The CSF compartments and the adjacent CNS ECF constitute a regional cavity for the purposes of drug administration. This cavity is not closed, and a drug administered into the CSF can leave through
Aside from biotransformation rates, which vary depending on the structure of the drug, the clearance of drugs from the CSF will be somewhat predictable, based on molecular size and partitioning into lipid (e.g., octanol/water partition coefficient).
Figure 8.1 shows the observed relationship for
Kout versus log(octanol/water partition coefficient)
Mr-1/2 as described by Levin and Landahl.
36Figure 8.2 shows the hypothetical relation between drug half-life (a term that in this context includes biotransformation and the loss of drug from the ECF to the blood through permeation across capillaries), diffusion coefficient in cm
2 per second, and the distance into brain parenchyma that 10% of the CSF drug level will permeate. This bar graph was computed assuming diffusion from a planar surface.
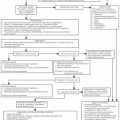
A number of therapeutic points emerge for consideration. Drugs administered intrathecally (spinal subarachnoid) will not reflux into the ventricular system unless a reversal of the normal hydrostatic gradient or hydrokinetic flow has occurred. Reversal of the hydrokinetic flow is observed in the hydrocephalus. This is important because it means that the IT route is inferior when the drug is required to reach the choroid plexuses or the intraventricular ependymal surface. Other reasons to avoid the IT route include
inadvertent drug injection into the subdural space instead of the CSF and the risk of local damage to the spinal cord or nerve roots because of high concentrations of drug at the injection site. Intraventricular drug administration with gentle barbotage four to six times quickly dilutes the drug in a large ventricular fluid volume and enhances drug egress from the ventricles to a half-time in the order of minutes,
36 although for most relatively small molecules such as those that are currently used, transit from the ventricles is quite rapid.
Diffusion
Because drug diffusion into brain parenchyma is slow relative to its clearance from the CSF, the depth of effective drug concentration is small, and a therapeutic benefit for a deep parenchymal lesion, and by extrapolation, a nodular lesion on the meningeal surface, is unlikely (
Fig. 8.2). Further compromising drug delivery to a nodular tumor in the CSF pathway is the fact that when drug diffuses into a nodular lesion, as soon as it comes into contact with a tumor capillary, it crosses into the systemic circulation and reduces the potential tumor drug level. Pharmacokinetic calculations suggest that nodules greater than 5 mm in diameter are inadequately treated by regional therapies.
41,42 Administration of drug into the CSF often fails because the drug does not make contact with tumor cells long enough to kill them. This is because
the tumor obliterates the subarachnoid space and the drug cannot reach many of the cells;
the tumor is nodular and only the most superficial cells make contact with the drug; and
the drug is too unstable or is small and nonionized, being cleared from the CSF before reaching distal sites in the CSF pathway.
Sometimes these shortcomings can only be overcome by increasing the administered dose at the risk of CNS toxicity or by providing a carrier, such as a monoclonal antibody, to slow the CSF clearance of the drug and to increase its targeting to tumor cells. To fully evaluate the potential of this last approach, further experimental study is required to ascertain optimal conditions for carrier-drug targeting.
Regional Delivery
Regional delivery of chemotherapeutic agents to the CNS had its earliest use in the treatment for infectious meningitis. Antibiotics were injected through a spinal needle through frontal burr holes into the frontal lobes and ventricles. In an effort to diminish the morbidity associated with this form of therapy, Ayub Ommaya developed an implantable closed delivery system while working at the National Institutes of Health.
43 Using this system, the ease with which therapeutic agents could circumvent the BBB opened new strategies for the treatment of CNS infections and malignancies. Although great advances have been made since the introduction of the indwelling closed ventricular delivery system, major problems still face clinicians who utilize these systems.
Refinements, such as valves and shunt attachments, have permitted greater flexibility in the use of reservoirs. Lumbar reservoirs have been used more frequently for the delivery of analgesics than for chemotherapy. Although some studies have reported good results in using lumbar reservoirs,
44 their high rate of malfunction
45 and the better distribution of drug when delivered into a ventricle
46 have made the intraventricular route favored for chemotherapy for CNS malignancy.
Following percutaneous lumbar administration of methotrexate (MTX), the drug at times fails to reach the head and leaks into the epidural or subdural space; this complication is more likely after repeated lumbar administration.
47 Even with successful lumbar administration, the intraventricular levels of MTX are highly variable, as indicated by a study measuring drug concentrations at both levels
46 (
Fig. 8.3A). In that study, serum MTX levels were approximately 1 × 10
-3 those achieved in the CSF (
Fig. 8.3B). More recent data suggest that, with respect to progression-free survival, intraventricular administration may be more important for agents with short, as compared with long, half-lives.
48Given the cell cycle-specific action of MTX, administering that drug by a pulse technique may limit its effectiveness while increasing the chances of neurotoxicity, as toxicity seems to correlate with peak levels. One randomized study of children with leptomeningeal acute lymphocytic leukemia (ALL) compared standard 12 mg per m
2 therapy twice weekly with concentration time therapy.
49 By ventricular reservoir, 1 mg of MTX was administered every 12 hours for 6 doses. The dosage
was adjusted to achieve an MTX level of 5 ± 2 × 10
-7 in the lumbar spinal fluid before administration of the next dose of MTX. This course was repeated every 7 to 10 days until remission occurred. As with standard pulse therapy, the course was repeated during the consolidation and maintenance periods. Less neurotoxicity was seen in patients who received the “concentration × time” therapy than in those who received the standard pulse therapy, with no difference in efficacy between the two approaches.
Intraventricular catheters are relatively safe. The most important complications include catheter malposition or obstruction (3.8% to 6.6%)
45,50 or reservoir exposure (1.6%),
50 and catheter-related infections (3.8% to 7.5%).
45,50 Most infections are controllable with antibiotics. Infected reservoirs can be successfully managed with antibiotic therapy without removal of the hardware,
51 although in some cases, reservoir removal is required just as it is in other foreign body infections. Skin bacteria are the most frequent cause of infection, but scrupulous attention to technique will lessen the incidence of this complication.
51 An additional benefit of the reservoirs is the avoidance of repeated lumbar punctures that are painful and inconvenient.
Whether the intralumbar or intraventricular reservoir administration route is used, it is critical to establish the patency of the CSF pathways, as blockages are common in leptomeningeal malignancy. Local compromise of CSF flow may leave some areas untouched by the administered therapeutic agents and may increase local toxicity if CSF circulation is impaired. Radionuclide imaging with
111indium-albumin accurately assesses spinal fluid flow. Focal radiation therapy can often ease areas of blockage once they have been identified. Focal CSF blocks that are unrelieved by radiotherapy portend a worse prognosis.
52,53