Major Concepts
The Populations
Persons with compromised immune systems fall into various groups. Some of the causes of immunosuppression are transient, and the immune systems of these people return to a normal functional state with time. Such populations include infants, pregnant women, individuals receiving chemotherapy, and persons with a short-lived viral infection. Others are immunosuppressed for lengthy or indefinite periods of time, including those with metabolic disorders, with congenital immune deficiencies, on long-term immunosuppressive drug treatments, or with certain chronic viral infections. The number of immunocompromised persons is currently increasing, especially in developed areas of the world where those in a weakened state of health are surviving for longer periods of time.
Causes of Immunosuppression
A number of factors may induce a state of reduced immunity. Some of these factors relate to a person’s age (fetuses, infants, and the elderly), special circumstance (pregnancy), genetic background (inherited immune deficiency disorders), or lack of immune system organs. Other immunosuppressive elements are acquired during one’s lifetime, such as immunosuppressive bacterial or viral infections, including AIDS. Medical interventions may compromise a person’s immune response. Immunosuppressive drugs may be administered during the treatment of several diseases, including cancer and inflammatory conditions. Chemotherapy drugs and dialysis also decrease immune responsiveness. Compounds naturally produced by the human body (some hormones and cytokines) may also inhibit activity of various parts of the immune system.
Diseases
Immunosuppressed persons are particularly vulnerable to diseases caused by some bacteria, viruses, fungi, protozoa, and helminths. Some of the most troublesome of these microbes are Clostridium difficile, agents that cause respiratory and diarrheal diseases, cytomegalovirus, rotavirus, Toxoplasma gondii, and Cryptosporidium. The pathogenic role of many fungi in immunosuppressed populations is becoming increasingly well known. Coinfection with HIV and other organisms, including Mycobacterium tuberculosis, Trypanosoma cruzi, and Leishmania species, is especially problematic.
This book describes a number of infectious diseases that are presently emerging as novel threats to human health as well as infections that for a variety of reasons are reemerging to endanger new segments of humanity or have escaped the mechanisms that humans have carefully created over decades for our protection (antibiotics, vaccines). One of the large categories of emerging infectious diseases encompasses diseases that strike persons whose immune system is compromised, leaving them vulnerable to infection with one or more groups of microbes. Many of the diseases described in other chapters are either only pathogenic in immunosuppressed individuals or cause much more serious or life-threatening diseases in these people. Given the large increase in numbers of persons with dysfunctional immune responses, many people currently entering the health care or public health fields will find themselves addressing some unique forms of microbial infection as well as special needs of persons harboring the responsible microbes. This chapter describes specific populations of persons at high risk of developing these infections and the microbes involved in disease causation.
Several groups of people have compromised immune systems that leave them more susceptible to malignancies and infections than the general population. Immunocompromised persons are at greater risk for developing opportunistic infections by microbes that typically are a part of the normal flora or even some that under other circumstances act in a manner that benefits both host and microbe. In other cases, infections that usually result in mild or self-limiting infections in immunocompetent persons may engender chronic or severe and life-threatening infections in immunosuppressed individuals. The number of such persons is increasing in developed nations as the population ages, as organ transplantation becomes more common, as more individuals become obese and thus more prone to developing type 2 diabetes or requiring dialysis, and as persons with previously fatal medical conditions live for an extended number of years.
Immunocompromised individuals may be divided into several groups. The first group includes specific segments of the population, such as infants, the elderly, and pregnant women. The second group consists of persons whose immune system is affected by medical procedures. This group would include recipients of cancer chemotherapy, diabetics and hemodialysis patients, transplant recipients, and persons receiving anti-inflammatory therapy for the treatment of autoimmune, inflammatory, or allergic disorders. The third group encompasses individuals with other disease conditions or disorders. Persons in this category include those with congenital immune deficiency diseases; those with immunosuppressive bacterial or viral infections, including HIV-positive persons; those who are malnourished, debilitated, or depressed; diabetics; individuals without a spleen; those in burn units; and those with congenital diseases such as β-thalassemia, Down syndrome, or cystic fibrosis.
