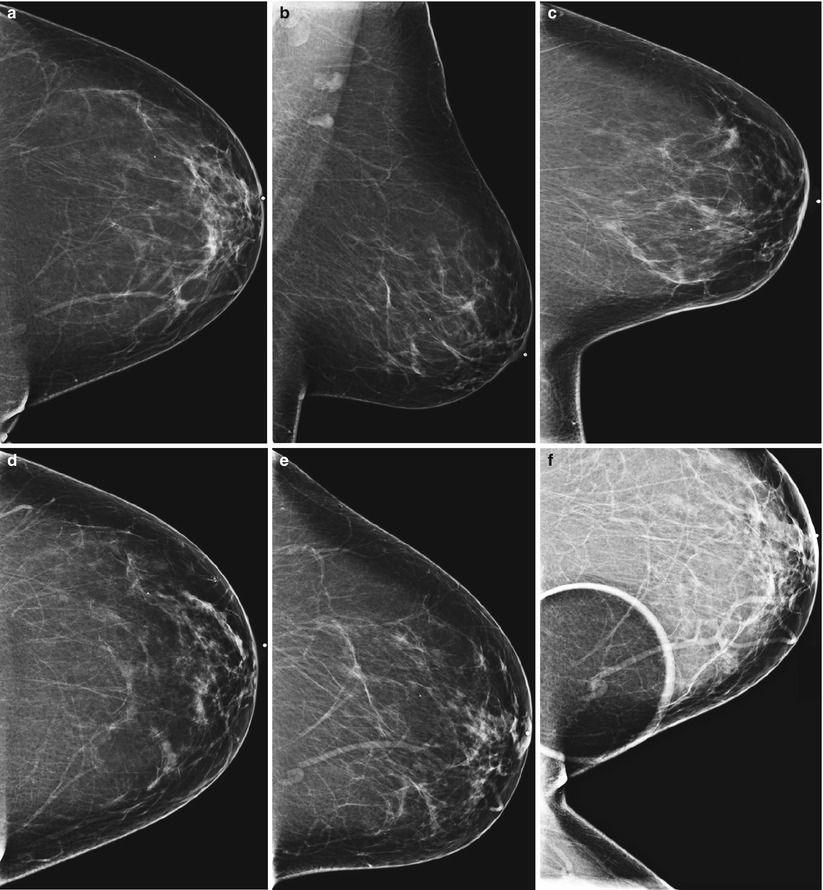
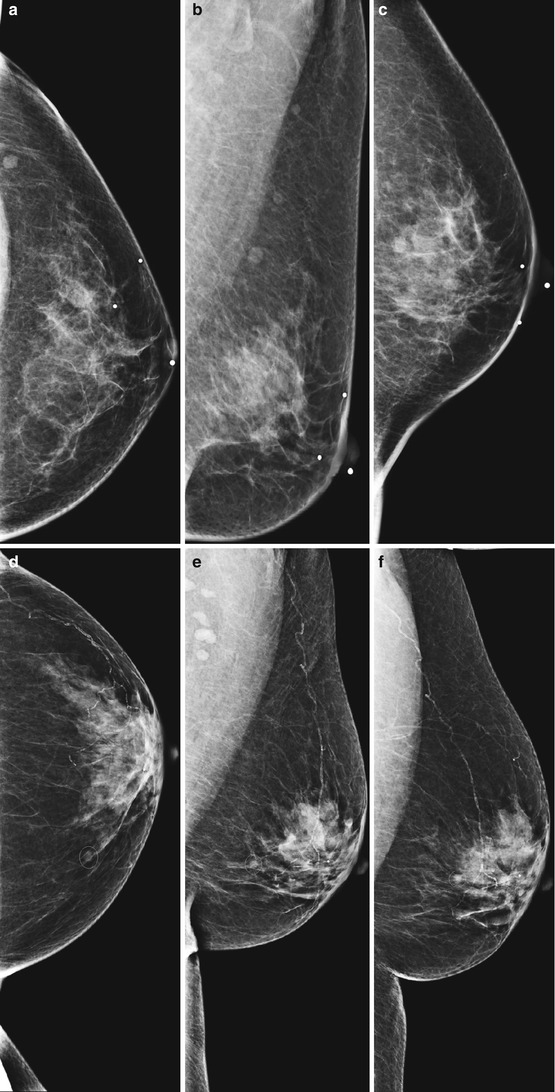
Fig. 3.16
(a–f) Use of rolled views to differentiate between a “pseudomass” from overlapping tissue (a) and a real mass that is not visualized on the MLO (b) or lateral (c) view. In this example, the finding is secondary to a “pseudomass” from overlapping tissue (a). The process of rolling the breast medially (d) and laterally (e) separates the overlapping tissue and the mass disappears. Spot compression view (f) was added to the rolled views to further evaluate the questionable finding
The rolled views can also help localize a lesion if it persists on these views and is still not seen on the MLO view. This concept is discussed in more detail under the section “Localization Techniques” found later in this chapter.
Another technique instead of rolling the breast medially and laterally on the 0° plane is to rotate the imaging receptor 15–20° off the 0° plane (usual CC plane). This technique is more reproducible and is tolerated better by the patient than rolling the breast medially and laterally.
Tangential Views
The tangential views of the breast are utilized to determine if a lesion, usually calcifications, are dermal or intraparenchymal in location. It is important to make this determination prior to scheduling a patient for stereotactic biopsy for suspicious calcifications. These additional views are discussed in more detail under the section “Localization Techniques” found next.
Localization Techniques
For increased diagnostic accuracy, any suspicious lesion should be seen on at least two views so that its true three-dimensional location can be established. One way to determine the location of the lesion of interest is by employing the triangulation technique. The craniocaudal (CC), mediolateral oblique (MLO), and true lateral views (either mediolateral (ML) or lateromedial (LM) views) should be placed with the nipples at the same level and the mediolateral oblique view put in the middle. A straight line drawn passing the lesion of interest on the true lateral view and the mediolateral oblique view will point to the location on the breast in the craniocaudal view. The opposite is also true, as a straight line drawn passing the lesion of interest on the craniocaudal view and the lateral view will point to the location on the breast in the true lateral view. If the lesion “falls” closer to or below the nipple on the ML or LM view as compared to the MLO view, the lesion is located in the lateral aspect of the breast. An easy way to remember is “lead falls,” i.e., if the lesion falls on the ML or LM view, it is lateral in location (Fig. 3.17a–c). Likewise, if the lesion rises closer or is above the nipple on the ML or LM view as compared to the MLO view, the lesion is located in the medial aspect of the breast. The way to easily remember this is the saying “muffins rise,” i.e., if the lesion rises on the ML or LM view, it is medial in location (Fig. 3.17d–f). These steps assist in directing additional imaging to the appropriate quadrant of the breast for spot compression views and/or focused breast ultrasound examination.