Intraperitoneal Chemotherapy
Maurie Markman
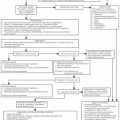
The intraperitoneal administration of chemotherapeutic agents has evolved since the 1980s from a pharmacokinetic concept to a procedure that should be considered for use by physicians in routine clinical practice.1 This chapter reviews the basic principles supporting the intraperitoneal delivery of antineoplastic agents, practical issues raised by the use of this technique, and results of clinical trials examining this unique therapeutic strategy.
PRINCIPLES OF INTRAPERITONEAL CHEMOTHERAPY
The fundamental goal of the intraperitoneal administration of antineoplastic agents is to expose tumor present within the abdominal cavity to higher concentrations of drug for longer periods than can safely be accomplished following systemic drug delivery.1,2 Increased exposure is measured by demonstrating both higher peak levels and area under the concentration-time curve in the cavity after intraperitoneal delivery, compared with those observed in the systemic circulation. Extensive preclinical evaluation has defined a number of characteristics considered important in optimizing any advantage associated with intraperitoneal drug delivery (Table 9-1).
An important consideration in selecting drugs for intraperitoneal therapy of a previously treated tumor (e.g., small-volume residual ovarian carcinoma after systemically delivered cisplatin or carboplatin) is whether there is evidence of absolute, or only relative, resistance of the tumor to the agents in question. If the resistance that develops in tumors exposed to concentrations of drug achieved with systemic drug delivery can be overcome by exposing the tumor to the higher concentrations of the agent attainable after intraperitoneal delivery, there is a strong rationale for using the same drug(s) administered by the intraperitoneal route after a major (but incomplete) response to the agent delivered intravenously.
This is the principal justification for the use of intraperitoneal cisplatin-based therapy in small-volume residual ovarian carcinoma after systemic treatment with either cisplatin or carboplatin-based chemotherapy.1 Preclinical evaluation has demonstrated that, in experimental systems, cisplatin resistance can be overcome by exposing tumor cells to 2- to 5-fold higher concentrations of the agent.3
Therefore, the 10- to 20-fold increased exposure of the peritoneal cavity to cisplatin achievable after regional delivery might be predicted to result in additional clinically relevant cytotoxicity in patients who have previously demonstrated a level of activity when the drug was delivered systemically.1,4,5
When antineoplastic agents are administered by the intravenous route, they reach the tumor by capillary flow. Any advantage for intraperitoneal treatment over that achieved with systemic drug delivery will be secondary to the direct free-surface diffusion of the drug from the peritoneal surface into the tumor. This is perhaps the major concern with the use of intraperitoneal therapy because, in general, the depth of penetration of chemotherapeutic agents into tumor tissue is extremely limited (<1 to 2 mm).6,7,8 Therefore, it would be predicted that if intraperitoneal treatment should be shown to be superior to systemic drug administration, it would be in clinical situations in which only very small-volume tumor nodules (1 cm or less) or microscopic disease only are present when intraperitoneal therapy is initiated.
However, it is also relevant to note that in those situations where systemic drug delivery is anticipated to be highly effective in rapidly reducing overall tumor volume (e.g., primary cisplatin-based chemotherapy in ovarian cancer), the initial treatment cycles may permit subsequent intraperitoneal drug delivery (e.g., cycles three to six) to exert a meaningful impact on the ultimate course of the illness.
Finally, there are several practical considerations involved in the potential use of intraperitoneal treatments. A number of investigators have demonstrated both the safety and the convenience of using surgically implanted, semipermanent, indwelling catheters through which the treatments are administered.9,10,11,12 Although percutaneous catheter placement with each treatment course may be used, there is a legitimate concern that the bowel may be punctured during catheter insertion in patients without ascites and in individuals who have previously undergone one or more laparotomies with subsequent adhesion formation.
In contrast to intravenous or intraarterial drug administration, where it can be assumed that blood flow will deliver the antineoplastic agent to the tumor after initiation of the infusion, the use of large treatment volumes (>1 to 2 L) is critical with intraperitoneal therapy to optimize drug distribution. Unfortunately, even with the use of such volumes, there may be portions of the peritoneal cavity that are not adequately bathed by the drug-containing fluid.
Table 9-1 Desired Characteristics of Drugs Considered for Intraperitoneal Therapy | ||||||
|---|---|---|---|---|---|---|
|
SINGLE ANTINEOPLASTIC AGENTS DELIVERED BY THE INTRAPERITONEAL ROUTE
A number of chemotherapeutic and biologic agents have been delivered by the intraperitoneal route in phase I trials designed to define the toxicity and pharmacokinetic profile associated with this route of delivery (Table 9-2).
Cisplatin and Carboplatin
As the platinum drugs are the single most important cytotoxic agents in ovarian cancer,14 it is appropriate that considerable effort has been directed toward exploring the potential for these drugs when delivered by the intraperitoneal route.1 Most regional chemotherapeutic studies have involved cisplatin, rather than carboplatin, based essentially solely on preclinical data (and limited clinical information) suggesting higher intracellular drug concentrations from direct diffusion associated with the older platinum agent.15,16
Several conclusions can be drawn from a review of the results of trials examining the clinical usefulness of intraperitoneal cisplatin. First, after intraperitoneal delivery, the peritoneal cavity is exposed to concentrations of the drug (peak and area under the concentration-time curve levels) that are 10 to 20 times higher than those in the systemic compartment.4,5 Second, there is a limited or no abdominal discomfort associated with intraperitoneal cisplatin delivery.4,5 This allows for an escalation of the intraperitoneal cisplatin dose to maximize systemic delivery of the drug after intraperitoneal administration. In fact, the dose-limiting toxicity of intraperitoneal cisplatin will be systemic side effects of the cytotoxic agent.4 Third, the results of both single-agent and combination cisplatin-based intraperitoneal therapy trials, when delivered in the second-line setting to women with advanced ovarian cancer, have confirmed that patients can achieve surgically documented responses, including complete responses, through the use of this therapeutic strategy.1,13,17
Table 9-2 Pharmacokinetic Advantage Associated with Intraperitoneal Administration of Selected Antineoplastic Agents | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree