Major Concepts
Diseases
Infection with hepatitis C virus (HCV) is very common throughout the world, involving 3% of humans, especially those from the western Pacific, Southeast Asia, and Africa. Chronic infection may result in hepatic or extrahepatic disease manifestations. The hepatic diseases are primarily cirrhosis of the liver and hepatocellular carcinoma. Liver damage may be intensified by alcohol consumption. Extrahepatic diseases include essential mixed cryoglobulinemia (a noncancerous lymphoproliferative disease of B cells), porphyria cutanea tarda (abnormal sensitivity to sun exposure and liver damage due to excessive iron deposition in the liver), Sjögren’s syndrome (an autoimmune syndrome in which production of tears and saliva are decreased), lichen planus (an autoimmune disease with chronic dermal or intraorbital keratinization), rheumatoid arthritis (an autoimmune disease in which synovial tissues are damaged), several malignancies, and renal and myocardial impairments. Most persons infected by the virus, however, remain asymptomatic.
Infection
Hepatitis C virus is a flavivirus, a small, enveloped, single-stranded RNA virus that infects primarily liver cells but may also grow in lymphocytes and monocytes. Several genotypes exist that respond differently to treatment. HCV has a very high mutation rate due to the error-prone nature of its RNA polymerase. Rapid mutations allow the virus to escape killing by CD8+ T killer cells.
Transmission and Populations at Risk
HCV infection usually involves intravenous (IV) drug use, blood transfusion, organ donation, or mother-to-child transmission. The virus survives for long periods of time outside of the body, even on surfaces in a dried condition. Some groups of people have higher rates of infection or develop more severe disease manifestations. These groups include persons of African descent, Hispanics, Asians, older persons, the obese, and alcoholics. Coinfection with HIV also increases disease severity. The reasons for these differential effects are complex and involve socioeconomic factors as well as genetic differences in enzymatic activity and susceptibility to other diseases.
Immune Response
CD8+ T killer cells and NK cells are the most important components of the immune response to HCV. The virus’s high mutation rate allows it to escape killing by T killer cells, which recognize very specific amino acid sequences on their targets. HCV down-regulates expression of stimulatory receptors on NK cells while increasing expression of inhibitory receptors on both NK cells and T killer cells, thus decreasing the cytotoxic activity of both immune cell types. Treg activity is increased in persons infected with HCV. These cells produce TGF-β that blocks activation of other T lymphocytes and inhibit production of the antiviral agent IFN-γ.
Protection
To prevent infection, IV drug use should be avoided, or the injecting supplies should be decontaminated. Health care workers should carefully follow the universal precautions guidelines and disinfect work surfaces and biohazard spills promptly. If infection were to occur, alcohol consumption should be halted. Patients require plenty of rest and may consider receiving a hepatitis A vaccine to decrease further liver damage. The most commonly used treatment regimen is combination therapy with IFN-α and the antiviral agent ribaviran. This regimen is associated with several side effects, some which are severe.
The number of new infections with hepatitis C virus (HCV) in the United States has been decreasing. In the 1980s, 240,000 new infections occurred per year; by 2004, this number had fallen to 26,000. Most HCV infections result from illegal IV drug use. Of the 4.1 million Americans affected by HCV (1.6% of population), 3.2 million have chronic infection.
HCV is the second most common chronic viral infection in world, affecting approximately 3% of the world’s population (180 million people). The areas of the world that are hardest hit are the western Pacific region, Southeast Asia, and Africa. In the United States, infection rates vary from 1% to 2%, while in parts of the developing world, prevalence may reach as high as 7%. This virus contributes to more than 100,000 deaths per year either directly or in connection with alcohol abuse or coinfection with HIV or hepatitis B virus. The number of HCV-related deaths is projected to triple between 2008 and 2020 in the United States. It is estimated that over half of the individuals infected with HCV are not aware of their condition and contribute to the spread of the disease.
In addition to HCV, several other types of hepatitis viruses have been found—A, B, D, and E. Type A is transmitted by being in close contact with infected persons or by contaminated food. This infection is often resolved within six months. Type B is most commonly spread via blood but also via semen or from mother to child. As with HCV, there is an increased risk of liver disease and hepatocellular carcinoma. Effective vaccines have been developed for both type A and type B hepatitis viruses. Hepatitis D virus is able to survive and reproduce only in cells that are coinfected with hepatitis B virus. Approximately 5% of individuals with type B virus also are infected with type D. Hepatitis E virus is most often contracted by consuming contaminated food or water. This virus does not cause chronic infection. Type E infection is rare in the United States and more common in South Asia and North Africa.
Initially, HCV was named “non-A, non-B” hepatitis and was seen in IV drug users and recipients of blood transfusions in the 1970s. The virus was described by two research groups in the Lancet in 1984. Five years later, the Chiron biotech corporation cloned HCV RNA. A test was developed to screen the blood supply in 1990, and an improved test was introduced in 1992, vastly increasing the safety of blood transfusion. The current test detects 95% to 99% of positive blood samples. It is not as widely available in the developing world, where the risk of iatrogenic infection is higher.
Several famous Americans have contracted HCV. This virus curtailed the career of country singer Naomi Judd, who was infected by a needle prick while she was a nurse. Actress Pamela Anderson was infected via a tattoo needle. Motorcycle daredevil Evel Knievel acquired hepatitis C, most likely through a blood transfusion following an accidental spill. He received a liver transplant to replace his damaged organ. Newsman Frank Reynolds and actor-singer Jim Nabors also contracted this disease. Baseball great Mickey Mantle is believed to have been a victim of the unfortunate combination of HCV infection and cirrhosis of the liver induced by excessive alcohol consumption.
For approximately 60% to 85% of persons infected with HCV, infection will become chronic. The long-term nature of this illness is due to the rapid rate at which the virus mutates, allowing continual evasion of antibodies directed against its components. Spontaneous resolution occurs in 0.5% to 0.7% of those with chronic disease; death from hepatic or extrahepatic damage occurs in 1% to 5%.
The majority of individuals infected with HCV (80%) are asymptomatic. For the remaining 20%, symptoms include jaundice, fatigue, dark urine, pain in the right abdominal quadrant, loss of appetite, nausea, vomiting, low-grade fever, pale or clay-colored stools, generalized itching, ascites (fluid in abdominal cavity), and dilated veins in the esophagus. The diseases associated with this viral infection may be broken down into hepatic diseases (involving the liver) and extrahepatic diseases (involving other areas of the body).
Hepatic Diseases
Chronic liver diseases affect 70% to 80% of symptomatic persons. Due to the large number of people affected and the severity of the hepatic damage, HCV infection is the leading cause of liver transplantation in the United States. Following transplantation, however, HCV may infect the new liver and damage it as well. This has led some researchers to examine the possibility of using baboon livers instead of human livers for the transplants. Such xenotransplants (transplants using organs from other species) are almost always rapidly rejected, even when strong immunosuppressive drugs are administered.
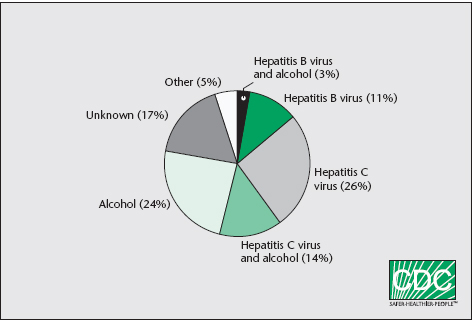
FIGURE 18.1 Primary causes of chronic liver disease
Note: Based on data for Jefferson County, Alabama.
Source: CDC/NCID.
Many people with hepatic manifestations (20% to 30%) develop cirrhosis of the liver (irreversible liver scarring) after 20 to 30 years. Alcohol consumption increases the risk of developing this condition and should be avoided. Symptoms of cirrhosis include jaundice, weakness, weight loss, nausea and vomiting, swelling of the legs, bleeding hemorrhoids, the development of small spiderlike blood vessels in the skin, and impotence and loss of interest in sex. The damage to the liver cannot be repaired, nor can its functioning be restored. Liver transplantation may be recommended in life-threatening cases.
Hepatocellular carcinoma, a form of liver cancer, occurs in 1% to 5% of chronically infected individuals. It is responsible for 80% to 90% of all liver cancers and is seen more commonly in men than in women. The disease typically affects persons in their fifties and is present in Africa and Asia to a greater extent than other areas of the world. If this form of cancer is detected early, small or slow-growing tumors may be successfully treated by aggressive surgery or liver transplantation. Early diagnosis is, however, unusual. Chemotherapy and radiation treatments are not usually curative but may shrink large tumors prior to surgery. Sorafenib toslate may inhibit tumor growth.
Extrahepatic Diseases
Areas other than the liver may also be adversely affected by HCV. Chronic HCV infection has been linked to insulin resistance and can lead to type 2 diabetes. The development of insulin resistance is associated with a rapid progression to fibrosis and cirrhosis, resulting in hepatocellular fibrosis or liver failure. Individuals with insulin resistance often respond poorly to antiviral therapy.
Some of the pathology of the extrahepatic diseases results from inappropriately stimulated immune responses and involves excessive growth of lymphocytes or excessive lymphocyte activation. Essential mixed cryoglobulinemia (EMC) is one such extrahepatic disease associated with HCV infection. This condition is a noncancerous lymphoproliferative disease characterized by abnormally high levels of B cell growth that may be associated with decreased apoptosis resulting from a rearrangement of the antiapoptotic protein bcl-2 and Ig JH due to a t(14;18) chromosomal translocation, which leads to the constitutive production of the former. These B cells produce unusual types of antibodies called cryoglobins due to their tendency to precipitate out of solution at temperatures below that of the human body (37°C or 98.6°F). They are of a mixed nature in that both polyclonal IgG, monoclonal IgM, or polyclonal IgM with rheumatoid factor activity antibodies are involved. EMC symptoms include weakness, arthralgia, kidney disease progressing to renal insufficiency, purpura, Raynaud’s phenomenon (extremities become whitish-blue when exposed to cold), peripheral neuropathy, and lung and liver damage. These symptoms are secondary to systemic vasculitis due to vascular deposition of immune complexes. Cryoglobins may be detected in 70% of individuals with chronic HCV infection.
Another HCV-related condition is porphyria cutanea tarda, which results from excessive iron deposits in the liver. Excess iron decreases uroporphyrinogen decarboxylase activity and increases urinary excretion of several porphyrins. Symptoms of this disorder include abnormal sensitivity to sun exposure and liver damage.
Various types of renal impairments are associated with HCV. These include membranoproliferative glomerulonephritis, membranous nephropathy, mesangial proliferative glomerulonephritis, Henoch-Schönlein purpura nephritis, and tubulointerstitial nephritis. The underlying cause of these conditions may be the formation of immune complexes of IgM κ chains with rheumatoid factor activity. These impairments may occur in 2.7% (membranous nephropathy) to 17.6% (mesangial proliferative glomerulonephritis) of persons infected with HCV virus and indicate a poor prognosis.
Several types of cancers are associated with infection with HCV. One of these involves abnormal growth of infected lymphocytes, B cell non-Hodgkin’s lymphoma, which may be found in sites such as the salivary glands and the liver. Splenic lymphoma, diffuse large B cell lymphoma, and monoclonal gammopathies of uncertain significance are other associated lymphoproliferative disorders. Other malignancies linked with HCV infection include oral and thyroid cancers and cervical squamous cell carcinoma.
Myocardial impairments may also result from HCV infection. The heart damage may result from an immune response to HCV, whose RNA has been detected in cardiac muscle tissue.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree