Adverse Outcome |
Therapeutic Exposures Associated with Increased Risk |
Factors Associated with Highest Risk |
Recommended Screening |
Adverse psychosocial effects (mental health disorders, risky behaviors, psychosocial disability due to pain, fatigue, limitations in health care and insurance access) |
Any cancer experience |
CNS tumor; cranial irradiation; hearing loss; premorbid learning or emotional difficulties; older age at diagnosis |
Psychosocial assessment with attention to: Educational and/or vocational progress, social withdrawal, anxiety, depression, posttraumatic stress, suicidal ideation, health care and insurance access
Yearly |
Hearing loss |
Cranial irradiation, platinum-based chemotherapy |
Younger age (<4 y) at treatment, increasing radiation and chemotherapy dose |
Complete audiologic evaluation
Baseline at entry to LTFU and as clinically indicated for patients who received platinum; every 5 y for patients who received radiation. |
Cataracts |
Cranial irradiation, total body irradiation, corticosteroids |
Higher radiation dose, combination of steroids and radiation, single daily fraction |
Eye exam (visual acuity, funduscopic exam)
Yearly
Radiation only:
Evaluation by ophthalmologist
Yearly if radiation dose was >30 Gy; every 3 y if radiation dose was <30 Gy |
Dental abnormalities |
Cranial irradiation, any chemotherapy prior to permanent dentition |
Younger age at treatment |
Dental exam and cleaning
Every 6 mo |
Neurocognitive deficits |
Cranial irradiation, intrathecal methotrexate, high-dose methotrexate and cytarabine |
Female sex, younger age (<5 y) at treatment, cranial irradiation, intrathecal methotrexate |
Review of educational and/or vocational progress
Yearly
Neuropsychological evaluation
Baseline at entry to LTFU; repeat as clinically indicated |
Obesity |
Cranial irradiation; neurosurgery involving the hypothalamic-pituitary axis |
Younger age at treatment (<8 y), female sex, cranial irradiation dose >20 Gy |
Height, weight, BMI
Yearly |
Growth hormone deficiency |
Cranial irradiation |
Radiation dose >18 Gy |
Targeted history and physical examination including height, weight, BMI and Tanner staging
Every 6 mo until growth is completed, then yearly |
Precocious puberty |
Cranial irradiation |
Female sex, younger age at treatment, radiation dose >18 Gy |
Height, weight, Tanner staging
Yearly until sexually mature |
Hypothyroidism |
Radiation to the thyroid gland (neck, mantle, etc.) |
Increasing dose, female sex, age at treatment |
Free T4, TSH
Yearly |
Cardiomyopathy/congestive heart failure
Atherosclerotic heart disease, myocardial infarction, valvular disease |
Anthracyclines, chest and spinal irradiation
Chest and spinal irradiation |
High cumulative doses (>500 mg/m2), females, younger than 5 y at treatment, mediastinal irradiation |
Echocardiogram
Every 1 to 5 y as indicated based on age at treatment, anthracycline dose, and history of radiation with potential impact to the heart
Electrocardiogram
Baseline at entry to LTFU; repeat as clinically indicated
Radiation only:
Fasting blood glucose or HgA1C and lipid profile
Every 2 y; if abnormal, refer for ongoing management |
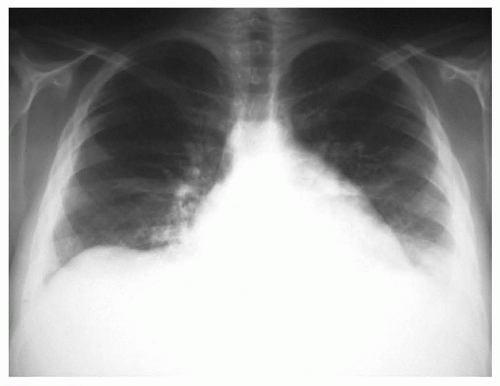
Pulmonary fibrosis/interstitial pneumonitis |
Bleomycin, chest or whole lung irradiation, carmustine, lomustine, busulfan |
Younger age at treatment, bleomycin dose >400 U/m2 |
Pulmonary function tests
Baseline at entry to LTFU; repeat as clinically indicated |
Hepatic dysfunction |
Methotrexate, mercaptopurine, thioguanine, irradiation involving the liver |
Previous veno-occlusive disease of the liver, chronic viral hepatitis |
ALT, AST, total bilirubin
Baseline at entry to LTFU; repeat as clinically indicated |
Renal dysfunction (glomerular and/or tubular) |
Platinum-based therapy, ifosfamide, high-dose methotrexate, abdominal irradiation, surgery |
High-dose chemotherapy, younger age, abdominal radiation, and chemotherapy |
Blood pressure, urinalysis
Yearly
Serum BUN, creatinine, and electrolytes including calcium, phosphorus, magnesium
Baseline at entry to LTFU; repeat as clinically indicated |
Bladder complications |
Alkylating agents, abdominal irradiation, surgery |
Use of high-dose alkylating agents without bladder uroprophylaxis, abdominal radiation |
Targeted history, urinalysis
Yearly |
Hypogonadism (acute or premature ovarian failure in females) |
Alkylating agents, craniospinal irradiation, abdomino-pelvic irradiation, gonadal irradiation |
Treatment during peripubertal or postpubertal period in girls, higher cumulative doses of alkylators; gonadal irradiation |
Pubertal onset, tempo, Tanner staging
Yearly until sexually mature
Females: Serum FSH, LH, estradiol
Baseline at age 13, repeat as clinically indicated
Males: Serum testosterone
Baseline at age 14, repeat as clinically indicated; ideally obtain in the morning |
Infertility |
Alkylating agents, craniospinal irradiation, abdomino-pelvic irradiation, gonadal irradiation |
Males sex; higher doses of alkylators; gonadal irradiation; total body irradiation |
Females:
Targeted history and physical examination
Yearly
Males: Semen analysis
At request of sexually mature patient
Males: FSH
If unable to obtain semen analysis |
Short stature; musculoskeletal growth problems |
Cranial irradiation, corticosteroids, total body irradiation |
Younger age at treatment, cranial radiation dose >18 Gy, unfractionated (10 Gy) total body irradiation |
Standing and sitting height
Yearly until growth completed |
Scoliosis/kyphosis |
Radiation involving the chest, abdomen, or spine; thoracic surgery; neurosurgery-spine |
Younger age at irradiation, higher radiation doses; hemithoracic, abdominal, or spinal surgery |
Spine exam for scoliosis and kyphosis
Yearly until growth completed; may need more frequent assessment during puberty |
Reduced bone mineral density |
Corticosteroids, craniospinal irradiation, gonadal irradiation, total body irradiation |
Associated hypothyroidism, hypogonadism, growth hormone deficiency |
Bone density evaluation (DEXA or quantitative CT)
Baseline at entry to LTFU; repeat as clinically indicated |
Avascular necrosis |
Corticosteroids, high-dose radiation to any bone |
Dexamethasone, adolescence, female sex |
Targeted history and physical examination
Yearly |
Life-threatening infection |
Splenectomy, radiation impacting the spleen (>40 Gy), chronic active graft-versus-host disease |
Anatomic asplenia; higher radiation doses to the spleen; ongoing immunosuppression; hypogammaglobulinemia |
Blood culture
When febrile, temperature > 101°F (>38.3°C) |
Chronic Hepatitis C Virus (HCV) infection and HCV-related sequelae |
Transfusions before 1993 |
Living in hyperendemic area |
Hepatitis C antibody
Once if treated prior to 1993 (date may vary for international patients)
Hepatitis C PCR
Once in patients with positive Hepatitis C antibody |
Therapy-related myelodysplasia, therapy-related acute myeloid leukemia |
Alkylating agents, epipodophyllotoxins, anthracyclines |
Increasing dose of chemotherapeutic agents, older age at therapeutic exposure, autologous hematopoietic cell transplant |
Targeted history/physical examination
Yearly |
Skin cancer (basal cell, squamous cell, melanoma) |
Radiation (any field) |
Orthovoltage radiation (prior to 1970)—delivery of greater dose to skin, additional excessive exposure to sun, tanning booths |
Physical examination
Yearly |
Secondary brain tumor |
Cranial irradiation |
Increasing dose, younger age at treatment |
Targeted history and neurologic examination
Yearly |
Thyroid cancer |
Radiation to the thyroid gland (neck, mantle, etc.) |
Increasing dose up to 29 Gy, female sex, younger age at radiation |
Physical examination
Yearly |
Breast cancer |
Chest irradiation |
Increasing dose, female sex, longer time since radiation |
Females:
Clinical breast exam
Yearly beginning at puberty until age 25, then every 6 mo
Mammogram and breast MRI
Yearly for patients who received >20 Gy beginning 8 y after radiation or at age 25, whichever occurs last. For patients who received 10-19 Gy, clinician should discuss benefits and risks/harms of screening with patient; if decision made to screen, then follow recommendations for >20 Gy |
Colorectal cancer |
Abdominal/pelvic irradiation Spinal irradiation |
Higher radiation dose to bowel; higher daily dose fraction; combined with chemotherapy (especially alkylators) |
Colonoscopy
Every 5 y (minimum) for patients who received >30 Gy, beginning 10 y after radiation or at age 35 y, whichever occurs last; more frequently if indicated based on colonoscopy results. Monitoring of patients who received total body irradiation without additional radiation potentially impacting the colon/rectum should be determined on an individual basis. |
ALT, alanine aminotransferase; AST, aspartate aminotransferase; BMI, body mass index; BUN, blood urea nitrogen; CT, computed tomography; DEXA, dual x-ray absorptiometry; FSH, follicle-stimulating hormone; Gy, Gray; HgA1C, hemoglobin A1C; HIV, human immunodeficiency virus; IV, intravenous; LH, luteinizing hormone; LTFU, long-term follow-up; MRI, magnetic resonance imaging; N/A, not applicable; PCR, polymerase chain reaction; T4, thyroxine; TSH, thyroid-stimulating hormone. |
Screening recommendations are based on the Children’s Oncology Group Long-Term Follow-Up Guidelines, Version 4.0, available in their entirety at www.survivorshipguidelines.org. |