Major Concepts
Historical Incidence
Malaria has plagued humankind since antiquity. In the third century B.C., the conquests of Alexander the Great were cut short by this disease. Italy was long affected by the illness. A swampy area near ancient Rome, the Pontina, was noted for its high rate of infection. In the 1930s, the Italian dictator Benito Mussolini drained the swamps and greatly decreased disease incidence. Malaria was once common in parts of the United States, particularly the southern states but also in areas such as northern Ohio. In the early 1900s, construction of the Panama Canal required decreasing the incidence of mosquito-borne malaria and yellow fever by reducing vector numbers. Toward the end of that century, after several major battles in the war against malaria had been won, the tide began to turn and malaria began to reemerge in some areas of the world due to resistance and increased travel and migration to endemic areas.
Current Impact
At present, 350 to 500 million people are infected with the malaria parasites, and more than 1 million of them die each year, making malaria one of the major causes of death from infectious diseases today. Sub-Saharan Africa has been and remains one of the hardest-hit areas, with about 90% of the world’s cases, the majority occurring in young children. In addition to the high death toll in the very young, infection of either expectant mother or fetus leads to premature birth, low birth weight, anemia, epilepsy, and learning difficulties in children. Countries in this region suffer huge economic losses resulting from ill workers, decreased tourism, and the unwillingness of companies to invest in high-risk areas.
Symptoms
Malaria is best known for its cyclical periods of severe high fever and chills, but nonspecific symptoms occur as well, including headache, fatigue, abdominal discomfort and vomiting, muscle and joint aches, loss of appetite, and malaise. The cycles last either 48 or 72 hours, depending on the species of parasite. These result from periodic rupture of infected erythrocytes, the release of large amounts of hemoglobin, and its conversion into the toxic compound bilirubin. Exposure to bilirubin may result in renal or heart failure. One of the more serious consequences of infection is cerebral malaria, characterized by progressive headache, very high fever, psychosis, convulsions, coma, and rapid death. Another very serious condition is blackwater fever, in which the kidneys are damaged by massive amounts of hemoglobin, producing black urine and death from renal failure. The mortality rate for cerebral malaria and blackwater fever is 20% to 50%. Other serious complications of malaria include severe anemia, metabolic acidosis, hypoglycemia, and acute pulmonary edema. Young children are most vulnerable to developing severe disease due to their lack of protective antibodies.
Infection
Four members of the Plasmodium genus of Apicomplexan protozoa cause human malaria. The most pathogenic of these is P. falciparum, which kills more erythrocytes than the other species because it infects red blood cells of any age. This species also has the highest rate of drug resistance. P. vivax is found more commonly in temperate zones and causes a milder form of the disease. It infects only immature erythrocytes. P. malariae infects older cells and has a longer cycle than the other species. P. ovale is the rarest of the malarial parasites. Plasmodium species have a complex life cycle involving two different hosts, the Anopheles mosquito and a human host. Sporozoites are injected into humans as female mosquitoes take a blood meal. They travel to the liver and infect hepatocytes, transforming into merozoites, which multiply asexually and subsequently burst the host cell to travel into the bloodstream and infect erythrocytes. Once inside these blood cells, asexual reproduction leads to the production of more merozoites. These rupture the infected cells and enter new erythrocytes to continue the cycle in humans. Other merozoites transform into male and female gametocytes that are ingested by a mosquito feeding on the infected person. Once inside the mosquito, the gametocytes produce micro- and macrogametes, similar to sperm and eggs. A microgamete fertilizes the macrogamete and produces a motile zygote, the ookinete, which penetrates the mosquito’s stomach and transforms into an oocyst on the exterior of that organ. Asexual reproduction results in the formation of multiple sporozoites that travel to the mosquito’s salivary glands in preparation for being transferred to the next human host.
Protection
Treatment for malaria has historically included drugs such as artemisinin from wormwood, quinine, and chloroquine. Drug resistance reduced the effectiveness of these and other more recently developed drugs, leading to a resurgence in disease incidence. The insecticide DDT was once very effective in reducing numbers of the mosquito vectors, but many regions either banned or severely restricted its use, and mosquitoes subsequently became resistant to this inexpensive and nontoxic insecticide. Several effective campaigns are currently under way to decrease malarial incidence, particularly in sub-Saharan Africa. These rely heavily on the use of DDT-treated bed nets and indoor residual insecticide use.
In human beings, malaria is caused by four species of parasitic blood protozoa of the genus Plasmodium. Malaria is a huge health problem worldwide, with 350 to 500 million people infected and 1 to 2 million dying each year. Approximately 41% of the world’s population is at risk for contracting disease, with 90% of the cases occurring in sub-Saharan Africa. Most of these are in children less than 5 years of age and are responsible for 20% of the childhood deaths in Africa. In addition to death, malarial infection induces premature birth, low birth weight, anemia, epilepsy, and learning difficulties in children. This decreases educational opportunities for children and may lead to permanent neurological damage. Malaria is estimated to cost Africa $12 billion per year in lost income as a result of illness in workers, decreased tourism, and an unwillingness of many companies to invest in high-risk areas. Together, these factors magnify malaria’s toll on countries with high rates of infection.
Chemicals have been developed to kill either the malarial vector or the parasites themselves, leading many people to believe that malaria might be brought under control. However, the development of resistance has been problematic. Furthermore, some of the most effective agents have been cited as harmful environmental contaminants. New drugs and new strategies are raising cautious optimism in the health care community.
At one time, malarial infection was problematic throughout the world. In addition to areas currently affected, such as parts of Africa and Asia, southern Italy was particularly hard-hit. Many swamps were found in close proximity to ancient Rome, the Pontina, which had very high infection rates. “Bad air” (mal aria) from swamps was thought to be responsible. The Italian dictator Benito Mussolini drained these swamps and greatly decreased disease incidence in Italy during the 1930s. Malaria was also common in parts of the United States, particularly in the southern states but also was found as far north as Cleveland and Toledo, in northern Ohio, until the 1830s.
FIGURE 24.1 Construction of a drainage ditch to eliminate vector breeding sites, Virginia, 1920s
Source: CDC.
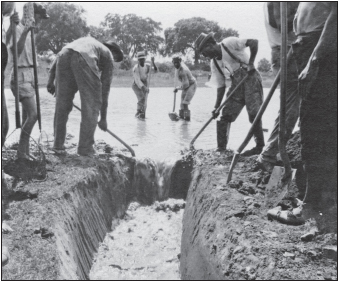
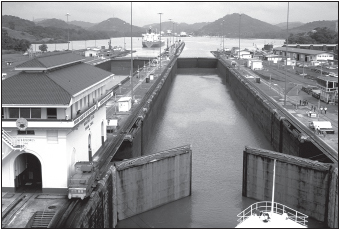
Controlling malaria and yellow fever by decreasing the numbers of their mosquito vectors was vital to the construction of the Panama Canal in the first decade of the 1900s. This was accomplished under the direction of W. C. Gorgas of the U.S. Army Medical Corps through a combination of drainage, cutting of brush and grasses, adding oil to standing water that served as habitat for larvae, and the use of quinine. Thanks to these efforts, death rates of canal workers decreased from 11.6 per 1,000 in 1906 to 1.2 per 1,000 in 1909, permitting completion of the canal that decreased the need for ships to make the dangerous passage around Cape Horn at the tip of South America, facilitating travel and trade between the Atlantic and Pacific Oceans
The decrease in numbers of mosquitoes of the Anopheles genus in affected areas was vital to freeing them from the burden of malaria, as was the development of effective drugs that killed the protozoa responsible for causing the disease. As mosquitoes and parasites developed resistance, however, the incidence of malaria rose greatly. In some areas of Africa, the infection rate of the population was 150% annually (virtually all members of the population became infected, many of them more than once a year). In the United States between 1957 and 2003, a total of 63 outbreaks were attributed to bites of locally occurring mosquitoes. Two mosquito species capable of malaria transmission remain common in the United States, allowing the possibility of reintroduction. Currently, however, most cases in North Americans do not occur in the traditional manner. Between 1963 and 1999, some 93 cases resulted from blood transfusion. In 2002, a total of 1,337 cases were reported, all but 5 of them imported from regions in which the disease is endemic.
FIGURE 24.2 One of the fruits of malaria reduction programs in the Western Hemisphere: the Panama Canal
Source: CDC/Edwin P. Ewing Jr.
Malaria is best known for the development of alternating periods of fever and chills, but its initial symptoms are nonspecific and similar to mild viral infections. These symptoms include headache, fatigue, abdominal discomfort and vomiting, muscle and joint aches, loss of appetite, and malaise. A high body temperature is present during both fever and chill stages as the erythrocytes periodically rupture and release intracellular contents, such as hemoglobin and its toxic byproduct, bilirubin. Cycles occur every two to three days, depending on the parasite species. Individuals with most types of malaria often feel better between cycles. The fever and chills may be very intense and debilitating; the affected individual might shake hard enough to damage the bed. Anemia, sometimes severe, results from erythrocyte rupture. The person may experience severe nausea and continuous vomiting. Renal or heart failure may result from bilirubin exposure.
Several far more serious disease manifestations may occur. One such manifestation is cerebral malaria, resulting from parasite entry into the central nervous system. Cerebral malaria is characterized by a progressive headache, very high fever which may exceed 108°F (42°C), psychosis, convulsions, coma, and death within hours. This form of the disease has a mortality rate of 25% to 50% and is usually restricted to infection caused by Plasmodium falciparum. Another very serious condition associated primarily with P. falciparum is blackwater fever. During this manifestation, the kidneys are damaged by massive releases of hemoglobin from ruptured erythrocytes. The presence of this pigment produces black urine. Death usually results from renal failure. This condition is believed to have an autoimmune component, as antibodies aid in the erythrocyte lysis. Mortality rate is 20% to 50%. Other serious complications of malaria include metabolic acidosis, hypoglycemia, and acute pulmonary edema.
Malaria may be especially harmful to the very young. Infection raises the risk of low birth weight, childhood mortality, and neurological damage and is particularly problematic in areas where access to proper nutrition and health care is limited. Pregnant women are more susceptible to infection with the highly pathogenic P. falciparum.
After a person’s initial infection, a state of partial immunity often occurs, reducing the individual’s parasite burden and subsequent disease severity during future infections. In areas of the world with high and stable rates of infection, therefore, severe malaria is often restricted to the very young, travelers, or the immunocompromised, including HIV-positive individuals. In some areas, such as sub-Saharan Africa, incidence of both HIV and malaria is very high. In parts of the world with lower or fluctuating rates of infection, severe disease occurs in any age group and may result in epidemics. Travelers or immigrants from malaria-free areas entering endemic areas, including military personnel, are at higher risk of more severe disease due to their complete lack of protective immunity. Currently, no effective vaccine exists for malaria prevention despite enormous amounts of research having been conducted for decades.
In humans, four species of parasitic blood protozoa of the genus Plasmodium cause malaria. These parasites are members of the Apicomplexan class Sporozoa. Other species of the genus cause disease in animals.
Life Cycle
The life cycle of the Plasmodium species responsible for malaria is split between the human host and the vectors, Anopheles mosquitoes.
The portion of the cycle occurring in humans begins when sporozoites are injected into the human host from the salivary glands of an infected female mosquito during a blood meal. The sporozoites travel via the blood to the liver and there infect hepatocytes within 30 minutes. They then divide repeatedly asexually, forming schizonts containing 30,000 to 40,000 individual merozoites. The schizont ruptures, releasing merozoites that infect erythrocytes. In these cells, the merozoites first develop into the ring form, which resembles a signet ring, and then divide rapidly, each parasite producing 8 to 24 daughter cells. The cells lyse with a periodicity related to the parasite species, releasing the newly formed merozoites. For most malaria-inducing parasite species, cell rupture is synchronized, occurring in waves. Some merozoites infect new erythrocytes, continuing the blood cycle, while others develop into sexual stages of male and female gametocytes. Some of these are ingested by another feeding mosquito to start the next stage of the life cycle.
Once inside the female mosquito, gametocytes develop into the female macrogamete, similar to an egg, or multiple male microgametes, similar to sperm. The microgamete penetrates a macrogamete, and fertilization occurs inside the mosquito’s stomach, producing an ookinete. This motile form of the parasite passes through the wall of the stomach to form an oocyst on its outer wall. The oocyst divides asexually to produce multiple sporozoites, which migrate to the mosquito’s salivary glands and from there are passed to another human to continue the cycle in a new host.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








