Abstract
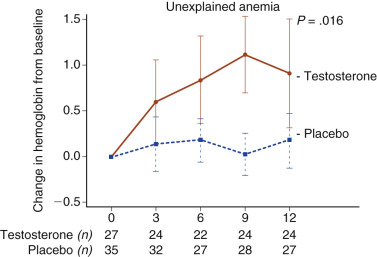
As men age, their reproductive functions, both spermatogenesis and testosterone production, diminish, but slowly and to a relatively small degree. The fall in testosterone appears to be the result of primary hypogonadism in some men and secondary hypogonadism, associated with concomitant illness, in others. The fall in testosterone production may have some consequences, including decreased sexual function, energy, mood, muscle mass, and bone density. Increasing the serum testosterone of older men with low testosterone to that of young men does improve sexual function, mood, walking, anemia, and bone density, but not energy or cognitive function. The cardiac and prostate risks of increasing testosterone in older men are not yet known.
Keywords
Testosterone, spermatogenesis, luteinizing hormone, follicle-stimulating hormone
As men age, reproductive function declines in several ways. Although the change is gradual, unlike the relatively abrupt decline that occurs in women at the time of menopause, it is progressive and probably has some adverse consequences. The decline is sometimes called andropause , male menopause , late-onset hypogonadism , and other terms. This chapter reviews the changes in male reproductive function with aging and what is known about the consequences of attempting to prevent the changes by treatment with testosterone.
Changes in Male Reproductive Function with Age
- ◆
As men age, their reproductive functions, both spermatogenesis and testosterone production, diminish, but slowly and to a relatively small degree.
- ◆
The fall in testosterone appears due to primary hypogonadism in some men and secondary hypogonadism, associated with concomitant illness, in others.
Spermatogenesis and Semen Parameters
The little information available suggests that spermatogenesis does not decline severely with increasing age. Testicular volume, which reflects largely seminiferous tubular volume, averaged 20.6 mL, as determined by ultrasound, in 114 elderly men compared to 29.7 mL in 42 young men. Sperm production was studied in an autopsy study of 89 men aged 21 to 50 years old and 43 men aged 51 to 80 years old who died suddenly. The older men had a daily sperm production rate per testis that was approximately 30% less than that in the younger men. Ejaculated sperm were studied in 20 fathers aged 24 to 37 years old and 22 grandfathers aged 60 to 88 years old. Sperm density was somewhat higher in the older men, and the percentage of sperm motility was somewhat lower in the older men, so the total number of motile sperm was similar in the two groups. In 189 ambulatory men, the serum concentration of inhibin B, a reflection of Sertoli cell function, in men over 70 years old was about 75% of that in men younger than 35 years old ( P = .002). In the same study, the serum follicle-stimulating hormone (FSH) concentration was more than three times as high in the men over 70 years old than in the men under 35 years old ( P < .001). From these data, it appears that sperm production declines with age, but marginally.
Sex Steroid Hormone and Gonadotropin Concentrations
Serum Testosterone Concentration
The serum testosterone concentration has been found to decrease with age in both cross-sectional and longitudinal studies. The decrease appears to occur gradually beginning in the third decade of life. The magnitude of the decrease appears to be greater in longitudinal than cross-sectional studies, and greater in the free testosterone concentration than in the total. This decrease reflects a decrease in testicular secretion of testosterone, since, in men, testosterone is principally of testicular origin.
