Fig. 13.1
(a) Hemangioma with sole cutaneous infiltration. (b) Typical postinterventional mauve purpura (ointment applied). (c) After one treatment only faint residuals left for further spontaneous regression
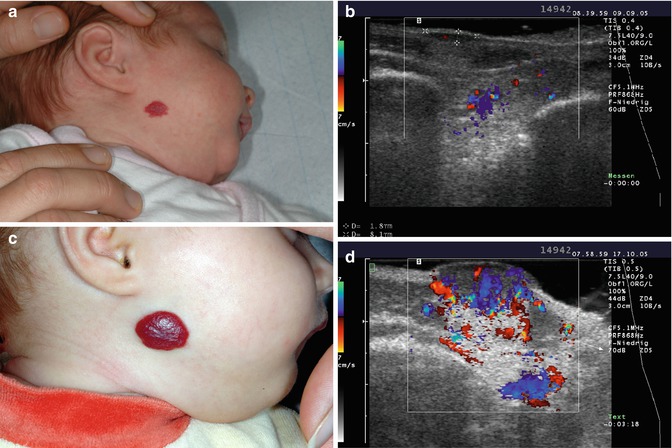
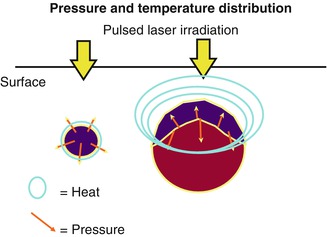
Fig. 13.2
(a) Hemangioma assumed to be only superficial. (b) In CCDS hyposonic swelling of the skin, notice the faint hypersonic modification of the subcutaneous region with some small color-coded vessels: indication of deeper infiltration. (c) Rapid growth despite FPDL laser therapy. (d) Now CCDS shows the preexisting subcutaneous infiltration more clearly
Table 13.1
Vessel size limits the effect of the flashlamp-pumped pulsed dye laser
Frequency-Doubled Nd:YAG Laser (“KTP”)
This type of laser must not be mixed up with the pulsed Nd:YAG laser or even with the continuous wave Nd:YAG laser [6]. Here, the infrared light of the Nd:YAG laser passes through a potassium titanyl phosphate crystal, which produces from the near infrared (NIR) of 1,064 nm by frequency doubling half the wavelength of 532 nm. Thus the biological effect is comparable to that of an argon laser [4]. The advantage of this type of laser is that the KTP due to its better efficacy, especially when pumped with diodes, does not need water cooling unlike the argon laser. This makes it easier to handle.
Due to the experience with other telangiectases, such as angioma serpiginosum, small tuberous hemangiomas and residual telangiectasias after regression are being directly treated under glass spatula compression dot to dot (Fig. 13.3a, b). By short pulse durations of a maximum of 100 ms and avoidance of double exposure or overlapping, absorption only takes place in the hemoglobin of the vessels, so that no thermal side effects are to be expected in the surrounding tissue.
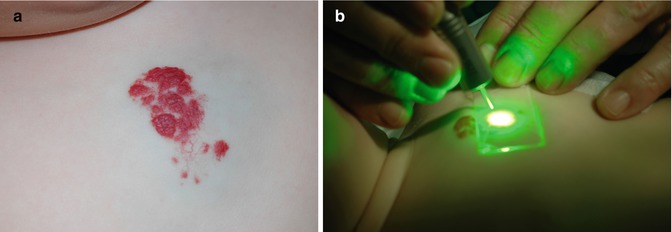
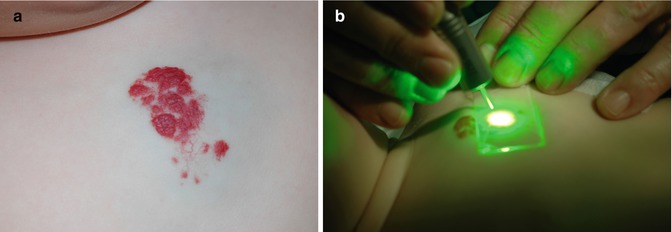
Fig. 13.3
(a) The cutaneous part of this combined hemangioma shows vascular ectasias and tuberous infiltrations. (b) KTP treatment under quartz glass compression
Pulsed Nd:YAG Laser
Unlike the KTP laser, NIR radiation is applied directly. The difference to the standard cw-Nd:YAG laser is its short pulse rate of 2–10 ms, albeit with high pulse peaks. While the biophysical penetration is the same as that of the cw-Nd:YAG laser, the actual penetration depth is limited due to the short pulse duration (Fig. 13.4a–c). For this reason, this laser is suited in anatomically endangered regions or larger vein ectasias and tuberous lesions [7]. To avoid secondary damage by scattered radiation or heat conduction, at least one intermittent cooling system by cold air or ice cubes is required, unless the beam is led through the fluid cooling cuvette or the ice cube as with the cw-Nd:YAG laser.


Fig. 13.4
(a) Markedly elevated cutaneous infiltration in the sensitive anogenital region. (b) Circumscribed spotted superficial coagulations after pulsed Nd:YAG laser exposition. (c) Only minor hemangioma residuals after healing without any scar
Continuous Wave (cw-Nd:YAG) Lasers
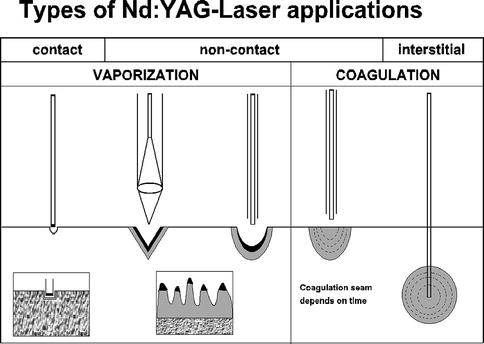
With longer exposure times than 100 ms, thermal conductivity by the laser-heated tissue is the main effect. This means that for the primary reaction, a specific absorption is important, but the whole tissue interaction is also triggered by the exposure time (Table 13.2). Lasers with high water absorption like erbium or CO2 lasers have in all tissue the same primary effect; the real tissue interaction depends only on the exposure time. Besides argon laser, the cw-Nd:YAG laser is the laser type that has been used for the longest time in the treatment of congenital vascular anomalies. It is the same laser which is used for endoscopic surgery. In addition to the possibility of directing the laser beam via thin glass fibers, the immense biophysical variability has made this laser the “workhorse” in the treatment of congenital vascular anomalies. The biophysically determined penetration (drop in photon density to 1/e2) is 8 mm for most tissues. But this means that with continuous wave mode at high performance, an effective photon density can still be attained in depths of 20 and 30 mm. On the other hand, the photon density and thus the effective depth can be limited to less than 1–4 mm by short pulse durations. Suitable cooling procedures protect the penetrated surface enough despite surface absorption to allow no tissue reactions there but only deeper down. Moreover, different absorption coefficients are responsible for the selective effect. Blood and organs rich in blood absorb this near-infrared radiation considerably better than connective or fatty tissue. The tissue reaction to NIR also differs from tissue to tissue. Collagen shows considerable shrinkage and the endothelium already reacts with a serious vasculitis to power densities which do not yet trigger a reaction in other tissue. High power densities quickly lead to carbonization, which then fully absorbs the following laser radiation. Thus, vaporization sets in with two consequences: if one wants to ablate or cut, this process must occur very quickly to avoid unwanted thermal effects in the vicinity. If coagulation is intended especially in the deep regions, this process must be avoided, as no radiation gets deep down enough. The direction of these processes determines the wide usage of cw-Nd:YAG laser [8].
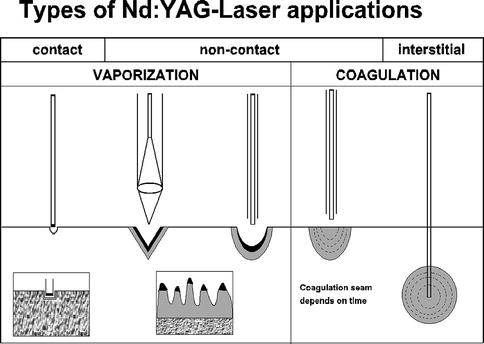
Table 13.2
Principle application modes of the cw-Nd:YAG laser
Transcutaneous Direct Application
In the same way such in the case of patients with Osler syndrome, small tuberous lesions and telangiectasias may also be treated with cw-Nd:YAG laser analogous to pulsed Nd:YAG laser and KTP laser. To avoid thermal damage, short pulse rates of a maximum of 100 ms, an output of 25 W, and a small spot diameter of up to 0.5 mm are required by using a focusing handpiece. Besides, intermittent and post cooling with ice cubes have to take place to avoid thermal damage by heat blockage.
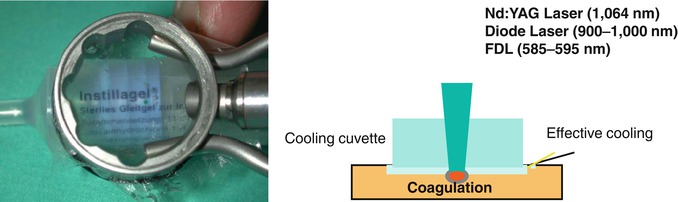
Transcutaneous Application with Fluid Cooling Cuvette
If intermittent cooling is not sufficient, continuous cooling is required. The heat capacity of spray or cold air cooling is not sufficient for the heat blockage caused by the cw-Nd: YAG laser. Various contact cooling systems are on the market or are offered. Cooled sapphire plates are easy to handle but have a series of disadvantages. The metal frame of the cooling Peltier element may lead to frostbite in case of direct skin contact. The biggest disadvantage, however, is that their plane surface cannot adapt to the anatomic situation, especially in children’s faces, so they either do not have full contact to the surface or are too heavily compressed at the edges, causing not only frostbite but also change in the microcirculation. Thus, they can actually be used only for large plane areas. The fluid cooling cuvette with a 40 % refrigerated glycol solution has a (side of the patient) highly flexible, highly transparent latex membrane which, through changes in the outlet valve, can adapt even to difficult anatomic silhouettes (Table 13.3). An additional advantage is that this prestressing makes it possible to adjust the compression pressure and the blood flow to vary tissue absorption [9]. With maximum compression, the overlying tissue can be made transparent for the Nd:YAG laser radiation. With negative pressure (suction), the tiniest capillary vessels can be expanded, boosting specific absorption. The cooling capacity has been calculated to have a reaction in the center of the laser beam given the necessary absorption while adverse events by scattering and thermal conduction are avoided in the surrounding areas. In case of vein ectasias, this procedure is better suited than the KTP.
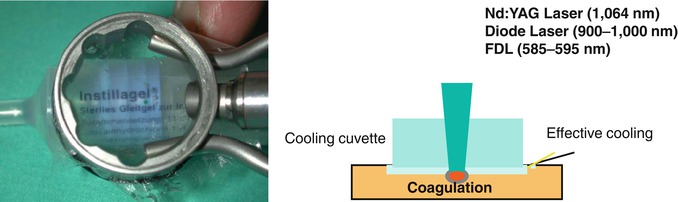
Table 13.3
Cooling chamber, principle of the fluid cooling cuvette
Transcutaneous Application with Continuous Ice Cube Cooling
If subcutaneous lesions are to be treated transcutaneously, a continuous Nd:YAG laser application would create so much heat that none of the abovementioned cooling systems would be able to completely protect the transient tissue from unwanted coagulation [10]. Deep freezing systems such as liquid nitrogen or deep temperature Peltier elements cannot be directed sufficiently, so frostbite would result. Here, radiation through a transparent, ice cube without air bubbles seems to be the solution. The melting of ice to water is one of the most energy-consuming processes. This high heat capacity is capable of completely rerouting the heat that builds up in the transient tissue by basic absorption, so there are no reactions on the surface. On the other hand, natural law prevents the temperature from dropping below 0 °C, avoiding frostbite. Since meltwater always guarantees good tissue contact, contact gels moreover are superfluous. This cooling effect is limited to 2 mm due to the thermal conductivity properties of the tissue, so that laser radiation can treat subcutaneous lesions thanks to its greater penetration, without causing any defects on the surface. Prerequisites are the use of a focusing handpiece with a focus diameter of 0.5–1 mm. This focus has to be positioned to the tissue surface through an ice cube, as otherwise no sufficient penetration will be attained because of diffraction scattering. As the ice cube has its own absorption for this laser radiation, a prolonged exposition would drill a hole into the ice cube (“chimney effect”), letting radiation get directly to the tissue surface. Therefore, the 6 ice cube has to be moved above the hemangioma under laser exposition, the ray itself moving in small spiral motions with a radius of about 5 mm to avoid too high a load for a single spot. If only the laser beam would be moved above the ice cube, but not the ice cube as well, the chimney effect could be avoided, but the developing heat on the surface of the hemangioma would melt the ice cube so much that there would be no more direct tissue contact between the ice cube and hemangioma (“igloo effect”). By compression especially in large hemangiomas with the ice cube, the depth of penetration can be increased, and by pressure on the surface, the absorption decreased, boosting the protection (Table 13.4). This procedure is only recommended under anesthesia because of the associated pain. Besides, this is also necessary because of laser safety, because most hemangiomas are located in the face near the eyes. For the exact positioning of the laser parameters, an intraoperative CCDS is required, as this alone enables determination of activity and exact stage, dimension, and where applicable involvement of various layers (Fig. 13.5a–d). To choose the laser output, the following rules apply: The more active and aggressive the growth and the earlier the stage, the smaller the output to avoid an overreaction. The more vessels are visible already, the higher the output to attain involution. Moreover, the stronger the intracutaneous lesion, the smaller the output, but in exclusive subcutaneous lesions, more output. However, in exclusive subcutaneous lesions, the output is higher. Treatment next to the eyes necessitates protection from forward-scattered radiation. For this purpose, metal spatulas (“eye spatulas”) are suited that float on a kanamycin-ointment bed in such a way that the backside never touches the cornea. For this reason, the laser beam should always be turned away from the eyeball. At the columella, attention should be paid to the cartilage structure of the nose. In case of hemangiomas on the lips, the laser also has to be turned away from the gingiva to avoid destruction of the dental germ. A hemangioma of the gingiva itself can then be treated with the FPDL laser. The aim is not a definite coagulation of the infantile hemangioma but the induction of a vasculitis. A visible blanching or even an involution during laser treatment should be avoided as this would be equivalent to overdosing. The optimal total dose has been reached when the hemangioma during laser treatment starts to show a swelling and is bulging and the surrounding area turns red, which lasts up to 12 h. Occasionally, 6–24 h postoperatively, subcutaneous blue indurations develop as an expression of the vasculitis with a vessel breakdown. This reaction is common in very active infantile hemangiomas in the early proliferation phase. As the overlaying epidermis is easily damaged, postoperatively, enough ointment should be applied, and the area should be protected against scratches with suitable measures such as the wearing of gloves. A bandage is rarely necessary, except in case of heavy mechanical abrasions. Although this treatment does not cause injuries on the surface of the skin, about 2 % of the children, 12–48 h after the operation, develop erysipelas with a beginning lymphangitis (Fig. 13.6a, b). This is seen frequently in the face. Erysipelas does not develop in the hemangioma itself or around it, but occasionally a few centimeters away draining into the lymph. This inflammation can be differentiated from the direct postoperatively laser-induced inflammation as this region is sensitive to touch and hardened. In already exulcerated or even secondarily infected hemangiomas, this reaction has never been noted, nor in interstitial treatment when puncturing. It thus is not a nosocomial infection. An immediate treatment with oral antibiotics with a broad-spectrum cephalosporin will cause the clinical symptoms to subside within a few hours. Fever and symptoms do not exist at any time then, but the infiltrate may persist for a few days.
Table 13.4




Transcutaneous Nd:YAG laser treatment with ice cube cooling
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







