Fig. 35.1
Therapeutic algorithm of vascular malformations. Only the simple form of port-wine stain does not need any further diagnostics. In all other cases, the visible part of the vascular malformation may be the tip of the iceberg of underlying affections
Table 35.1
The choice of laser types depends on the depth, the thickness, and the kind of malformation
Superficial cutaneous | |
Flat findings | Flash lamp-pumped dye laser |
Telangiectatic findings | Argon laser, KTP |
Tuberous findings | Pulsed Nd:YAG laser |
Hyperkeratotic findings | CO2 laser |
Intra- and subcutaneous to a depth of 1–15 mm | |
Impression technique with bare fiber | |
Transcutaneous Nd:YAG laser with ice cube cooling | |
Subcutaneous, voluminous up to a depth of 10 mm | |
Nd:YAG laser interstitial or intraluminal | |
Hollow organs, body cavities | |
Nd:YAG laser endoscopic in air/water | |
Capillary Malformations
Port-Wine Stains (PWS)
Capillary vascular malformations are the most frequent and the oldest indication for laser treatment in both children and adults [1].
With the introduction of the flash lamp-pumped pulsed dye laser (FLPDL), PWS can be treated in infancy and early childhood. The high pulse peak power of the pulsed dye laser disrupts the vessels. The energy fluency ranges from 4 to 10 J/cm2 and is varied according to the age of the patient, the anatomic location, and the color of the lesion: 5.0–5.6 J/cm2 in children less than 12 months of age, 5.6–6.4 J/cm2 in children 12 months to 4 years of age, and approximately 7 J/cm2 in children over 4 years of age. Energy is reduced over the eyelids and hands. If blanching or graying of the epidermis occurs during application, energy fluencies should be reduced in order to avoid blistering of the epidermis. Treatments start at the lowest energy density that shows an adequate primary reaction. The lighter the lesion, the higher the energy density for the age range. The darker the lesion, the lower the energy density. Immediately after treatment the area characteristically becomes blue gray and turns purpuric in a few hours with surrounding erythematous flare: this takes 7–14 days to resolve. Some edema, especially in the periorbital area, is possible. As the purpura disappears, the area lightens progressively for up to 6 weeks. After treatment, the treated areas are covered with panthenol ointment. In case of blistering, parents are instructed to cleanse the area with polyvidone-iodine solution, even if a crust has formed. To avoid postoperative irritation of the treated areas, we instruct the parents to keep their children’s fingernails short or that the children wear gloves to avoid trauma to the treated areas. Treatments are usually repeated at 6 week intervals until the desire degree of lightening is achieved.
Adult and teenage patients can often be treated without anesthesia, although this is dependent on the size and anatomic location of the lesion. General anesthesia is necessary for children with extensive lesions or in case of central facial PWS because of the need for eye protection (Fig. 35.2). A significant reduction of pain as well as skin protection during laser treatment can be achieved using a fluid cooling cuvette or cold air. Some authors use cryogen spray cooling. This can lead to patient discomfort, especially near the nose, eye, mouth, or ear.


Fig. 35.2
Treatment of port-wine stains using the flash lamp-pumped pulsed dye laser. LPDL therapy of port-wine stain in early childhood. The earlier the therapy begins, the better the results. Due to intraoperative eye protection in facial lesions, general anesthesia is mandatory. In case of Sturge-Weber syndrome, anesthesia can be used for further clinical investigations such as ophthalmotonometry
The incidence of complete clearing is variable. PWS in dermatome V2 centrofacial regions involving the medial portion of the cheek, upper lip, and nose show less lightening than PWS in other locations. Furthermore, lesions on the hand and arm respond less well than lesions on the face, neck, and torso.
Patients younger than 4 years of age require fewer treatments [2]. Treatment of children at the earliest possible age may prevent considerable psychosocial impairment and result in a more complete response. Early treatment of these lesions is expected to prevent the progression of the vessels in the PWS to more ectatic structures that make the lesions dark purple, raised, and nodular in many adults. It is hoped that hypertrophy of affected areas, a common complication of extensive PWS, and permanent deformity associated with these lesions can be mitigated. The argon- or potassium-titanyl-phosphate (KTP) laser (power 2 W, pulse duration 0.1 s, interval 0.1 s, spot size 0.05–1 mm) is useful for telangiectatic PWS and dark purple and nodular PWS of adults, with a good response and a low risk of scarring.
Capillary-Lymphatic Malformation
Capillary-lymphatic malformations may be discriminated from the classical PWS by light staining and can be bluish red to black in color. Due to the lower erythrocyte concentration, the basic absorption for the FLPDL is reduced so the results of dye laser therapy are generally worse than for PWS. However, the ectatic venules in the epidermis are a good indication for the KTP, pulsed Nd:YAG, or chopped CW Nd:YAG with fluid cooling cuvette (Fig. 35.3). However, in these lesions the birthmark is only the tip of the iceberg. In nearly all cases, there is a mixed venous-lymphatic malformation in the underlying organs. Capillary-lymphatic malformations are observed either in association with Klippel-Trenaunay syndrome or alone. So the general anesthesia needed for the laser therapy in childhood may also be used for clinical examinations if necessary.
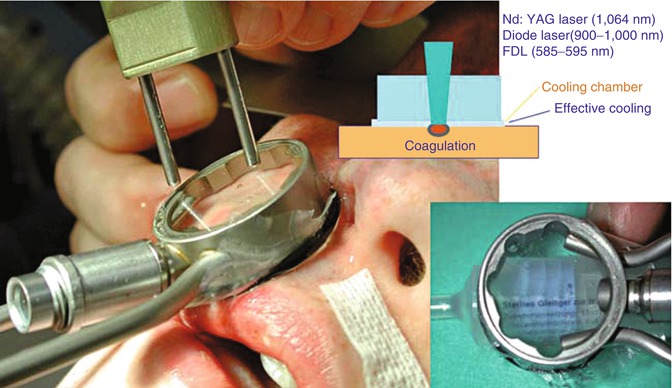
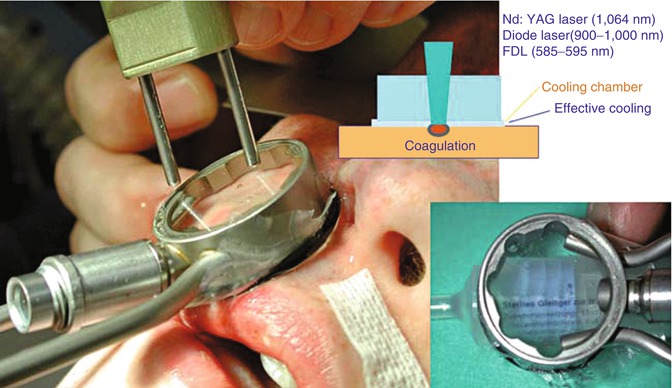
Fig. 35.3
Cooling chamber. The flexible membrane on the patient side of the fluid cooling cuvette can follow all anatomical contours. This allows complete protection of the skin even in difficult regions
Hyperkeratotic Capillary Malformation
Angiokeratomas are usually known by their eponyms, matched with the predilection of the lesions: Mibelli for lesions on the hands or feet, Fordyce for lesions on the scrotum, and Fabry for lesions on the trunk or thighs. If only the lymphatic capillaries are affected, this is known as “lymphangioma circumscriptum” [3], but the subcutis may also be affected. Often these lesions bleed easily and weep, either spontaneously or following trauma. Another risk is the high rate of spontaneous erysipelas. The complications provide the indication for laser therapy. KTP laser is mostly not useful due to the high surface absorption. In punctual lesions a pulsed Nd:YAG laser coagulation is helpful, but the popcorn effect due to high energy should be avoided because this can cause bleeding. In disseminated excessive bleeding areas, a homogeneous CW Nd:YAG laser coagulation through ultrasound jelly is necessary to avoid carbonization. However, this is followed by scarring. In more hyperkeratotic lesions CO2-laser vaporization is possible, but even this results in scarring (Fig. 35.4).


Fig. 35.4
CO2-laser vaporization. In hyperkeratinization of mixed vascular malformation with the CO2 laser, a bloodless ablation is possible. Due to depth of the disease, scar-free healing is not possible
Port-Wine Stains with Associated Vascular Malformations (Neurocutaneous Syndromes or Phakomatoses)
Capillary or dermal vascular malformations are occasionally associated with deeper vascular anomalies. The key point is that these cutaneous signs permit early diagnosis, thus helping in further recognition of more complex syndromes. Sturge-Weber syndrome is the most well-known vascular malformation complex associated with port-wine staining. The same malformation affects the soft tissue of the face with the risk of subsequent hypertrophy. This can be detected early by color-coded duplex sonography (CCDS) and especially by thermography with hyperthermy. If this is shown despite the FLPDL therapy, the growing tissue will be treated in cases of dermal hypertrophy with a double pulsed Nd:YAG/pulsed dye laser or in cases of more subcutaneous or soft tissue hypertrophy with the transcutaneous ice cube-cooled Nd:YAG laser, as for infantile hemangioma but with a higher power of 60 W.
The large PWS of the extremities in Klippel-Trenaunay syndrome sometimes need the same combination of pulsed dye laser, transcutaneous ice cube-cooled Nd:YAG laser, or, in cases with hyperkeratinization, CO2 laser. In Proteus syndrome with patchy PWS of the hands or feet, the effectiveness of pulsed dye laser therapy is limited, just as it is for other mixed capillary-lymphatic malformations. However, even here the treatment of ectatic vessels with pulsed Nd:YAG or KTP laser is possible.
In Wyburn-Mason syndrome/Bonnet-Dechaume-Blanc syndrome, the facial PWS may be the sign of unilateral arteriovenous malformation of the retina and the intracranial optic pathway (Fig. 35.5). This means that before FLPD laser starts, embolization of the feeding artery is helpful [4].
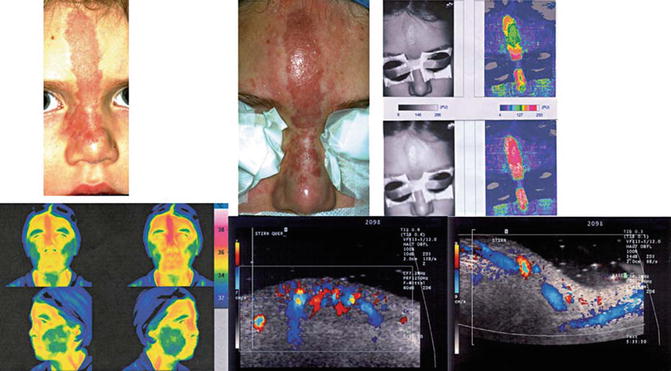
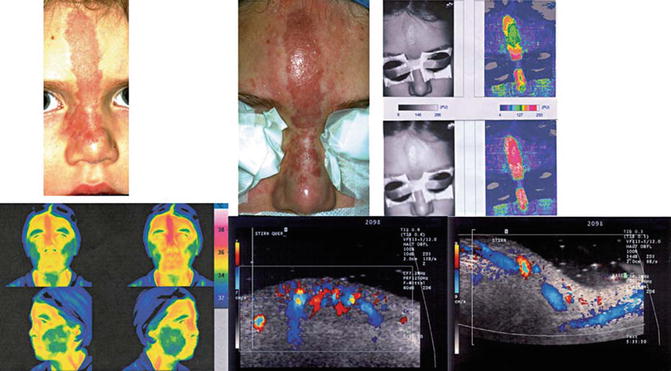
Fig. 35.5
Arteriovenous malformation. Centrofacial port-wine stains may be only an overlying symptom of a deep vascular malformation. As a screening method, thermography is an important investigation. The simple PWS show normotemperature, whereas a hyperthermia is a sign of an AV malformation. In this case no embolization was possible, so transcutaneous Nd:YAG laser therapy with ice cube cooling was started to occlude the microfistulas. The result is seen in the CCDS investigation with a decrease in perfusion
Nonfading Telangiectasias
Nonfading telangiectasias have been subcategorized under capillary malformations. These present in a spectrum, from the classical spider nevus to the maculopapular punctate anomalies of Osler-Rendu-Weber syndrome to the characteristic reticulated marbling and cutaneous hypoplasia seen in cutis marmorata telangiectatica congenita (CMTC).
Cutis Marmorata Telangiectatica Congenita (Van Lohuizen Syndrome)
The characteristic lesion of CMTC has a distinctive deep purple color and is depressed in a serpiginous reticulated pattern. In some cases of CMTC-associated deep venous anomalies, ulceration of the reticulated purple areas and hypotrophy of the involved limb and subcutaneous tissue have been reported. The skin atrophy and deep vascular staining can persist into adulthood, along with diffuse ectasia of the veins in the involved extremities. If the steal effect of these pathological vessels causes skin atrophy, coagulation can enhance the microcirculation to avoid further trophic defects. Spider vascular lesions can be obliterated by KTP laser directed at the central artery under compression.
Osler-Rendu-Weber Syndrome (Hereditary Hemorrhagic Telangiectasia)
This disease is classified with the extratruncular capillary malformations and can appear as telangiectasias in the skin and AV malformations widely distributed throughout the body with a predilection for the gums, lips, mucosa of the nose, face, and fingers [5].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