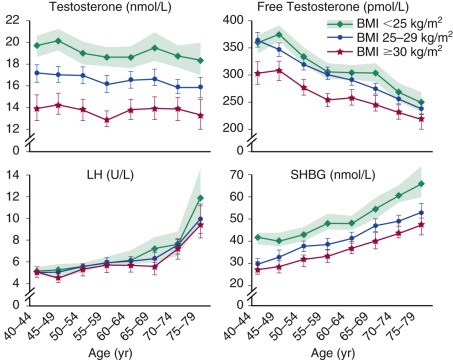
Several cross-sectional studies show a decrease in serum testosterone concentration with age. One cross-sectional study was performed on 302 healthy men in Belgium, in whom the serum testosterone concentrations decreased with increasing age. The mean (± standard deviation [SD]) total testosterone concentration in that study in the 70 men, 20 to 39 years old, was 683 ± 289 ng/dL, and that in 51 men, 70 to 79 years old, was 428 ± 128 ng/dL. The calculated free testosterone concentration fell by a relatively greater amount; in 70- to 79-year-old men it was approximately half of that in 20- to 39-year-old men. In a study of 4263 men, 70 to over 85 years old, total serum testosterone remained stable with age, but sex hormone binding globulin (SHBG) increased and free testosterone decreased. In the European Male Aging Study of 3200 community dwelling men aged 40 to 79 years old, total serum testosterone was not associated with increasing age, but free testosterone was lower and luteinizing hormone (LH) higher ( Fig. 15.1 ), suggesting that primary hypogonadism was the cause of the fall with age. Comorbid conditions and obesity (see Fig. 15.1 ) were also correlated with lower free testosterone concentrations but not higher LH, suggesting that these conditions cause secondary hypogonadism.
Longitudinal studies all show a decrease in testosterone with increasing age. In the Baltimore Longitudinal Study of Aging, the serum total testosterone concentration and a calculated free testosterone index fell from the third to the ninth decades in 890 men who were followed longitudinally. By the eighth decade, approximately 30% of men were hypogonadal using the total testosterone concentration, and 70% were hypogonadal by the free testosterone index. In the Massachusetts Male Aging Study, a population-based, random sample cohort of men aged 40 to 70 at baseline, 1156 men were followed for 7 to 10 years. The serum concentration of total testosterone fell at a rate of 0.8% per year cross-sectionally, but 1.6% per year longitudinally.
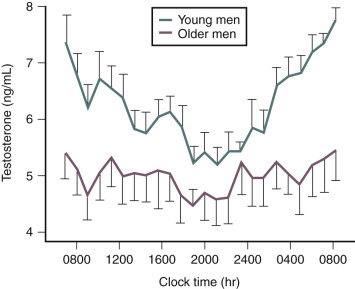
The decrease in serum testosterone concentration with increasing age appears to be primarily the result of a decrease in the morning peak that younger men experience ( Fig. 15.2 ). When the serum testosterone concentration was measured once an hour for 24 hours in 17 men, aged 23 to 28 years old, and in 12 men, aged 58 to 82 years old, the young men exhibited a clear diurnal variation: the peak at 8 am and the nadir at 8 pm . The older men exhibited much less of a diurnal variation, so that the young men had a significantly higher serum testosterone concentration than the older men from 2 am to 1 pm , but not from 2 pm to 1 am . The decrease in serum testosterone concentration with increasing age also appears to be affected by other health factors. In the Massachusetts Male Aging Study, a decrease in body mass index of 4 to 5 kg/m 2 or a loss of a spouse resulted in a similar decrease in testosterone as 10 years of aging.
Serum Estradiol Concentration
The serum total estradiol concentration does not appear to change with increasing age, but the serum bioavailable estradiol concentration, which is not bound to SHBG, appears to decrease slightly. In a study of 810 men aged 24 to 90 years old in Rancho Bernardo, California, the serum concentration of total estradiol decreased by only 0.3 pg/mL per year of age, but the concentration of bioavailable estradiol decreased by 0.12 pg/mL per year of age. In Rochester, Minnesota, 130 men, aged 66 to 90 years old, did not have a significantly different concentration of total estradiol than did 88 men, 22 to 39 years old, but the older men had a significantly lower serum bioavailable estradiol concentration than the younger men, 40 pmol/L compared to 59 pmol/L. In a study of 206 men, 18 to 95 years old in Parma, Italy, both the total and free serum concentrations of free estradiol fell with age.
Serum Gonadotropin Concentration
Both cross-sectional and longitudinal studies show an increase in the serum concentrations of LH and FSH with increasing age. In 15 years of observation in the New Mexico Aging Process Study, the mean serum LH concentration increased from 9.4 mIU/mL to 13.7 mIU/mL and the FSH from 14.1 mIU/mL to 27.4 mIU/mL. In the Massachusetts Male Aging Study, LH increased by 0.9% per year and FSH by 3.1% per year. This increase in serum gonadotropins suggests that a degree of primary hypogonadism is responsible for the decline in testosterone, which is supported by the smaller testosterone response to human chorionic gonadotropin (hCG) or recombinant human LH stimulation of elderly men than young men. However, the increase in basal serum LH is not as great as one would expect for the magnitude of testosterone decline, suggesting secondary hypogonadism as well. In several aspects of LH secretion, the magnitude appears to be less in elderly men than in younger men. The LH response to a bolus dose of gonadotropin-releasing hormone (GnRH) is slightly less in older men than in younger men, and the peak response is somewhat delayed. Spontaneous LH pulses are also different in elderly men compared to young men. LH secretory burst amplitude is less in elderly men than in young men. The fall in testosterone with increasing age, therefore, appears to be the result of a combination of primary and secondary hypogonadism. As shown in the European Male Aging Study, age itself appears to result more in primary hypogonadism and comorbidity and obesity more in secondary hypogonadism.
Consequences of Decreased Serum Testosterone Concentrations
- ◆
The many parallels between the consequences of very low testosterone and the consequences of aging suggest that the fall in testosterone with increasing age may have consequences.
These consequences include decreased sexual function, energy, mood, and physical function, as well as anemia and low bone density.
The parallels between the consequences of frank hypogonadism due to known hypothalamic-pituitary or testicular disease and the consequences of normal aging in men suggest that the fall in testosterone with increasing age might contribute, at least in part, to the consequences of aging in men. These consequences include decreases in bone density and quality, muscle mass and strength, physical function, energy, and sexual function, and an increase in heart disease. Treatment of these deficiencies in frankly hypogonadal men often reverses those consequences.
Bone
The bone mineral density (BMD) of men who are evaluated because of hypogonadism is lower than that of eugonadal men. When men are made hypogonadal by GnRH agonist treatment for prostate cancer, their BMD decreases. In a study of 152 men with prostate cancer—30 who had been kept hypogonadal for less than 6 months, 50 who had been kept hypogonadal for 6 or more months, and 72 who had prostate cancer but were eugonadal, as well as men who did not have prostate cancer—had areal BMD determinations on two occasions 1 year apart. During this year, the men who had been kept hypogonadal for less than 6 months experienced a 4.0% decrease in BMD of the spine and 2.5% of the total hip, but the men who had been hypogonadal for 6 or more months and the eugonadal men did not experience a decrease. Men who are made hypogonadal to treat prostate cancer also are at greater risk for bone fracture, as shown in data from the Surveillance, Epidemiology, and End Results program and the Medicare database, in which the prevalence of fractures was determined in 50,613 men age 66 years or older with prostate cancer who had been made hypogonadal by a GnRH agonist or bilateral orchiectomy. Men who had been made hypogonadal had a significantly higher prevalence of fracture (19.4%) than men not made hypogonadal (12.6%; P < .001). There was also a significant relationship between the number of doses of GnRH agonists and the risk of fracture.
As men age, BMD also decreases. In a study of normal men who had no history of hip fracture, BMD of the spine and hip deceased linearly from age 20 to more than 80 years ( Figs. 15.3 to 15.5 ); the decline was less than that in women, similar to the findings of other cross-sectional studies. However, a cross-sectional study in which bone density was measured by quantitated computed tomography (QCT) showed a greater rate of bone loss, perhaps reflecting the greater sensitivity of QCT in detecting changes in trabecular bone than bone densitometry. A longitudinal study showed as rapid a loss of bone density in men as in women. Within the 2908 men of an average age of 75.4 years in the Swedish Osteoporotic Fractures in Men (MrOS) study, serum free testosterone was a modest predictor of bone density and prevalent osteoporotic fractures. In 728 men at two sites in the European Male Aging Study, increased age was associated with decreased cortical BMD by peripheral QCT. The association of the decrease in cortical bone with the serum concentrations of estradiol and testosterone was less clear.

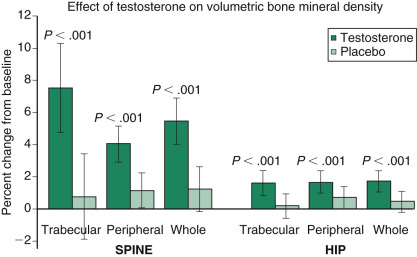
Replacement of testosterone in unequivocally hypogonadal men greatly increases BMD. Administration of 100 mg of testosterone enanthate once a week for 18 months to 29 men with previously untreated hypogonadism resulted in a 5% increase in BMD in the lumbar spine as determined by dual energy x-ray absorptiometry (DEXA). Trabecular BMD, as measured by QCT, increased by 14%. Administration of testosterone transdermally for 3 years to 18 hypogonadal men who had previously untreated hypogonadism resulted in increases in BMD as determined by DEXA of 7.7% at the lumbar spine and 4.0% at the trochanter.
Body Composition
When men become hypogonadal as the result of hypothalamic-pituitary or testicular disease, they experience a decrease in lean body mass and an increase in fat mass, and testosterone treatment of hypogonadal men usually reverses those changes. The same changes occur as men age. Whole-body lean mass in one study was about 15% less at age 70 than at age 20, and whole body fat mass was about 100% more. In another study, appendicular skeletal muscle mass was 16% less in men over 75 years old than in men 18 to 34 years old. The percentage of body fat was 26% in 36 hypogonadal men compared to 19% in 44 eugonadal men. When six normal young men were made hypogonadal for 10 weeks by the administration of the GnRH agonist leuprolide, their fat-free mass decreased from 56.5 to 54.4 kg and their fat mass increased from 15.8 to 16.9 kg.
Administration of testosterone reverses these changes in body composition. Administration of 100 mg of testosterone enanthate once a week for 18 months to previously untreated hypogonadal men resulted in a 14% decrease in total body fat and a 12% decrease in subcutaneous fat, as assessed by QCT. Lean muscle mass, assessed by the same technique, increased 6.8%. When testosterone was administered transdermally to 18 previously untreated hypogonadal men, lean body mass increased.
Muscle Strength
Muscle strength has long been known to decrease with increasing age, but demonstrating that hypogonadism leads to decreased muscle strength, and that testosterone treatment improves strength, has been much more difficult. In a study of 72 normal men in three age groups aged 20 to 86, the strength of knee extension, both isometric and isokinetic, decreased with increasing age. In another study in 114 men aged 11 to 70 years old, quadriceps strength increased up to the third decade, was stable until age 50, then declined with increasing age. The only clear demonstration that hypogonadal men have lower muscle strength than eugonadal men was provided by the study described earlier in this chapter, in which six healthy young men were made severely hypogonadal for 10 weeks by the administration of leuprolide. At the end of the 10 weeks, their strength of knee extension was 6% less than prior to treatment when measured isokinetically at 60 degrees angular velocity, but was not significantly different during treatment than before when measured isokinetically at 180 degrees angular velocity or isometrically at either angular velocity.
Administration of testosterone transdermally to 18 previously untreated hypogonadal men did not increase their strength of knee extension or flexion or handgrip strength. Administration of 100 mg testosterone enanthate once a week to men with wasting secondary to human immunodeficiency virus (HIV) infection resulted in a 16% increase in leg press strength compared to no significant change in those treated with placebo, whereas men who were treated with testosterone and resistance exercise did not exhibit a greater increase than those treated with placebo and exercise. In short, it is clear that muscle strength decreases with increasing age, but it is not clear how much, if any, the decline in testosterone contributes to the decrease in muscle strength.
Physical Function
The relationship between testosterone and physical function in middle-aged to elderly men was evaluated in the Framingham Offspring Study, in which 1445 men, with an average age of 61 years, were evaluated twice, an average of 6.6 years apart. By logistical regression analysis, free testosterone, but not total, was associated with incident Short Performance Physical Battery score and usual walking speed but not with grip strength. Free testosterone at the first visit was significantly associated with increased risk of self-reported mobility disability at the second visit.
Cardiovascular and Metabolic Risk
Because the prevalence of heart disease is greater in men than in women, the possible role of testosterone in the development of arteriosclerotic cardiovascular disease has long been discussed. An alternative explanation for the difference is higher estradiol concentrations in women before menopause. This possibility is suggested by the gradual decrease in the gap between the genders the greater the length of time after menopause. One study, however, suggests that it may be low testosterone that is harmful. When 794 men of median age 73.6 years had a serum testosterone measurement and were followed for an average of 11.8 years, the men whose serum testosterone concentrations were in the lowest quartile (<241 ng/dL) were 40% more likely to die of all causes, and 38% were more likely to die of cardiovascular causes than the men with higher values. This association was independent of age, adiposity, and lifestyle.
If low testosterone does cause an increased mortality rate, one possible mechanism is via metabolic risk factors, because, in epidemiological studies, low testosterone precedes the development of central obesity, metabolic syndrome, and diabetes. However, in the study cited earlier in this chapter, the association between low testosterone and higher mortality rate persisted even after adjusting for metabolic syndrome and diabetes mellitus. Further, associations between testosterone, metabolic syndrome, and diabetes are equivocal. In the Baltimore Longitudinal Study of Aging, the prevalence of the metabolic syndrome was associated with a lower total testosterone, but a higher index of free testosterone. Conversely, in an analysis of data from the Third National Health and Nutrition Examination Survey (NHANES III), men in the lowest tertile of an index of free testosterone were four times as likely to have a diagnosis of diabetes mellitus than men in the highest tertile, but that relationship was not observed with total testosterone. Perhaps the best evidence that testosterone influences glucose metabolism is a randomized, placebo-controlled, crossover trial in which testosterone treatment of men for 3 months who had type II diabetes and low-normal to low serum testosterone concentrations improved their fasting glucose, hemoglobin A 1 c, and homeostatic model assessment (HOMA) index, compared to placebo treatment.
Other possible mechanisms by which testosterone could affect cardiovascular disease are via serum lipids, clotting factors, and markers of inflammation, but the treatment of hypogonadal men with testosterone does not consistently change these parameters.
Energy
Men’s sense of energy decreases with increasing age, and when men who are hypogonadal due to known disease are treated with testosterone, their self-reported energy increases markedly. Administration of testosterone transdermally to 18 men with severe, untreated hypogonadism resulted in an increase in self-reported energy, reaching an apparent peak in about 3 months.
Cognition
The association of low testosterone with declining cognitive function was evaluated in the Baltimore Longitudinal Study of Aging, in which 407 men aged 50 to 91 years old at baseline assessment were followed for an average of 10 years. Men who were classified as hypogonadal, defined for this study as a free testosterone index (total testosterone/SHBG) below the 2.5 percentile, had significantly lower scores on measures of memory and visuospatial performance, and a faster decline in verbal memory.
Sexual Function
Low testosterone appears to be associated with decreased sexual function in middle aged and elderly men, as shown in data from the European Male Aging Study. In a random population sample of 3369 men aged 40 to 79 years, the combination of three sexual symptoms (low sexual desire, poor morning erection, and erectile dysfunction) was significantly related to total and free testosterone concentrations; the relationship was stronger the lower the testosterone. Hypogonadism also causes a decrease in libido. When men who were unequivocally hypogonadal were treated with a single dose of testosterone enanthate, sexual function increased much more within a few weeks after a dose of 100 mg than a dose of placebo, and even more after a dose of 400 mg than 100 mg. When 18 severely hypogonadal men were treated with testosterone transdermally, sexual function increased markedly when first reassessed at 3 months, but did not increase further when the observation was continued for a total of 3 years.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree