Major Concepts
Outbreak
Lyme disease was first reported in Connecticut in 1976 as an outbreak of arthritis in an unusually large number of children and adults. It was later found to result from infection by a tickborne spirochete bacterium. A spirochete is a spiral-shaped, rodlike bacterium that has caused diseases such as syphilis and relapsing fever. Nymphal and larval forms of the tick transmit the spirochete to humans. Disease incidence is highest during spring and summer when these ticks are seeking new hosts.
Symptoms
The symptoms of Lyme disease include a combination of a tick bite with or without the presence of a tick, an erythema migrans rash, fever, chills, fatigue, weight change, hair loss, swollen glands, sore throat, irritable bowel, chest pain, shortness of breath, heart palpitations, joint pain and stiffness, muscle pain, headache, tingling or numbness, facial paralysis, double vision, buzzing or ringing in the ears, dizziness, poor balance, light-headedness, difficulty walking, tremor, heart murmur, confusion, forgetfulness, poor short-term memory, mood swings, meningitis, sensitivity to light, recurring hepatitis, and adult respiratory distress syndrome. Lack of prompt treatment may lead to persistent fatigue or malaise, migratory musculoskeletal disorders, chronic encephalopathy and encephalomyelitis, peripheral neuropathy, and difficulty with concentration or memory.
Setting
Lyme disease in the United States occurs primarily in the Northeast along the coast from Maine to Maryland, in portions of the Midwest, and in parts of the Far West. It is also found in temperate areas of Canada, Europe, Africa, Asia, and Australia. Incidence of Lyme disease has been on the rise due to increased habitats for the tick vectors and the mice and deer on which they feed. The rising incidence is also influenced by greater use of tick habitat by humans and an increase in the construction of human residences in these regions. Southern-tick-associated rash illness (STARI) is a similar disease found in the American Southeast. It results from infection with Borrelia lonestari, transmitted by the bite of the lone star tick.
Infection
Lyme disease is the result of infection by genospecies of Borrelia burgdorferi sensu lato. These are gram-negative, flagellated spirochetes, similar to the causative agent of syphilis. Over 300 strains of these bacteria are found worldwide. In Europe and Africa, B. afzelii and B. garinii may also cause Lyme disease, while B. japonica and B. miyamoto cause the disease in Japan. Borrelia species have a small linear chromosome and up to 9 circular and 12 linear plasmids. These plasmids are involved in the infection of mammals and ticks and in drug resistance. The spirochetes contain very limited numbers of biosynthetic proteins, relying instead on the host for most of their nutritional needs (importantly, B. burgdorferi does not require iron for survival, permitting it to avoid host defense mechanisms that limit microbial access to iron). Following a localized skin infection, bacteria enter the blood and cerebrospinal fluid and may migrate to the myocardium of the heart, retina, muscle, bone, spleen, liver, meninges, and brain. As systemic infection declines, some organisms persist for years in areas such as the joints, nervous system, and skin.
Immune Response
The reaction of the immune system to B. burgdorferi is complex, involving complement-mediated lysis, antibody production by B lymphocytes, Th1 cytokine secretion by T helper lymphocytes, activation of macrophages, and phagocytosis by neutrophils. These cells, acting together, kill bacteria and limit their dissemination. The immune response may, however, also induce pathology. Persons suffering from moderate to severe arthritis often have very high levels of antibody in their blood and joints, which may contribute to arthritis. The bacteria trigger macrophages to produce proinflammatory cytokines such as IL-1 β, TNF-α, and IL-6, worsening joint damage. Borrelia also have mechanisms to evade the immune system, such as complement regulatory factors, rapid antigenic variation to avoid recognition by T cells, and triggering apoptotic death pathways in macrophages.
Medicinal Therapy
Various bacteriostatic or bacteriocidal drugs are available to treat Lyme disease, including the tetracyclines, doxycycline, minocycline, penicillins (amoxicillin but not penicillin G), macrolides, and cephalosporins. These vary widely in their ability to penetrate tissues and enter the central nervous system. Antibiotic use may result in the Jarish-Herxheimer reaction, a temporary increase in discomfort due to shedding toxins released by dead spirochetes stimulating an intense immune response.
Prevention
Ticks are found mainly in leaf litter and low-lying vegetation. Prevention of Lyme disease involves avoiding tick habitat; wearing light-colored, protective clothing that covers the arms and legs; wearing closed shoes; and using tick repellents containing DEET (an oily, colorless chemical that is the active ingredient in the most widely used insect repellents that may be safely applied to the skin) on clothing and exposed skin. The removal of leaf litter, tall grass, woodpiles, and brush from residential areas may reduce vector and reservoir habitat. Following visits to tick-inhabited areas, it is essential to inspect the skin and hair, and promptly remove ticks using methods that completely eliminate all tick parts.
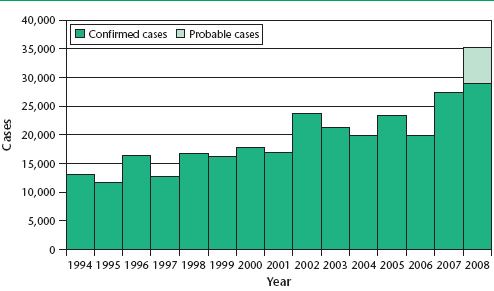
Lyme disease, spread by the bite of deer ticks, is the most prevalent arthropod-borne illness in temperate climates due to reforestation, decreased hunting, increased human habitation near woodlands, and the subsequent increases in deer numbers and in human-deer interactions. First reported in Connecticut, this disease has been found in all states in the United States. It is concentrated in three regions: the Northeast coast from Maine to Maryland, the Midwestern states of Wisconsin and Minnesota, and parts of the Far West. It is endemic in New York, New Jersey, Connecticut, Pennsylvania, Massachusetts, Rhode Island, Delaware, Maryland, Wisconsin, Minnesota, California, and Oregon. While the absolute number of cases in the United States are highest in New York and Pennsylvania, the incidence is highest in Delaware (77 per 100,000 population) and Connecticut (51 per 100,000). Numbers of cases in other coastal or midwestern states are increasing as the causative bacterium, Borrelia burgdorferi, spreads to new areas. It is estimated that only 10% of the true number of cases are accurately diagnosed and reported to the Centers for Disease Control and Prevention. Lyme disease also occurs in Canada, much of Europe, the former Soviet Union, northern China, Japan, North Africa, and eastern Australia. The areas of Europe with highest incidence of disease are Germany, Austria, Slovenia, and Sweden, in which the infection rate approaches that of Connecticut.
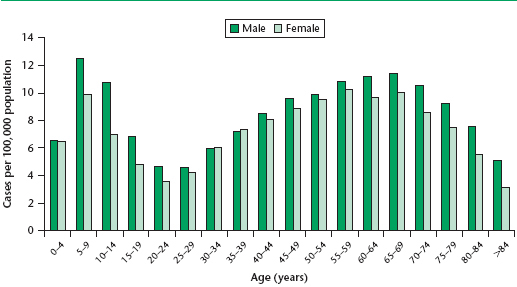
In the United States, Lyme disease most commonly strikes individuals between the ages of 5 and 14. Incidence decreases between the ages of 15 and 30 and then slowly increases until 70 years, followed by declining numbers in older persons. Males are infected at a higher rate than females, perhaps due to a greater exposure to ticks.
Table 3.1 Incidence of Lyme disease by state
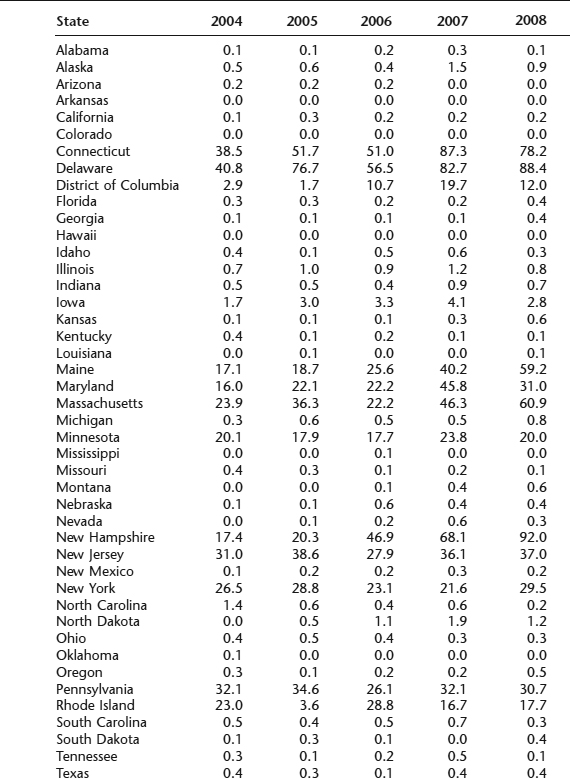
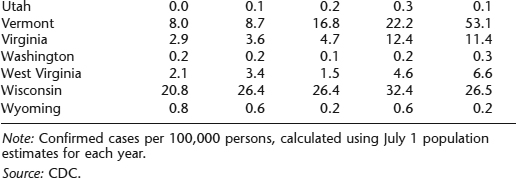
FIGURE 3.1 Annual incidence of reported cases of Lyme disease in the United States, by age group and sex, 1992–2004
Note: Age- and sex-specific incidence was calculated using Census Bureau population estimates for July 1, 2000.
Source: CDC.
Lyme disease was named after the town of Old Lyme, Connecticut, where it was reported in 1976 to cause an unusually large number of arthritis cases in children (39 cases in children and 12 in adults). The arthritis presented as intermittent episodes of asymmetric pain and swelling, particularly in large joints such as the knees. A search of historical records indicates that a similar condition was reported in 1883 in Breslau, Germany, by Alfred Buchwald, who described a degenerative skin condition, acrodermatitis chronica atrophicans. In the early 1900s, Arvid Afzelius observed a ringlike lesion that he believed resulted from the bite of an Ixodes tick.
In the Americas, Lyme disease was present in Cape Cod during the 1960s. DNA from the causative organism, however, was detected by polymerase chain reaction (PCR) in museum specimens of ticks and mice from Long Island dating from the late nineteenth and early twentieth centuries. After European colonization, much of the habitat required for Lyme disease transmission was removed as wooded areas were cleared for farmland. During the twentieth century, however, much of the area was returned to forests, and the deer, rodent, and tick populations grew, as did the incidence of Lyme disease. This disease now affects suburban locations in some of the most heavily populated regions of the country, including Boston, New York, Philadelphia, and Baltimore.
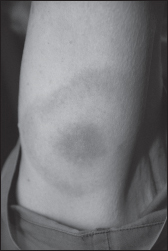
The initial symptoms are known as early localized Lyme borreliosis and include a rash, erythema migrans (EM), in 60% to 80% of infected individuals. This rash appears between 2 and 30 days after the bite of an infected tick and often has a bull’s-eye appearance that may be circular or oval. The rash may be quite large, up to 30 inches in diameter. It is often accompanied by a nonspecific fever.
Although up to 10% of infections may be asymptomatic, Lyme disease is usually associated with a variety of symptoms that allow it to be confused with other diseases. It presents as a combination of several of the following symptoms: tick bite, erythema migrans rash at the tick bite site or other areas, fever, chills, sweats, fatigue, weight change, hair loss, swollen glands, sore throat, irritable bowel, chest pain or rib soreness, shortness of breath, heart palpitations, joint pain or swelling, stiffness of joints, neck, or back, muscle pain, headache, tingling or numbness, facial paralysis (such as Bell’s palsy), double or blurry vision, buzzing or ringing in the ears, dizziness or poor balance, light-headedness or difficulty walking, tremor, heart murmur, confusion, difficulty thinking, forgetfulness, poor short-term memory, disorientation, mood swings, meningitis, sensitivity to light in the eyes, mild transient or recurring hepatitis, or adult respiratory distress syndrome. Patients do not manifest all of the listed symptoms. If the infection is not promptly treated in a manner leading to its elimination, several manifestations may occur several years later, including persistent fatigue and malaise, together with migratory musculoskeletal disorders, such as Lyme arthritis, chronic encephalopathy and encephalomyelitis, peripheral neuropathy, and difficulty with concentration and memory. These symptoms are believed by some to result from persistent infection. Host immunogenetic background may influence disease course, with individuals with major histocompatibility complex class II HLA-DRB1*0401 and 0101 alleles at increased risk for chronic joint inflammation or nonresponsiveness to antibiotic therapy. Coinfection with the protozoan parasite Babesia microti or the bacterial causative agent of human granulocytic ehrlichiosis, both transmitted by deer ticks and endemic to regions with high incidence of Lyme disease, may lead to acute flulike symptoms.
A disease similar to Lyme disease, southern-tick-associated rash illness (STARI), is present in the American Southeast and is transmitted by the bite of the lone star tick, Amblyomma americanum. This tick carries a newly described spirochete, Borrelia lonestari. This spirochete may be widespread in the southeastern United States.
Borrelia burgdorferi was isolated by William Burgdorfer at the Rocky Mountain Laboratory in 1981. Lyme disease results from infection with genospecies of B. burgdorferi
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree