Step 1
Surgical Anatomy
- ♦
A thorough knowledge of the surgical anatomy is mandatory for lymph node dissection of the neck.
Cervical Lymph Node Levels
- ♦
The lymph node regions of the neck are shown in Figure 5-1 .
- ▴
Level I contains the submental and submandibular lymph nodes.
- ▴
Levels II through IV contain lymph nodes along the internal jugular vein and medial to the sternocleidomastoid muscle. The carotid bifurcation marks the boundary between levels II and III; the superior belly of the omohyoid separates levels III and IV.
- ▴
The posterior triangle of the neck, level V, is bounded by the posterior border of the sternocleidomastoid muscle, the anterior border of the trapezius, and the clavicle. In thyroid cancer, supraclavicular nodes medial to the sternocleidomastoid muscle are the most commonly involved lateral cervical lymph nodes.
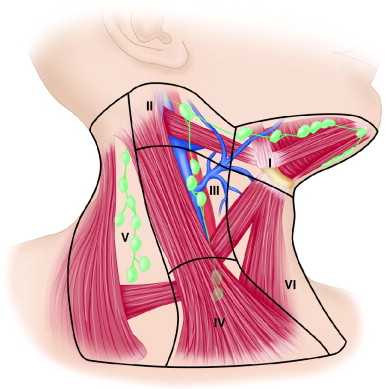
Figure 5-1
- ▴
Spinal Accessory Nerve
- ♦
The spinal accessory nerve exits the skull base and travels deep to the posterior belly of the digastric muscle and stylohyoid muscles, just posterior to the internal jugular vein. The nerve enters the sternocleidomastoid muscle on its medial surface, approximately 2 cm inferior to the mastoid tip.
- ♦
The spinal accessory nerve frequently branches within the substance of the sternocleidomastoid muscle, giving off a branch to the muscle and continuing on into the posterior triangle to innervate the trapezius muscle. Occasionally, the spinal accessory nerve branches before penetrating the sternocleidomastoid muscle.
- ♦
In the posterior triangle, the accessory nerve may be identified 1 cm above Erb’s point, where the great auricular nerve wraps around the posterior edge of the sternocleidomastoid muscle. The nerve courses posteriorly and inferiorly within the posterior triangle in a relatively superficial plane and runs along the medial surface of the trapezius muscle before innervating it.
Thoracic Duct
- ♦
Involvement of level IV with metastatic thyroid cancer is common. A thorough dissection of level IV, an important part of neck dissection for thyroid cancer, places the thoracic duct at risk for injury.
- ♦
The thoracic duct enters the base of the neck behind the common carotid artery, extends forward and laterally, passing anteriorly to the anterior scalene muscle and phrenic nerve, and opening into the venous system at the junction of the internal jugular vein and the subclavian vein. Frequently, before entry, the duct arborizes into fine thin-walled vessels, making injury difficult to avoid.
Trapezius Muscle and Levator Scapulae
- ♦
The trapezius is a fan-shaped muscle, which, in combination with other muscles, including the levator scapulae and rhomboid, stabilizes the scapula and shoulder girdle during arm movement. Injury to the accessory nerve or to the nerves to the levator scapulae muscle (by means of the fourth and fifth cervical nerves) predisposes to shoulder pain and dysfunction, characterized by shoulder drop and limitation in arm abduction. Gentle and meticulous dissection of the spinal accessory nerve and preservation of the nerves to the levator scapulae can prevent these sequelae.
Cervical Plexus ( Fig. 5-2 )
- ♦
The cervical plexus, which contains the ventral rami of C1-C4, provides sensory innervation to the head and neck via the great auricular nerve, greater and lesser occipital nerves, transverse cervical nerve, and supraclavicular sensory nerves. These sensory roots are frequently severed during neck dissection, but may sometimes be preserved.
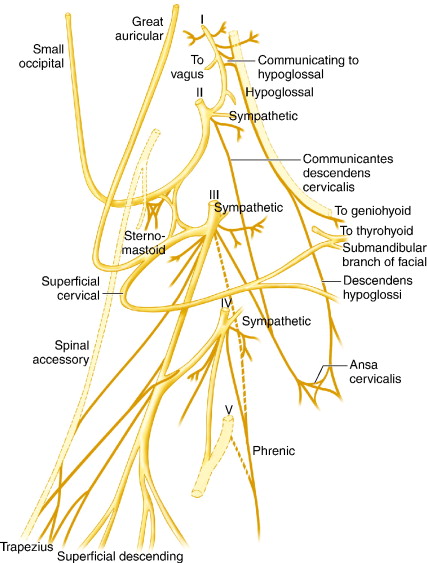
Figure 5-2
- ♦
Sacrifice of motor branches providing motor innervation to the deep muscles of the neck (levator scapulae, splenius capitis, scalene muscles) exacerbates shoulder dysfunction after neck dissection. A communicating branch to the accessory nerve may sometimes be preserved.
- ♦
Ligation of the cervical rootlets high on the specimen is performed to avoid injury to the phrenic nerve.
Step 2
Preoperative Considerations
Preoperative Staging
- ♦
Before surgery, patients with thyroid malignancies should undergo an ultrasound evaluation of the thyroid gland and neck as part of preoperative staging. Abnormal nodes in the lateral neck may be identified before surgery, and the patient may be counseled regarding the need for lateral neck dissection.
- ♦
Although a computed tomography scan of the neck ( Fig. 5-3 ) is not usually recommended as part of the workup of thyroid cancer, metastatic papillary carcinoma has a distinctive appearance on this type of imaging.
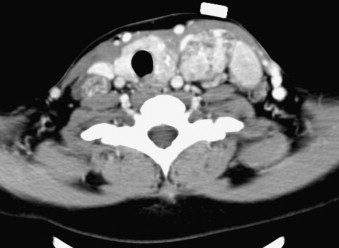
Figure 5-3
- ♦
Lateral neck dissection confers no survival advantage when performed prophylactically but improves recurrence-free survival for patients with nodal disease on imaging studies such as ultrasound. Thus, nodal dissection of the lateral compartment is recommended to improve regional control and enhance the efficacy of subsequent radioiodine ablation for this subset of patients.
- ♦
Papillary thyroid carcinomas and medullary thyroid carcinomas are associated with a high incidence of metastatic disease to the lateral neck. Reported rates of metastatic disease to the lateral cervical lymph nodes from papillary thyroid cancer have ranged between 11% and 80%. The risk of spread to the neck is lower in patients with the follicular variant of papillary carcinoma, whereas the incidence of lymph node metastases from follicular cancers is low.
- ♦
Other factors associated with lymph node metastases include evidence of extrathyroid extension and youthful patient population. In general, nodal metastases are believed to increase local recurrence risk and reduce survival in those older than age 45 years. The frequency of lymph node metastases by neck level is listed in Figure 5-4 .
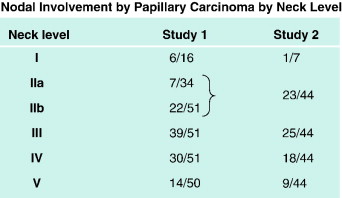
Figure 5-4
Extent of Neck Dissection
- ♦
Lymph node metastases from thyroid carcinoma usually occur first in the paratracheal nodes, although skip metastases into the lateral compartment are not uncommon. Reviews of the pattern of nodal metastases have noted that the majority of patients harbor metastatic disease at multiple levels, with levels II to V being most commonly involved.
- ♦
Level I is dissected when clinically involved by disease. Incomplete nodal dissections, including berry-picking operations, have been associated with higher rates of regional recurrence. For this reason, a comprehensive neck dissection of levels II through V is recommended for patients with clinical evidence of nodal metastases in the lateral compartment.
“Functional” Neck Dissection
- ♦
In the majority of patients with metastatic thyroid carcinoma, a “functional” neck dissection with preservation of the spinal accessory nerve, internal jugular vein, and sternocleidomastoid muscle may usually be performed because papillary carcinoma has a low tendency to invade these structures.
- ♦
Because many patients live a long time after surgery, quality of life is important. Nevertheless, even with preservation of the nerve, weakness of the trapezius muscle may result due to neurapraxia and, later on, adhesive capsulitis. Such complications may be diminished using several strategies: atraumatic dissection of the accessory nerve in the posterior triangle, preservation when possible of the communicating branch of the cervical contribution to the accessory nerve, and aggressive physical therapy.
- ♦
At our institution, patients undergo a preoperative evaluation and counseling by our physiatry department. Such interventions preserve range of motion during recovery from neurapraxia. In some patients, preservation of cervical nerves, including the great auricular nerve, may be possible, resulting in more expeditious recovery of sensory dysfunction after surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree