Step 1
Surgical Anatomy
- ♦
The adrenal glands lie partially anterior, superior, and medial to the renal upper poles. The caudal limb of the left adrenal lies in close proximity to the left renal hilum ( Figs. 11-1 and 11-2 ).

Figure 11-1
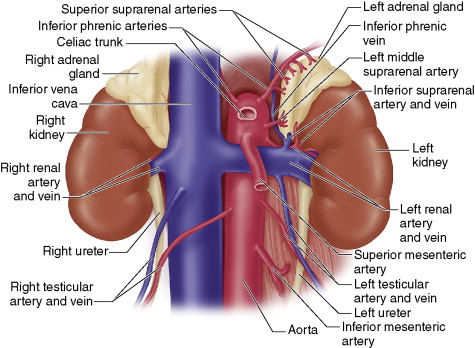
Figure 11-2
- ♦
The left adrenal vein often joins with the medially located inferior phrenic vein to form a common channel entering the left renal vein.
- ♦
The right adrenal vein is short and empties directly into the posterolateral aspect of the inferior vena cava. Occasionally, additional veins may drain into the inferior vena cava or right hepatic vein.
- ♦
Arterial inflow to the adrenals is less predictable but generally arises as small arteries originating from the renal artery (inferior suprarenal artery), the aorta (middle suprarenal artery), and the inferior phrenic artery (superior suprarenal artery). Paired small veins may accompany these arteries.
- ♦
Rarely, small rests of adrenocortical tissue may be found at sites near the adrenal bed or at a distance (e.g., ovaries). This has particular importance when treating corticotropin-dependent hyperadrenocorticism.
Step 2
Preoperative Considerations
- ♦
Lateral laparoscopic adrenalectomy is indicated in the following circumstances:
- ▴
All benign, functioning adrenal masses less than 6 cm in maximal diameter (aldosteronomas, cortisol-secreting tumors) and pheochromocytomas less than 8 cm in diameter
- ▴
All nonfunctioning adrenocortical tumors greater than 4 cm but less than 6 cm in diameter
- ▴
All nonfunctioning tumors less than 6 cm in diameter demonstrating interval growth by cross-sectional imaging (i.e., computed tomography [CT], magnetic resonance imaging [MRI]).
- ▴
All tumors, regardless of size, with a worrisome radiographic phenotype (i.e., high Hounsfield units on noncontrast CT, poor washout of intravenous contrast on CT, bright image on T2-weighted MRI).
- ▴
- ♦
The lateral laparoscopic approach is contraindicated in the following conditions:
- ▴
Obvious, large, adrenocortical carcinoma
- ▴
Pheochromocytoma greater than 8 cm or clearly malignant pheochromocytomas (i.e., invasion, nodal metastases)
- ▴
Extensive upper abdominal surgery in the past. In this instance, the surgeon should consider a posterior endoscopic approach.
- ▴
Preoperative Preparation
- ♦
For pheochromocytomas, pharmacologic blockade (α-blockade for 7 to 10 days, then β-blockade for 24 to 48 hours preoperatively for atrial tachyarrhythmias; and calcium channel blockers) is instituted. Effective circulating volume is restored using salt-loading and increased fluid intake.
- ♦
When treating aldosteronomas, optimal blood pressure control must be achieved and hypokalemia should be corrected. Mineralocorticoid receptor blockade is instituted.
- ♦
The patient with Cushing’s syndrome undergoes perioperative steroid preparation, as well as prophylaxis for deep venous thrombosis, stress ulcer, and opportunistic infection prophylaxis.
Surgical Equipment
- ♦
The equipment typically used to perform a lateral laparoscopic adrenalectomy includes the following:
- ▴
Four 10-mm trocars
- ▴
Endopath Xcel port (Ethicon Endo-Surgery, Cincinnati, OH)
- ▴
10-mm scopes, both straight and 30-degree
- ▴
Insufflator, light source, and camera
- ▴
Two monitors, InsideView (LSI Solutions, Victor, NY) optional
- ▴
5-mm harmonic scalpel
- ▴
L-cautery tip
- ▴
10-mm clip applier
- ▴
Suction/irrigation apparatus.
- ▴
Step 3
Operative Steps
Anesthetic Induction
- ♦
General endotracheal anesthesia is performed.
- ♦
A radial arterial line and one to two large-bore peripheral intravenous lines are introduced.
- ♦
A central line should be introduced in elderly, infirm, and select pheochromocytoma patients.
- ♦
Antibiotics and deep venous thrombosis prophylaxis should be administered.
- ♦
Nitroprusside (Nitropress), labetalol (Trandate), nicardipine (Cardene), and intravenous pressors should be readily available for pheochromocytoma patients.
- ♦
An orogastric tube is put in place.
Positioning and Port Placement
- ♦
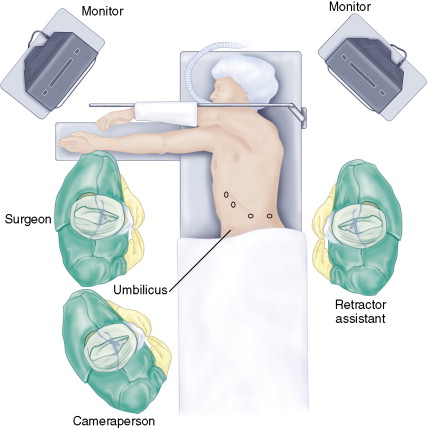
The patient is placed in (near-complete) lateral decubitus position with the side of the tumor facing up ( Fig. 11-3 ).