27328
Levels of Residential Care in the Elderly and the Role of Cancer Screening
Miriam B. Rodin
The logic of cancer screening makes certain assumptions about the population to be screened, and the clinician needs to understand how well individual patients fit those assumptions. This chapter describes the spectrum of residential settings specialized for the elderly ranging from the fit to the frail, and explains the terminology that is often confusing to nongeriatricians. Correctly identifying the level of support that is offered in each residential type will help clinicians to understand the role of cancer screening in each residential population.
SPECTRUM OF RESIDENTIAL OPTIONS FOR OLDER ADULTS
We tend to use the words nursing home and long-term care interchangeably, but in fact the latter is defined in regulatory language and health finance systems and the former is not. Long-term care is a catchall for a spectrum of medical, rehabilitative, and personal care services given outside of hospitals. With the explosion of the aging population, there is a panoply of residential facilities and housing developments targeted at older adults sorted along a broad spectrum of functional status from “healthy aging” tennis players to bedridden dementia patients. Specifically, although everyone uses the term, there is no such thing as a nursing home. Where people live is a clue to their performance status.
Table 28.1 shows the spectrum of residential options targeted to older adults. “Home” is included here because a substantial amount of postacute and chronic care is delivered in people’s own homes. Home-based care depends heavily on the unpaid care given by family members, often an aging spouse, supplemented by paid caregivers and visiting health professionals (1). If there is a need for assistance but no available caregiver, the rest of the residential options come into play.
There are two basic levels of assistance. The first is for instrumental activities of daily living (IADLs). IADLs are the higher-level functions that include managing money, cleaning the house, going shopping, preparing meals, and so forth. For elderly who do not need any assistance with these, there are “retirement” or “active senior living” communities that are usually downsized private homes or apartments linked to sports, fitness, and recreational centers. There is assistance with groundskeeping, common area, and outdoor maintenance. IADL assistance provides for individual task-based limitations and it allows people to remain safely at home alone. For example, help with housekeeping is often provided by family members. Housekeeping “chore workers” may be provided by the State Departments on Aging at reduced cost. Senior “call-a ride” services substitute for family when elderly give up driving.
274TABLE 28.1 Typology and Characteristics of Residential Options for the Elderly and Disabled, Population Screening Considerations
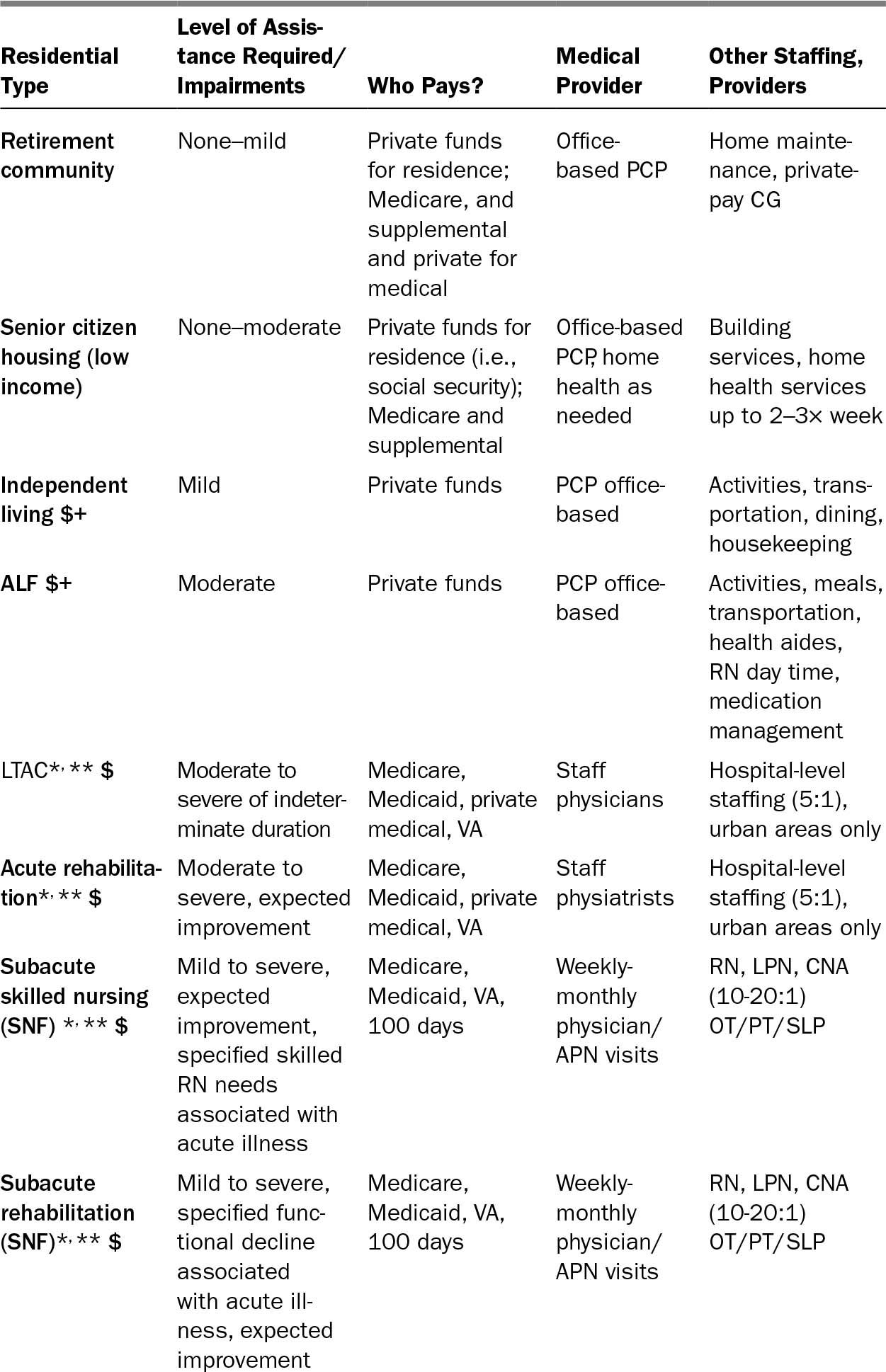
275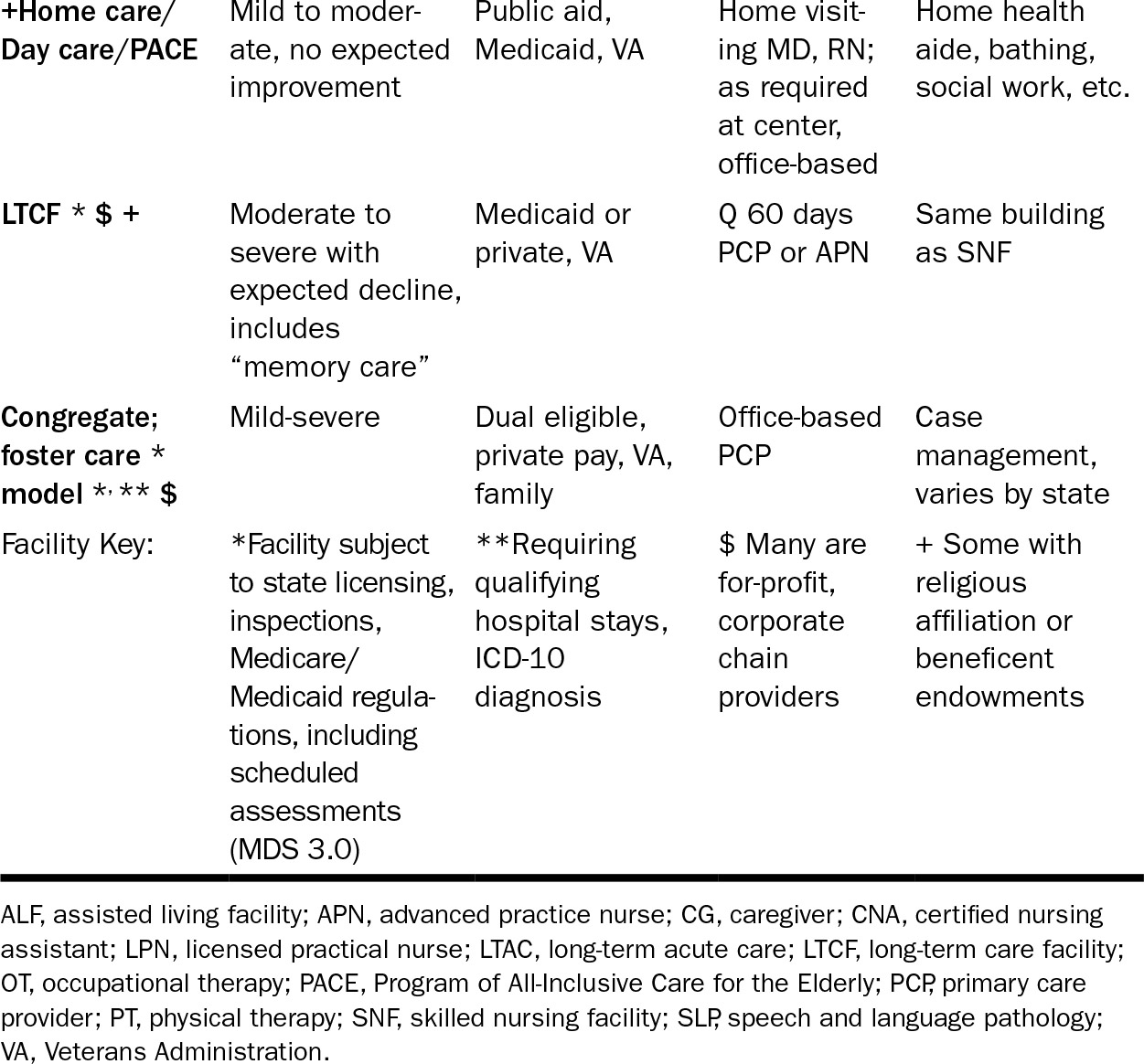
For those who are able to pay privately, “independent living” assumes or anticipates some higher-level instrumental dependence such as need for transportation. “Assisted living” assumes more IADL dependence and assisted living facilities (ALFs) usually advertise their planned recreational activities and dining facilities for elderly who no longer shop and prepare their own meals but are able to socialize (2). ALFs generally also assume mobility problems. The prevalence of walking aids, should there ever be 276a survey, increases from home to independent to assisted living to residential care. ALFs frequently provide medication supervision. Senior residences, independent living, and ALFs are neither defined nor regulated as health care facilities. Medicare does not pay for them (3).
The next level of assistance is for activities of daily living (ADLs). ADLs are the basic self-care activities of eating, bathing, transferring, toileting, taking medications, and making telephone calls that become difficult due to physical illness, disability, and sensory or cognitive decline. An elder’s ability to stay home depends on having a family member or other caregiver there daily. Day care can substitute for home assistance if a working caregiver is there at night. We are often concerned about the safety of ADL-dependent elders who insist on staying home alone. Expressing this concern often elicits an emphatic, “I’m not going into a nursing home.” Some home-based services, such as the VA HBHC (hospital-based home care) and PACE (Program of All-inclusive Care for the Elderly) are specifically designed as nursing home diversionary programs (2). They are targeted to elderly who are homebound and are nursing home appropriate in order to prevent nursing home placement.
The structure or building that is the “nursing home” has two different populations. The basic distinction is whether the stay is a continuation of an acute hospital episode or not, as set out in Medicare Part A. Postacute care is further divided into long-term acute care (LTAC) and subacute care. Additional terms include inpatient rehabilitation and intermediate or stepdown or transitional care. Eligibility for each level is defined by Medicare and supervised by the states with respect to documented functional status and immediate medical history (4). LTAC supplies hospital—indeed, intensive care unit (ICU) level—care indefinitely. Acute (inpatient) rehabilitation hospitals (levels 1–2) provide high-intensity rehabilitation. Skilled nursing facilities (SNFs) and subacute rehabilitation facilities are classified by levels 3 through 7 rehab and three levels of intensity of nursing documented by standardized assessments of the Minimum Data Set (MDS) 3.0 (1).
Medicare Part A was enacted with the original Medicare legislation in 1965. When hospitals were tasked with prospective payment (diagnosis-related groups or DRGs) in the early 1980s, complex patients were discharged to community care facilities that were unprepared to provide the complexity of care these patients required. Historically, they were residences for the elderly who were poor or frail and had no family to care for them. It soon became clear that the situation was unacceptable. The OBRA 1987 regulations specified that structured functional assessments be performed on all residents to find out what and how much care was going to be needed to return Medicare beneficiaries to their homes. In other words, Medicare pays only for short-term care that assumes return to prior level of function.
As shown in Table 28.1, postacute care facilities are covered by private funds, long-term care insurance, Medicare, Medicaid, and VA third-party payers with the expectation that health and performance will improve. When people have either returned to their previous state of health and function or when they plateau, they are discharged or they stay for indefinite residential care, long-term care. Medicare does not pay for that. Medicaid pays for long-term residential care once people have “spent down” their remaining private assets.
277The Medicare Part A–skilled nursing and rehabilitation services are given at home or in subacute facilities and are limited to 100 days per diagnosis per year. Medicare Part A (Med A) will pay 100% of 20 days in a SNF but only charges above the per diem room and board of an additional 80 days of postacute care for a qualifying diagnosis after a qualifying inpatient stay of 3 calendar days. Thus, a patient in subacute care can probably pursue screening after discharge. While they are Med A, the facility has to pay for screenings, and many will not.
WHO LIVES IN THE “NURSING HOME”?
About 1.4 million Americans live in “nursing homes” (5). The majority, 79.1% of long-term acute, postacute, and subacute admissions, came from hospitals (5). The distinctions are how the services are paid for, the specific nursing tasks, and volume of rehabilitation. However, all of these services are located in the same physical structure. The long-term care facility (LTCF) is the same building as the subacute rehab and SNF. In 2016, 33.2% of LTCF residents were there under Medicare A subacute coverage (3). Another source reported that 12.5% of LTCF residents on Medicare A generated 25% of the income for these facilities (2). About one-third of patients admitted to Med A SNF will go home within 30 days, another one-third will go home within 6 months, and one-third will remain as LTCF “custodial care” residents (5). LTCF deaths are concentrated in the first 6 months after admission. Overall, in the first year after “placement,” 50% to 60% of the elderly will die (4–7).
In other words, although we all know what a nursing home is, the real issue is functional status. The vast majority of elderly live at home and receive the bulk of their care from family members (3). Unpaid family caregivers provide an estimated $385 billion in home care that very likely could never be provided by a social welfare or fee-for-service system (8). Living in a facility that is not one’s home where care is not provided by one’s family suggests significant functional dependence.
Functional status has been shown to predict trajectories of further decline in community-living elderly (9). Having used the Medicare A benefit for SNF at all predicts further decline for up to half of beneficiaries (10). There are several validated predictive tools for mortality in hospitalized and nursing home residents (11–13). Dementia is an independent risk factor that confers high risk both for nursing home placement and for 4-year mortality (14–18).
THE LOGIC OF CANCER SCREENING
Physicians who practice in SNFs and LTCFs are aware of the debility of the population and the many reasons to avoid facility-wide policies in favor of cancer screening. Such policies have largely disappeared. The clear majority of LTCF residents, greater than 90%, are unlikely to benefit from cancer screening due to foreshortened life expectancy due to age, comorbidity, and frailty. Many will lack the cognitive capacity to participate in shared decision making about screening or about the treatment of a malignancy if it is found.
278The Cancer in the Elderly working groups have been proactive in urging careful functional screening of elderly cancer patients. Levels of functional impairment that may be subtle in the clinic (19) still have been shown to predict excess toxicity with chemotherapy (20). For that reason alone, residence in a LTCF should prompt a careful assessment of decisional capacity and likelihood of benefit during the best estimate of remaining life expectancy.
Primary care physicians are under pressure to provide “quality” care and meaningful use of electronic health records (EHR). Normal use of EHR in the clinic triggers algorithms requiring responses in real time. Nursing homes rarely have EHR capacity, and residents are generally seen every month or two by an assigned physician or advanced practice nurse. Some elderly continue to see their office-based primary care providers, where they are exposed to guideline-driven care. Table 28.2 summarizes current United States Preventive Services Task Force (USPSTF) (21–27) and American Cancer Society (ACS) (28–30) cancer screening guidelines. Specifically, guidelines are addressed to adults “at average risk” for cancer, but they provide little guidance on application to special populations (31). The American Geriatrics Society and the American College of Physicians, through the Choosing Wisely campaign, have addressed the value of cancer screening in the elderly, specifically advising on how to individualize assessments of burden and benefit conveyed by screening (31). Table 28.2 shows that the guidelines recommend reserving screening for breast cancer, colon cancer, and prostate cancer, all of which have their peak incidence in the elderly, for those with at least a 10-year estimated life expectancy. There are no recommendations for ovarian cancer screening, and elderly women are exempted from cervical cancer screening. Lung cancer screening has relatively recently achieved validation for high-risk individuals up to age 80, with no qualification for life expectancy. Prostate cancer screening is discouraged by the USPSTF (21–27). The ACS guideline on prostate cancer screening does not address older age (28).
TABLE 28.2 Current ACS and USPSTF Adult Screening Guidelines for Breast, Cervical, Uterine/Ovarian, Colorectal, Prostate, and Lung Cancer

279
280Mammography and colon cancer screening have been specifically studied to provide reference estimates to individualize screening decisions for the elderly (32–36). There are population-based estimates of survival (33,34) that show about 25% of elderly beyond the age of 75 do not have a 10-year remaining life expectancy. They are mostly the elderly with multiple comorbidities and functional deficits severe enough to require assistance. This describes the long-term care population.
IS THERE A ROLE FOR CANCER SCREENING IN NURSING HOMES?
The question, “Should nursing home residents be screened for cancer?” can be answered briefly. With few exceptions, cancer screening will not benefit people who live in nursing homes. However, this depends on the examiner’s understanding of what a nursing home is and who lives there. This chapter has presented current population descriptive data showing how the LTC “nursing home” population differs from the average risk population assumed by the screening models. There are some possible circumstances in which cancer screening might be appropriate care for an LTCF resident. The average age of LTC residents is in the mid-80s. About 16% of LTCF residents are under age 65 and another 18% are under age 75 (2,5). The younger group includes adults with developmental disabilities or severe physical disabilities such as brain injuries, quadriplegia, and degenerative diseases. Some are chronically mentally ill adults who may eventually transition to community care. If they are otherwise healthy and able to participate in decision making, the standard population screening recommendations should apply. In particular, mentally ill and disabled women are often at high risk for sexual abuse and have had substandard well woman care. In this case Pap smears and mammograms should be ordered. Heavy smoking is prevalent in this population. Low-dose CT screening for lung cancer and colon cancer screening might be appropriate for patients who can participate in decision making.
Aside from intentional screening, LTCF residents experience frequent hospitalizations during which blood testing and imaging may find an incidental early stage malignancy. Colonoscopy for rectal bleeding, CT to rule out pulmonary embolism (PE), and a prostate-specific antigen (PSA) test ordered by an intern all can find an early stage malignancy. In this event, oncologists are consulted for advice on management. Here, the best way to proceed is to follow the principles of geriatric oncology, weighing the benefit and risk of treating an asymptomatic tumor in a frail elder (19,20). Thinking about the individual patient, if you would not be able to treat it curatively, and then prospectively, it does not seem reasonable to screen for it.
Few elderly residents of “nursing homes” would benefit from cancer screening because of reduced life expectancy, comorbidities that limit treatment options for screen-detected cancers, and inability to participate in informed decision making. Physicians caring for elderly should be familiar with prognostic tools to assist in screening and treatment decision making. Should an oncologist be faced with a screen-detected or incidental early stage malignancy in an elderly person, and a functional assessment reveals dependencies in motor and cognitive function, the web site www.ePrognosis.org is a repository of scales for estimating survival in a range of elderly populations.
281TAKE HOME POINTS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