Selected Causes of Immunosuppression
A variety of factors may compromise an individual’s defense systems. The immune system is not fully developed until well after birth and later in life loses functionality during the aging process. Several types of congenital immune system diseases affect various components of the immune system, whereas other immunosuppressive conditions are acquired.
Age- or Pregnancy-Related Defects in Immune System Functioning
Immune Alteration During Pregnancy
A state of induced immunosuppression occurs during pregnancy to prevent rejection of the fetus, whose cells contain foreign MHC class I molecules from the father. Several changes occur in antibody production and T lymphocyte numbers and activity. While some of these alterations decrease autoimmune conditions, they nevertheless make the mother more susceptible to microbial infections, as demonstrated by the relatively high number of pregnant women becoming severely ill or dying during the 2009–2010 H1N1 flu season.
Estrogen levels increase during pregnancy. Estrogens, female sex hormones, trigger an increase in antibody production, and some of these antibodies are transported across the placenta to protect the fetus. The incidence of some autoimmune disorders, such as systemic lupus erythematosus and diabetes, increase during pregnancy and decrease immediately postpartum as estrogen levels fall.
The activity of Th1 cells is reduced during pregnancy and restored postpartum, partly due to alterations in estrogen levels as this hormone decreases Th1 immune responses. The decrease in Th1 activity during the third trimester reduces the relapse rate in individuals with multiple sclerosis; the rate increases again by three months after birth. Treg cells play a vital role in decreasing Th1 and NK activity during pregnancy to prevent immunological rejection of the fetus. Treg numbers rise early during pregnancy in response to increased estrogen levels. Treg cells have on their surface the immune-inhibitory molecule cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4), which up-regulates the expression of another immunosuppressive molecule, indoleamine 2,3-dioxygenase (IDO), on cells that normally aid in T helper cell stimulation, including monocytes and macrophages; instead of stimulating T helper cells, IDO-expressing monocytes and macrophages instead block T cell activation.
Immune Defects in the Very Young
Newborns, infants, and young children have low levels of immunity until their immune system develops, leaving them more susceptible to infections. Both antibody and T cell activities are affected. Young children have high numbers of naive T cells, but these do not generally respond well to microbes.
Fetal antibody production begins approximately 20 weeks after birth, and adult antibody levels are not attained for five years. During fetal development, maternal antibodies protect against infection. IgG antibodies from the mother are able to pass through the placenta to the fetus during the last ten weeks of pregnancy. After birth, IgA antibodies are obtained by infant through the mother’s milk and play an important role in preventing lung and gastrointestinal infections. Infants who are bottle-fed are 60 times more likely to develop pneumonia during the first three months of life than those receiving maternal IgA through breast-feeding. Some children develop transient hypogammaglobinemia (low antibody levels), especially IgG2, during their first year of life due to a delay in maturation of antibody synthesis.
Premature infants are particularly prone to infections because they receive less of the IgG normally transported to the fetus during late gestation. They also have reduced complement activity: complement produces large pores in bacteria, which lyse the microbes. Premature infants also have more respiratory infections because the production of lung surfactant begins late during gestation. Surfactant contains collectins, defense proteins that bind sugars on microbial surfaces and aid in the killing of these invaders by phagocytes or the complement system.
Decreased Immunity in the Elderly
During the aging process, many components of the immune system diminish in number, reaching very low levels in the elderly and leaving this population much more susceptible to infection. Because both innate and adaptive immune responses are affected, the elderly are prone to infection by many different types of microbes.
Production of neutrophils, monocytes, and macrophages is decreased in the elderly due to low levels of a key hematopoietic growth factor that stimulates the synthesis of the appropriate progenitor cells in the bone marrow. Macrophages’ ability to kill microbes is diminished as well because their production of antimicrobial hydrogen peroxide and nitric oxide is reduced. Macrophages are activated by IFN-γ, and T cell production of that cytokine is also reduced.
Increases in prostaglandin synthesis may contribute to the decrease in T cell functions. Numbers of mature T lymphocytes are decreased during aging due to the loss of thymic tissue. The thymus is an immune system organ that is primarily responsible for the selection and maturation of T cells. Decreased activity of this organ during aging reduces the body’s ability to replace T lymphocytes. During aging, T cells themselves are less able to divide in response to microbes and produce lower amounts of cytokines such as IL-2, IFN-γ, and IL-4. Loss of IL-2 impairs T and B lymphocyte division and activation. Decreased levels of IFN-γ reduce protection against viruses and impair macrophage activity. Reduced production of IL-4 impairs synthesis of some Th2 cytokines.
Genetic Defects in the Immune System
A number of inherited conditions reduce antimicrobial activity of the immune system by either decreasing numbers of leukocytes or leading to loss of functioning. These genetic immunodeficiency disorders (primary immunodeficiencies) may be divided into three categories: those that affect neutrophils and monocytes, lymphocytes, or the complement system. The first category of immunodeficiency diseases includes congenital neutropenia (decreased neutrophil numbers resulting from reduced levels of a growth factor, G-CSF, which normally triggers bone marrow stem cells to produce these cells) and leukocyte adhesion deficiency (defective expression of cell surface molecules that normally allow neutrophils and monocytes to adhere to and pass through the endothelial cells of the blood vessels, inhibiting passage of these cells to sites of infection). The second category of primary immunodeficiency diseases includes common variable immunodeficiency (reduced numbers of antibody-producing cells) and several types of severe combined immunodeficiency syndrome (lack of mature T and B lymphocytes). The third category of primary immunodeficiency disorders leads to defective killing of microbes by the complement system due to decreased levels of several components of the complement cascade or its regulatory molecules.
Immunosuppression Resulting from Bacterial or Viral Infections
Infection with several bacteria and viruses may lead to a generalized state of immunosuppression that worsens the effects of diseases caused by other pathogens or permits the development of severe disease by typically benign opportunistic microbes. Anaplasma phagocytophilum (discussed in Chapter Four) is one such bacterium that infects neutrophils and impairs their activity, increasing the host’s susceptibility to opportunistic diseases caused by fungi or viruses. Several viruses may also impair the immune response. HIV (discussed in Chapter Sixteen) affects functions of many immune cells, including T helper cells, which it infects and kills. Infection with either the measles or Epstein-Barr virus induces a generalized state of immunosuppression as well.
Drugs That Suppress Immune Responses
Immunosuppressive antirejection drugs must be administered to recipients of solid organ or bone marrow transplants to prevent immune-induced graft rejection. Anti-inflammatory drugs, used in the treatment of conditions such as rheumatoid arthritis, psoriasis, and Crohn’s disease, also suppress T cell activity in order to block excessive pathogenic immune activation. Antirejection and anti-inflammatory drugs include corticosteroids such as prednisolone, tacrolimus, mycophenolate mofetil, cyclosporine A, and azathioprine. Monoclonal antibodies directed against immune cells (anti-CD3 and anti-CD4 antibodies to eliminate T lymphocytes) or against cytokines (anti-TNF-α antibody) also decrease graft rejection. These drugs all greatly increase the risk of microbial infections.
Cancer patients, especially those with hematological malignancies such as leukemia or lymphoma, are debilitated and hence more susceptible to microbial infection. Chemotherapeutic medications increase cancer patient vulnerability. This is particularly true of drugs used to treat leukemia and lymphoma because the cancer cells being targeted are immune cells, and many nonmalignant white blood cells and bone marrow stem cells are killed as well.
Other drugs may also affect susceptibility to microbial infection. Alcohol and illicit drugs decrease nutritional status, leading to debilitation and decreased immune responsiveness.
Immunosuppressive Hormones and Cytokines
Corticosteroids, such as cortisol, are hormones produced by the adrenal cortex. These stress hormones inhibit T cell activity, and persons living with chronic stress are at higher risk for developing infections than nonstressed persons who produce less of these hormones.
Treg cells, a subset of CD4+ T lymphocytes, down-regulate Th1 and Th2 immune responses. These cells act via the production of the regulatory cytokines IL-10 and TGF-β.
Table 29.1 Some factors that inhibit immune system functioning
| Age-related conditions | Fetuses, infants, the elderly |
| Health conditions | Pregnancy, diabetes, dialysis, depression, Down syndrome, cystic fibrosis, β-thalassemia, surgery, malnutrition, debilitating conditions |
| Primary immunodeficiencies | Deficiencies in monocytes and neutrophils, lymphocytes, complement system |
| Immunosuppressive infectious agents | Some bacteria, some viruses |
| Drug therapy | Antirejection drugs, anti-inflammatory drugs, chemotherapeutic drugs |
| Lack of immune system organs | Lack of thymus, loss of spleen |
Lack of Immune System Organs
The absence of immune system organs impairs defense against several types of microbes. In DiGeorge syndrome, children are born with a developmental defect that leads to the absence of a thymus, among other effects. Such children lack mature T lymphocytes. The spleen is an immune organ that may be severely damaged by trauma and removed surgically, often following a motorcycle accident. The spleen houses many B lymphocytes and macrophages.
Infectious Diseases of the Immunosuppressed
In a 2008 report, 199 pediatric kidney transplant recipients were followed for three years. A total of 64 episodes of diarrhea occurred during this period, 38 of them resulting from microbial infections: viruses in 16 patients, bacteria in 10, yeast in 4 (Candida albicans), and parasites in 8 (Giardia lamblia in one patient and Cryptosporidium in the others). The viral infections were as follows: cytomegalovirus (CMV; nine cases), rotavirus (five), and adenovirus (two). Of the bacterial infections, Clostridium difficile was found in four persons, especially within the first 30 days of transplant; Helicobacter pylori in three; and Escherichia coli, Campylobacter jejuni, and Salmonella enteritidis in one person each. In a 2007 study of kidney and liver transplant recipients, 33 episodes of diarrhea occurred due to infection by viruses—CMV (six cases) and rotavirus (one); bacteria—C. difficile (three), C. jejuni (two), Shigella sonnei (two), and S. enteritidis (one); parasites—G. lamblia (nine), Cryptosporidium (seven), Entamoeba histolytica (one); and a fungus—Blastocystis hominis (one). C. difficile again predominated early after transplant, while CMV was the most common microbial agent between months 1 and 6.
Bacterial Infections
Respiratory Tract Infections
Immunocompromised persons are particularly vulnerable to severe respiratory tract infections as a result of infection by different groups of bacteria. Several of these bacteria are discussed elsewhere in this book (Legionella pneumophila in Chapter Nine, Pneumocystis jiroveci (carinii) in Chapter Sixteen, and Mycobacterium tuberculosis in Chapter Ten). Other species of the Mycobacterium group also cause disease in immunocompromised persons, including HIV-positive persons, children, alcoholics, and those with chronic lung disease. Infections with members of the M. avium complex, M. kansasii, M. malmoense, and M. xenopi are particularly likely to result in respiratory tract disease. Pseudomonas aeruginosa infection is common among persons with cystic fibrosis and may result in serious illness, while infection with Burkholderia cepacia is particularly dangerous.
Nocardia species are gram-positive, branched filamentous bacteria. Infection with members of this group is common among transplant recipients but not immunosuppressed cancer patients.
Mycoplasma pneumoniae is a member of an unusual group of very small bacteria that lack a cell wall. They are the primary agents responsible for “walking pneumonia” and may also induce tracheobronchitis and bronchiolitis along with upper respiratory tract symptoms. Infection may also exacerbate asthma. Other nonpulmonary manifestations of infection include arthritis, gastrointestinal disorders (nausea, vomiting, and diarrhea), muscle ache, kidney damage, and skin rash. Some persons with primary immunodeficiency disease are more likely to develop joint and respiratory disease, brain abscesses, and subcutaneous skin nodules or abscesses. Renal manifestations are found in persons with AIDS.
Digestive Tract Infections
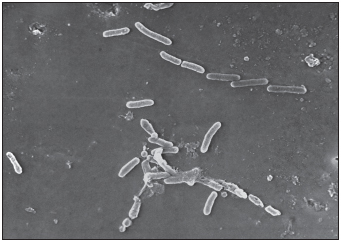
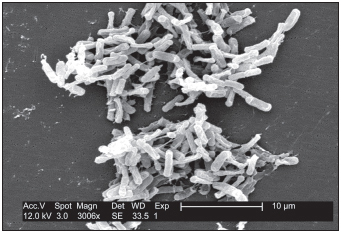
Clostridium difficile is particularly problematic in immunocompromised individuals. This bacterium is a normal inhabitant of the human intestine and a frequent cause of colitis in immunosuppressed persons. A ten-year study of transplant recipients in Minneapolis found an overall incidence of C. difficile–associated colitis of 8%, 16% in pediatric kidney recipients, 15.5% in kidney-pancreas recipients, and 3.5% in adult kidney recipients. The children generally became infected much sooner than the adults (33 days for pediatric kidney transplants versus 15 months for adult kidney transplants). Following general surgery, the incidence of C. difficile colitis is 1% to 4% and is partly linked to prior antibiotic use and length of hospitalization.
Other Bacterial Infections
Several other groups of bacteria covered elsewhere in this text cause more serious infections in immunocompromised persons than in members of the general population. Ehrlichia chaffeensis and Anaplasma phagocytophila, the causative agents of human monocytotropic ehrlichiosis and human granulocytotropic anaplamosis, respectively, are discussed in Chapter Four. Bartonella henselae and B. quintana (Chapter Five) cause bacillary angiomatosis and bacillary pelosis hapatis during late-stage AIDS and in cancer patients receiving chemotherapy.
Probiotic organisms, such as those found in yogurt, may be administered orally to outcompete other typically pathogenic organisms. These probiotic microbes occasionally also cause disease in individuals without a fully competent immune system. One such case involved a person with Sjögren’s syndrome, an autoimmune condition characterized by decreased production of tears and saliva. The patient was treated with immunosuppressive agents to control her inappropriate immune response and subsequently developed a recalcitrant infection with C. difficile in addition to Staphylococcus aureus pneumonia and S. pneumoniae septicemia. After a prolonged course of several broad-spectrum antibiotics failed to contain these bacteria, “biotherapy” with yogurt was instituted. Yogurt contains the probiotic bacterium Lactobacillus rhamnosus, a gram-positive bacillus that rarely causes opportunistic infections. The C. difficile infection subsequently resolved; however, L. rhamnosus caused vancomycin-resistant septicemia with respiratory and cardiovascular dysfunction as well as very high fever. These conditions, as well as S. pneumoniae pneumonia, led to the person’s death. More than 50 other cases of pathological L. rhamnosus infection have been reported in persons with cancer, organ transplant recipients, diabetics, or persons having had recent surgery. The mortality rate is 14%. These cases demonstrate that generally benign and beneficial microbes such as L. rhamnosus that are prescribed to counter C. difficile diarrhea may themselves cause life-threatening infections in debilitated persons receiving immunosuppressive drug therapy.
SEVERAL BACTERIA THAT ARE PROBLEMATIC FOR IMMUNOSUPPRESSED PERSONS
Legionella pneumophila
Pneumocystis jiroveci (carinii)
Mycobacterium species
Pseudomonas aeruginosa
Burkholderia cepacia
Nocardia species
Mycoplasma pneumoniae
Clostridium difficile
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree