Lung Resection
CRITICAL ELEMENTS
Surgical Approach
Chest Exploration
Flexible Bronchoscopy
Lung Isolation
Mediastinal Exploration for Gross Nodal Disease
1. SURGICAL APPROACH
Recommendation: Pulmonary resection can be approached safely through a thoracotomy or thoracoscopically depending on the extent of the disease and the surgeon’s experience and preference.
Type of Data: Retrospective, Prospective.
Strength of Recommendation: Weak.
Rationale
Video-assisted thoracoscopic surgery (VATS) approaches, which are being used with increasing frequency, can be performed safely by experienced thoracic surgeons.1,2,3 Compared with standard thoracotomy, VATS may cause less postoperative pain and morbidity while offering equivalent survival and recurrence rates.4,5,6 VATS lobectomy has become a standard approach for early-stage lung cancer and is being used increasingly for more advanced disease. According to the American College of Chest Physicians Clinical Practice Guidelines, a minimally invasive approach is preferable to a thoracotomy for anatomic pulmonary resection for stage I non-small cell lung carcinomas in experienced centers.7 In addition, VATS may enable patients to receive adjuvant chemotherapy earlier.8 Relative contraindications to VATS include the
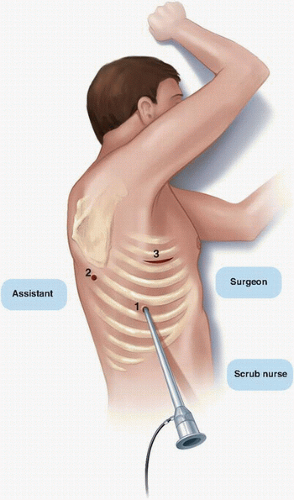
inability to completely resect the tumor with a lobectomy, the inability to tolerate one-lung ventilation, T3 or T4 tumors, and N2 or N3 disease.9 The incisions used in thoracoscopic lobectomy include incisions for an inferior port for the camera and for one or two additional ports anteriorly or posteriorly in the sixth intercostal space for the retraction and passage of the stapler (Fig. 9-1). A 6- to 8-cm utility incision for removal of the specimen is made in the fourth intercostal space overlying the hilum. A specimen retrieval bag should be used to decrease the risk of tumor seeding at the incision.10 Rib spreading should not be used.
inability to completely resect the tumor with a lobectomy, the inability to tolerate one-lung ventilation, T3 or T4 tumors, and N2 or N3 disease.9 The incisions used in thoracoscopic lobectomy include incisions for an inferior port for the camera and for one or two additional ports anteriorly or posteriorly in the sixth intercostal space for the retraction and passage of the stapler (Fig. 9-1). A 6- to 8-cm utility incision for removal of the specimen is made in the fourth intercostal space overlying the hilum. A specimen retrieval bag should be used to decrease the risk of tumor seeding at the incision.10 Rib spreading should not be used.
Although thoracotomy or thoracoscopic approaches can be used to safely perform pulmonary resection, experienced surgeons must know which approach to use for each patient and when it is necessary to convert a thoracoscopic surgery to an open thoracotomy.
Regardless of VATS or open approach, the patient is positioned in the lateral decubitus position, and the operating table is flexed to help widen the intercostal spaces. All pressure points should be padded. The thoracotomy incision is positioned for optimal exposure of the hilum and should have the capacity to be
rapidly extended if needed. An oblique skin incision is made 1 or 2 fingerbreadths below the scapular tip.
rapidly extended if needed. An oblique skin incision is made 1 or 2 fingerbreadths below the scapular tip.
Although no controlled studies have compared standard posterolateral thoracotomy to muscle-sparing thoracotomy, muscle-sparing thoracotomy may cause less pain and result in better postoperative pulmonary function and shoulder function preservation.11,12,13 The latissimus dorsi muscle is mobilized either posteriorly or anteriorly, and the serratus anterior muscle is mobilized anteriorly or spread along the direction of its fibers. The chest is entered through the fifth intercostal space, and a 1-cm segment of the inferior rib is resected to improve exposure. A standard posterolateral thoracotomy incision offers excellent exposure of the hilar structures. The latissimus dorsi muscle is divided, but the serratus anterior muscle can often be spared. If the serratus anterior muscle is divided, it should be divided close to the rib insertions to preserve innervation to the muscle. Surgeons should make an effort to avoid injuring the intercostal nerves, as such injury can cause chronic pain following thoracotomy. Several techniques to reduce the pain from intercostal nerve injury have been described, and these include using intracostal sutures placed through holes drilled in the inferior rib and harvesting a nondivided intercostal bundle prior to thoracotomy to minimize the compression of the intercostal nerves.14,15
2. CHEST EXPLORATION
Recommendation: The chest should be explored visually to evaluate for pleural dissemination of tumor. If such dissemination is confirmed by frozen section or cytologic analysis, the resection should be aborted.
Type of Data: Retrospective.
Strength of Recommendation: Weak.
Rationale
The chest should be thoroughly explored by palpating all lobes for additional nodules and examining the pleural surface. Suspicious lesions should be biopsied and subjected to frozen section analysis. Pleural effusion not identified preoperatively is infrequent and in one study occurred in only 45 of 1,279 (3.5%) patients undergoing lung resection. Of these 45 patients, 24 (53%) had positive pleural lavage cytology findings and 5-year survival rates of 6% to 8%, whereas the patients with negative cytology findings had outcomes similar to those of patients without an effusion.16 In contrast, Naruke et al17 found that 364 of 2,055 (17.7%) patients had previously unidentified pleural effusion at thoracotomy and that of these 364 patients, 74 (20.3%) had positive cytology findings. Pleural fluid or lavage cytology should be obtained and pleurodesis considered in patients found to have an unexpected pleural effusion. However, the use of pleural lavage cytology in the absence of pleural effusion remains controversial; in the American College of Surgeons Oncology Group Z0040 trial, only 29 of 1,047 (2.8%) lung cancer patients had a positive preresection intraoperative pleural lavage.18
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree