Invasive Mediastinal Staging Overview
CRITICAL ELEMENTS
Confirmation of Imaging Findings
Mediastinal Staging for Central Tumors
Mediastinal Staging Prior to Treatment
Mediastinal Staging at the Time of Lung Resection
1. MEDIASTINAL STAGING FOR PATIENTS WITH SUSPECTED MEDIASTINAL NODAL INVOLVEMENT ON IMAGING
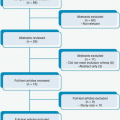
Recommendation: In general, for patients with known or suspected non-small cell lung cancer (NSCLC) who are potential surgical candidates, any positron emission tomography (PET) or computed tomography (CT) findings that suggest mediastinal nodal involvement should be confirmed with invasive mediastinal staging.
Type of Data: Retrospective.
Strength of Recommendation: Strong.
Rationale
Although PET and CT are critical components of the noninvasive clinical staging of NSCLC, both have surprisingly high false positive and false negative rates. Certain clinical presentations (e.g., granulomatous disease) can confound the interpretation of these imaging studies, which could result in inappropriate clinical stage assignment and improper care. Thus, guidelines for performing invasive staging of the mediastinum for NSCLC have been devised. More precise pretreatment staging should improve the care and survival of NSCLC patients.
Most guidelines for invasive mediastinal staging incorporate radiographic staging results, clinical T status, tumor location (central or peripheral), and available institutional technical expertise. Moreover, if PET or CT findings suggest the presence of disease in the hilum but not the mediastinum, invasive mediastinal staging is also recommended because of a substantial incidence of false negative radiographic mediastinal staging in such patients. If PET and CT results are discordant, invasive staging should be performed.
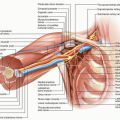
Invasive mediastinal staging techniques include cervical mediastinoscopy, endobronchial ultrasonography (EBUS), endoscopic ultrasonography (EUS), video-assisted thoracic surgery (VATS), and possibly transcervical extended mediastinal lymphadenectomy. The goal of these strategies is to accurately establish the pathologic disease stage to avoid unnecessary lung resection in patients with advanced disease and offer life-extending operations to patients whose clinical disease stage would otherwise be erroneously thought to be advanced because of false positive imaging results.
The negative predictive value of CT alone for mediastinal staging is 70% to 95% and that of PET alone is 80% to 99%. The combination of these two modalities has a negative predictive value of about 95%, indicating that in the absence of other indications, mediastinal staging is not necessary if both PET and CT reveal the mediastinal nodes to be normal.1 CT or PET findings suggestive of abnormal mediastinal nodes in areas in which fungal or other granulomatous diseases are endemic creates challenges to accurate clinical decision making. Certainly, these findings may not represent tumor involvement of the nodes, and the imperative to document pathologic nodal status is even stronger in these instances.
2. MEDIASTINAL STAGING FOR CENTRAL TUMORS, CLINICAL N1 DISEASE, AND LARGER TUMORS IN THE ABSENCE OF MEDIASTINAL NODAL ABNORMALITIES ON COMPUTED TOMOGRAPHY AND POSITRON EMISSION TOMOGRAPHY
Recommendation: Patients with central tumors, regardless of T status or PET or CT findings, and patients with T2 or greater disease should undergo invasive mediastinal staging.
Type of Data: Retrospective.
Strength of Recommendation: Weak.
Rationale
For patients for whom PET and CT findings are negative for mediastinal and hilar (and systemic) disease, the use of invasive lymph node staging is predicated on the T status, the location of the primary lesion, and the characteristics of ipsilateral hilar nodes on clinical staging. Patients with clinical T1a/T1b peripheral lesions (stage IA disease) and no evidence for hilar or mediastinal adenopathy on PET and CT do not require additional mediastinal staging.2 However, patients with T2 or greater primary
tumors, clinical evidence of hilar nodal involvement, or central tumors should undergo invasive mediastinal staging, even if their PET and CT findings are negative for disease in the mediastinum.3
tumors, clinical evidence of hilar nodal involvement, or central tumors should undergo invasive mediastinal staging, even if their PET and CT findings are negative for disease in the mediastinum.3
There are some cogent arguments for offering invasive mediastinal staging to patients with negative PET and CT findings in the mediastinum who present with synchronous small lesions (T1a/T1b), regardless of whether these lesions are in the same lobe, in the same lung, or in opposite lungs. Also, patients for whom stereotactic body radiosurgery is planned should be subject to the same criteria as operative candidates. Local therapy with stereotactic radiosurgery may be of little value in the setting of nodal disease.
3. MEDIASTINAL STAGING PRIOR TO LUNG RESECTION
Recommendation: Proper mediastinal node staging requires a thorough understanding of the limitations of mediastinoscopy, EUS, EBUS, and VATS.
Type of Data: Retrospective.
Strength of Recommendation: Weak.
Rationale
The appropriate extent of mediastinal staging to some degree depends on the minimally invasive technique that is used, as this determines the accessibility of the nodes.1 For traditional staging mediastinoscopy, sampled nodes should routinely include R4, L4, and 7 nodes. More stringent recommendations require that R2 and L2 specimens be obtained for all patients.
The different staging techniques afford variable access to the different lymph node stations. EBUS techniques have good lymph node yield when the nodes are enlarged and can access many level 10 and some level 11 nodes. EUS, on the other hand, offers access that is typically limited to level 7, 8, and 9 nodes. Thus, EUS can be used to diagnose the presence of mediastinal nodal involvement but is insufficient as a single staging modality to map the mediastinum. VATS typically permits access to only level 7 and ipsilateral nodes and so is useful for accessing nodes specifically targeted by PET or CT and for completing the staging of stations 5, 6, 8, and 9 when indicated. Cervical mediastinoscopy has been long held to be the gold standard of mediastinal lymph node staging and provides access to stations 2, 4, and 7 but not 5, 6, 8, or 9 nodal stations.
The first invasive modality performed for mediastinal staging should be bronchoscopic staging with EBUS, as it has a satisfactory lymph node yield, costs less, and has a lower complication risk than mediastinoscopy or VATS does.4,5 If abnormal inferior mediastinal adenopathy is present, EUS may be performed initially or instead of EBUS6 if institutional expertise is present. If it is not, mediastinoscopy should be performed first. The negative predictive value of mediastinoscopy is more than 90%, and the incidence of nodal involvement detected using the modality approaches 40%
overall. However, this latter value heavily depends on the indications for mediastinoscopy.7 For example, in patients with clinical stage I disease, the incidence of nodal involvement detected by mediastinoscopy is only 3% and that detected by thoracotomy is only 5.6%.2
overall. However, this latter value heavily depends on the indications for mediastinoscopy.7 For example, in patients with clinical stage I disease, the incidence of nodal involvement detected by mediastinoscopy is only 3% and that detected by thoracotomy is only 5.6%.2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree