Figure 19.4 A. Normal Achilles tendon: aligned parallel collagen fibrils. No extensive foci of fibrillar disruption. B. Charcot Achilles tendon: disruption of collagen fibrils. Irregular appearance compared with normal tendon. Note evidence of glycation of tendon.
Subsequently, a second paper addressed this question of altered Achilles function in the diabetic Charcot foot. Twenty diabetic Charcot Achilles tendons were compared with nine nondiabetic control tendons for ultimate tensile strength and Young’s modulus of elasticity. Results showed significantly less tensile strength and elasticity in Achilles tendons from the Charcot feet. Again, the mechanism for this is believed to be nonenzymatic glycosylation of the collagen (16).
The decreased elasticity may translate clinically as a short tight tendon unable to stretch to permit normal dorsiflexion as the body crosses over the foot during gait. The decreased tensile strength of the Achilles in Charcot may be generalized to include other collagen structures of the foot, including the ligaments, which principally stabilize the midfoot joints; these are potentially prone to failure, and especially so when equinus of the Achilles tendon forces the midfoot joints; they stabilize to dorsiflex as compensation during midstance and toe-off (Fig. 19.5). In fact, some early Charcot midfoot dislocations can be readily surgically managed with lengthening of the Achilles tendon and percutaneous screw stabilization of the subluxing Lisfranc’s joints.
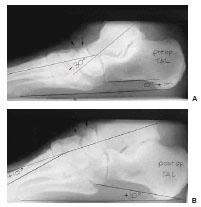
Virtually every Charcot foot reconstruction should begin with an open Z-plasty of the Achilles tendon to an extent that a 90-degree relationship is established between the plantar heel and an imaginary line bisecting the fibula (Fig. 19.6A–C). This re-establishes a positive calcaneal inclination angle as well as decompressing the severely fractured midfoot joints, thus permitting the reconstructive surgeon easier access to these structures for repair (Fig. 19.7A,B).

Figure 19.5 Equinus 90 degree with active dorsiflexion. Short tight Achilles tendon.
Figure 19.6 A. Isolation of the Achilles tendon. B. Open sagittal Z-plasty Achilles tendon lengthening. C. Note the increased dorsiflexion after lengthening.
ANATOMIC RECONSTRUCTION OF THE LISFRANC AND MIDTARSAL JOINTS IN THE CHRONIC CHARCOT FOOT
Both the Lisfranc and midtarsal joints are susceptible to complex fracture dislocations because of Charcot arthropathy. In many instances, both joint segments are affected, requiring realignment and arthrodesis of both hindfoot and midfoot.
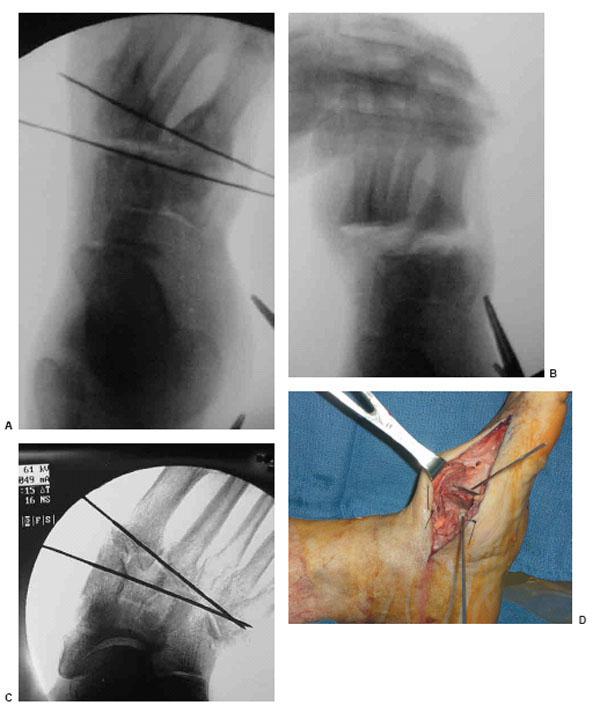
The Lisfranc joint is the easier of the two to repair in Charcot deformity. Depending on whether the forefoot is abducted and dorsiflexed or adducted and inverted, a medially or laterally based osteotomy is cut through the articular surfaces of the Lisfranc joint. After a dorsal envelope, including the neurovascular structures, is created, it is helpful to place two Kirschner wires (K-wires) under fluoroscopic guidance to act as guides for the correctional osteotomy, thereby minimizing excessive bone resection. Once the wedge of bone is resected, the forefoot can be readily manipulated into a correct position against the hindfoot and temporarily held with K-wires until permanent internal fixation is placed (Fig. 19.8A–D).
The repair of the midtarsal joint is considerably more challenging to perform and is at times associated with the need to arthrodese the Lisfranc joint. Often the navicular is resting below the displaced medial cuneiform medially; in these instances, the talus usually accompanies the navicular, producing a near vertical talus on lateral radiographic examination. On AP radiograph, the navicular may appear missing, as the talus appears to articulate with the medial cuneiform, which is blocking the view of the navicular. Similarly, the cuboid is often plantar dislocated beneath the bases of the fourth and fifth metatarsals, such that it appears foreshortened on AP radiographic viewing. On the lateral view, it is often possible to detect that the cuboid is plantar dislocated beneath the metatarsal bases. It is here, laterally at the site of the plantar dislocated cuboid, that an intractable ulceration often forms at the site of most plantar pressure. This ulceration is unlikely to resolve with bracing or special shoe gear.
Figure 19.7 A. Preoperative TAL lateral weight-bearing radiograph. B. Postoperative TAL. Note improved Meary’s and calcaneal inclination angles.
It is the authors’ preferred method to incise both the medial and lateral midtarsal joints with linear incisions beginning approximately 1 cm inferior to and distal to the malleoli, extending distally medially to the base of the first metatarsal and laterally to the base of the fourth metatarsal. Both incisions are deepened to gain direct visualization of the plantar dislocated navicular and/or cuboid. Using a combination of curved osteotomes, lamina spreader and sharp dissection with Sistrunk scissors or scalpel, the dislocated tarsal bones are either relocated into anatomic position, or more often removed from the wound and passed off to the back table for removal of all articular cartilage.
Figure 19.8 A. Lisfranc’s Charcot repair osteotomy with K-wire fluoroscopic guidance. B. Manual manipulation of the bony wedge osteotomy. C. Another example of using the K-wires as an axis osteotomy guide. D. Bony wedge resection at Lisfranc’s joint with K-wire guidance.
Figure 19.9 A. Lateral incision showing the dissection, isolation, and extraction of the Charcot plantarly dislocated cuboid. B. Reinsertion of the cuboid into the arthrodesis site(s) and after removal of all the articular cartilage. C. Medial incision showing the dissection, isolation, and extraction of the Charcot deformed navicular. D. Reinsertion of the navicular into the arthrodesis site(s) and after removal of all articular cartilages.
Once the dislocated tarsal bones are removed, it is relatively facile to manipulate the foot into a rectus alignment on all three body planes and temporarily hold it in place with K-wires. At this time, fluoroscopy imaging is used to determine areas of bony deficit, which can be repaired with grafting of the surgeon’s choice. If the cuboid and/or talus are to be arthrodesed to adjacent bone structures, such as the articular surface of the talus and the calcaneus, then these bones also require removal of all articular cartilage with débridement down to raw subchondral bone (Fig. 19.9A–D). The prepared cuboid and/or navicular can now be reintroduced into their correct anatomic position and temporarily fixated with K-wires.
Variations in the quality and even the presence of these bones can vary from case to case, and this requires a degree of resourcefulness in the reconstructive surgeon. If either or both tarsal bones have been rendered unsuitable for grafting because of the Charcot process or infection, alternatives include freeze-dried iliac crest, fresh-frozen femoral head, or even shortening of the midfoot with arthrodesis of remaining viable bone. This last method, resection of the entire Charcot midfoot, which produces a grossly shortened foot, was the initial technique used for salvage and remains a viable alternative to amputation in cases of osteomyelitis of the midfoot, often complicated by ischemic necrosis and cellulitis of the dorsum of the foot.
INTERNAL FIXATION OF CHARCOT DEFORMITIES USING THE BEAMING TECHNIQUE
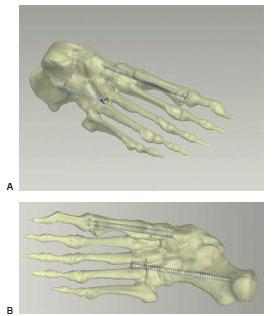
One of the authors developed a beaming technique to internally fixate Charcot midfoot and hindfoot deformities, and has used this method with gratifying results since 1994. The technique was then reported at the American College of Foot and Ankle Surgeons (ACFAS) Meeting in Palm Springs in February of 1997.
Initially, the technique of internal beaming was developed because of breakage of small screws used for fusion whenever pseudarthrosis occurred in these salvage surgeries. Often the broken screws resulted in loss of correction and redeformity. A second reason for development of this technique was as an alternative to large plates, which require removal in instances of dehiscence, again with possible loss of correction.
The use of large-diameter stainless steel screws has many advantages, including:
Figure 19.10 A. Lateral to medial schematic beaming technique placement of large-diameter screws. B. Plantar view of beam placements.
- The screw placed within the medullary canal of the first metatarsal accepts the loads of the medial longitudinal arch, namely, tension plantarly and tension dorsally. Thus, its placement is physiologic, acting as a beam to accept both types of loads through the arch (Fig. 19.10A,B).
- Placement of the medial column screw entering within the head of the first metatarsal and ending in the talus allows an anatomic recreation of Meary’s angle laterally; in fact, an arch can be produced with this technique from a collapsed foot. On AP viewing, the screw aligns the forefoot with the hindfoot directly, correcting varus or valgus angulation.
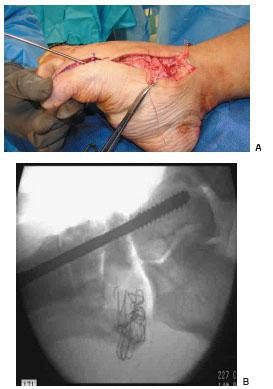
- Because a large diameter cannulated screw is used, its guide pin can be used first under fluoroscopy to readily line up all bone segments on both AP and lateral views. This ability to align the forefoot to the midfoot and hindfoot with a single guide pin on all body planes, followed by rigid internal fixation with a large-diameter intermedullary screw, is an enabling factor of value to the surgeon attempting complex realignment(Fig. 19.11A,B).
Figure 19.11 A. Medial column beaming guide wire. B. Intraoperative fluoroscopy medial column beam placement.
- Bending moment calculations at the Lisfranc’s joint indicate that a cannulated stainless steel screw of at least 7.2 mm diameter provides a 2× safety factor against failure in a 300-lb patient.
- The lateral column also may require beaming; this is particularly true when the cuboid has dislocated or subluxed, and is now relocated. In this case an arthrodesis needs to be effective between the fourth and fifth metatarsal bases to cuboid, and cuboid to calcaneus. In this case a second large-diameter screw is placed laterally, entering the adjacent bases of the lateral metatarsals. This screw should lock its head into at least one metatarsal base to ensure locking of the Lisfranc’s joint to the cuboid; otherwise, if fusion at the Lisfranc’s does not occur, the reactive forces of walking can cause recollapse, or at least loss of some correction (Fig. 19.12A,B).
The beaming technique has proved consistently successful over time in cases in which a true arthrodesis of Charcot joints was obtained, and likewise in cases in which pseudoarthrosis is the final outcome. If the screw diameters are large enough, and the beam is placed across the defective Charcot bone such that both head and tip of the screw are in (relatively) satisfactory bone, then the correction should not fail in spite of pseudoarthrosis.
Figure 19.12 A,B. Lateral and AP radiographs showing the medial and lateral column beaming technique.
One issue that has not been fully resolved in these cases has been the question as to whether or not to fuse the subtalar joint in cases of severe Charcot hindfoot and midtarsal collapse. The subtalar joint when fused connects the independent medial and lateral columns into a unified (regarding weight-bearing) entity. If the columns are locked together, then load sharing between the columns can occur. If pseudoarthrosis is the final outcome in such a case, then by locking up the subtalar joint through arthrodesis, the medial and lateral column beams can load share, thus protecting the correction from recollapse.
THE USE OF EXTERNAL FIXATION IN CHRONIC CHARCOT RECONSTRUCTION
The Ilizarov technique has proved especially useful in cases of Charcot arthropathy. The external fixator frame is extremely useful to compress segments of bone to achieve arthrodesis, offload and protect plantar wounds, bridge across sites of defective or infected bone, and allow access to postoperative diabetic wounds during the healing process (17–19).
Some surgeons initiate weight-bearing with their patients after Charcot reconstruction in an Ilizarov frame with the belief that this load-sharing between the plantar foot on the floor and the external fixation protects the correction and actually speeds bone healing. Recent research proposes a different possible mechanism for this type of healing with Ilizarov bent wire compression frames. Bent wire compression frames showed more compression across an experimental midfoot osteotomy site than a noncompression frame, parallel K-wires, or parallel screws. Additionally, the best compression was shown to occur with a combination of internal screws and an external fixator bent wire frame (20).
External fixators do carry with them an elevated complication rate with pin or wire tract infections, broken wires and/or half pins requiring reapplication, and need for frame adjustment. These complications do not appear to reasonably detract from enhanced outcomes in these difficult cases. The Ilizarov frame presently represents a cornerstone for Charcot limb salvage technique.
THE USE OF LOCKING PLATES IN CHARCOT RECONSTRUCTION
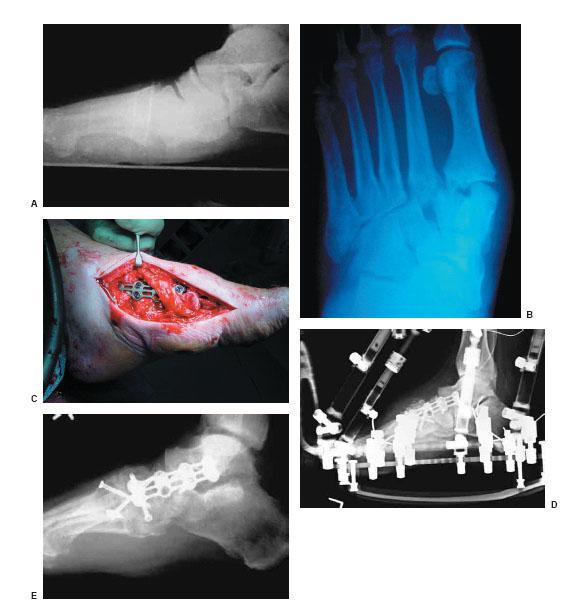
Thus far we have discussed the concepts of beams and external fixation. The common theme is that successful Charcot reconstruction is dependent on intersegmental stability during the biologic fusion process. Another method of obtaining significant stability into the surgical construct is via the use of locking plate technology (Fig. 19.13A–E). The primary advantage to the use of a locking plate along the medial and/or lateral column resides in the plate’s ability to resist strain across the fusion site (4). Perrens’ theory of strain states that there is a relationship between decreasing strain and increasing the potential for osteogenesis across a fracture or fusion site. The strain theory states that for two given fracture segments, the healing interface will have a force-generated motion potential that is contingent on the stability of the original fixation construct. Mathematically, strain is equal to the change in the interface length divided by the original interface length for any given disruptive force. Therefore, with an unstable construct, the healing gap may undergo excessive motion that is described as excessive strain. Strain 2% is considered to be equal to absolute stability, and therefore results in primary bone healing. Strain >10% is described as an unstable construct, and therefore is at great risk of nonunion or delayed union. If strain resides between 2% and 10%, there is micromotion at the bone healing interface, which results in predictable secondary bone healing. In a locking plate construct, in which the plate and the locked screws function as one unit, there is significant resistance to any change in the interfragmentary gap length for any given force. Thus, failure of the locking plate construct only occurs in the face of catastrophic forces at all of the locked screw–bone interfaces.
Figure 19.13 This 64-year-old man presented with a grossly unstable midfoot. A. The apex of the deformity was at the tarsometatarsal and naviculocuneiform joints. A,B. The dominant plane of the deformity was sagittal. C,D. The patient underwent reconstruction via TAL, medial column stabilization via an anterior cervical locking plate, limited internal screw fixation, and static external fixation. E. Note the re-establishment of structural alignment. The time to union and external fixation removal was 10 weeks.
Application of locking plates to the medial and/or lateral column is technically simple and follows the same concepts as any other standard plate fixation. However, care should be taken so that the plate is well-contoured to the bone prior to locked screw insertion. This is because, unlike non-locking plates, the screw does not compress the plate to the bone since the threaded head obviates a lag effect. Also, a small locking plate may be used when the primary fixation is that of a large fragment lag screw placed in a beam technique. This is because the beam provides excellent stability to sagittal and transverse forces, but does little to resist rotational or coronal forces. Therefore, in this construct, the small locking plate acts in a similar way as the static locking screw of an intramedullary rod.
CONCLUSION
Neuro-osteoarthropathy with resultant instability and deformity continues to be a vexing problem today, just as it was in the time of Jean Martin Charcot. However, unlike Charcot, the foot and ankle surgeon of the twenty-first century has many advantages, including advanced diagnostic and imaging techniques, a better understanding of the biomechanics and biology of the disease process, and a multitude of fixation materials.
REFERENCES
- Turek SL. Orthopaedics principles and their application. 3rd ed. Philadelphia: JB Lippincott, 1977.
- Mann RA. DuVries’ surgery of the foot. 4th ed. St. Louis: Mosby, 1978.
- Brodsky JW, Rouse AM. Exostectomy for symptomatic bony prominences in diabetic Charcot feet. Clin Orthop Relat Res 1993;296:21–26.
- Sammarco GJ, Conti SF. Surgical treatment of the neuroarthropathic foot deformity. Foot Ankle Int 1998;19(2):102–109.
- Papa J, Myerson M, Girard P. Salvage, with arthrodesis, in intractable diabetic neuropathic arthropathy of the foot and ankle. J Bone Joint Surg Am 1993; 75(7): 1056–1066.
- Sticha RS, Frascone ST, Wertheimer SJ. Major arthrodesis in patients with neuropathic arthropathy. J Foot Ankle Surg 1996;35(6):560–566.
- Reinherz RP, Cheleuitte ER, Fleischli JG, et al. Identification and treatment of the diabetic neuropathic foot. J Foot Ankle Surg 1995;34(1):74–78.
- Early JS, Hansen ST. Surgical reconstruction of the diabetic foot: a salvage approach for midfoot collapse. Foot Ankle Int 1996;17(6):325–330.
- Gupta R. A short history of neuropathic arthropathy. Clin Orthop Relat Res 1993; 296:43–49.
- Mitchell JK. On a new practice in acute and chronic rheumatism. Am J Med Sci 1831;8:55–64.
- Charcot JM. Sur quelques arthropathies qui paraissent dependre d’une lesion du cerveau ou de la moelle epiniere. Arch Physiol Norm et Pathol 1868;1:161.
- Jordan WR. Neuritic manifestations in diabetes mellitus. Arch Intern Med 1936;57:307–366.
- Glover JL. A 4 year outcome based retrospective study of wound healing and limb salvage in patients with chronic wounds. Adv Wound Care 1997;10: 33–38.
- Centers for Disease Control and Prevention. National diabetes fact sheet: general information and national estimates on diabetes in the United States, 2003. Rev ed. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2004.
- Grant WP, Sullivan R, Sonenshine DS, et al. Electron microscopic investigation of the effects of diabetes mellitus on the Achilles tendon. J Foot Ankle Surg 1997;36(4):272.
- Grant WP, Foreman EJ, Wilson AS, et al. Evaluation of Young’s modulus in Achilles tendon with diabetic neuroarthropathy. J Am Podiatr Med Assoc 2005;95(3):242–246.
- Pinzur M. Ring fixation in Charcot foot and ankle arthropathy. Tech Foot Ankle Surg 2006;5(2):68–73.
- Thompson DM. Ilizarov techniques in the foot and ankle. Curr Opin Orthop 2000;11:108–112.
- Paley D. The correction of complex foot deformities using Ilizarov’s distraction osteotomies. Clin Orthop Relat Res 1993;293:97–111.
- Grant WP, Rubin, LG, Pupp GR, et al. Mechanical testing of seven fixation methods of generation of compression across a midtarsal osteotomy: a comparison of internal and external fixation devices. J Foot Ankle Surg 2007;46(5):325–335.
INTRODUCTION
Charcot neuroarthropathy (CNA) involving the foot and ankle is a rather challenging clinical entity for the foot and ankle surgeon. Although nonoperative therapy is most often effective in maintaining a stable and ulcer-free limb, there are times when surgical management is often necessary for limb salvage. This chapter deals with surgical management of CNA involving the hindfoot and ankle. The use of intramedullary nail fixation is presented in detail. A review of indications, contraindications, technical execution, postoperative management, and complications is presented.
PREOPERATIVE CONSIDERATIONS
Those diabetic patients undergoing CNA reconstruction require an extensive preoperative evaluation. This should include cardiac assessment given that these patients often have silent cardiac disease. Cardiology consultation or thorough cardiac evaluation by the primary treating physician, including an echocardiogram or stress thallium scan, is often necessary to ensure that these patients are safe candidates to undergo a complex reconstructive procedure.
The soft tissue envelope should be thoroughly evaluated for wounds or poor-quality tissue. It is prudent to operate with a closed soft tissue envelope. There is clear evidence that elective surgery in the presence of an open wound increases the incidence of postoperative infection (1). However, there are times when surgery may be necessary in the presence of an open wound. It is important to ensure that there is no evidence of clinical infection within the wound site in these situations. Serial débridements, local wound care, offloading, and antibiotic therapy may be necessary before proceeding to any type of advanced surgical reconstruction.
Some patients may require a social services consultation prior to undergoing surgery. There is a relatively long period of convalescence following surgical intervention that includes non-weight-bearing and limited mobility. Therefore, patients are nonambulatory for an extended period of time. They may require postoperative deep vein thrombosis prophylaxis or have other special needs that are difficult to meet in a home environment. Unfortunately, these patients may have very little family support or are unable to manage themselves. It is often beneficial to have these patients placed in a subacute or rehabilitation facility to assist them during the initial period following surgery.
Advanced imaging may provide some benefit prior to surgical management. CNA often results in avascular bone, which is difficult to ascertain on standard radiographs. Avascular bone requires extensive débridement to obtain a healthy cancellous substrate that will proceed to primary union. Advanced imaging, such as magnetic resonance imaging (MRI), may provide insight as to whether or not avascular necrosis is present and will help with surgical planning. Bone scintography also may be of benefit in situations in which osteomyelitis is a possibility. This is especially beneficial in patients with longstanding open wounds that have failed to heal. It is important to ensure that osteomyelitis is not present prior to surgical reconstruction.
One of the most important preoperative considerations is to thoroughly evaluate the patient’s existing deformity. These patients need to be evaluated both clinically and radiographically. The majority of patients with CNA involving the hindfoot and ankle that have failed nonoperative care usually have frontal plane deformity. Unfortunately, frontal plane deformity, whether grossly unstable or fixed and nonreducible, is often difficult to manage with bracing or shoe therapy. Additionally, a frontal plane deformity is difficult to manage with percutaneous techniques in the presence of a nonreducible deformity. These patients usually require open surgical management. The authors often employ long-leg axial radiographs to evaluate the deformity (2,3). These radiographic views demonstrate the relationship of the tibia, talus, calcaneus, ankle joint, and subtalar joint relative to one another. These views specifically show which anatomic sites are involved and whether one is dealing with a translational versus an angulational deformity (Fig. 20.1).
Figure 20.1 A. Charcot foot demonstrating fixed hindfoot varus. B. Long-leg axial radiograph demonstrating severe angulational deformity between the calcaneus and tibia. C. Another example of a long-leg axial radiograph demonstrating severe lateral translation of the calcaneus relative to the tibia. D. Clinical appearance of the Charcot foot with fixed hindfoot valgus secondary to severe translation demonstrated in (C).
CONTRAINDICATIONS
There are some specific contraindications to CNA reconstruction of the hindfoot and ankle. Uncontrolled diabetes mellitus or malnutrition is an obvious contraindication. Those patients demonstrating elevated hemoglobin A1C levels or longstanding hyperglycemia are precluded from undergoing surgical management. Patients who are medically unfit for any reason, including poor cardiac and renal status and severe peripheral vascular disease, should not undergo any extensive surgical reconstruction. Active infection of either soft tissue or bone is an absolute contraindication to surgical reconstruction. Any soft tissue or osseous infection should undergo thorough débridement, antibiotic therapy, and complete resolution before proceeding to any complex reconstruction. Patients and their families must thoroughly understand what is required during the postoperative period. A patient’s inability to comply or comprehend is an obvious contraindication to surgery. Complications, extended convalescence, and return visits to the hospital and operating room are not uncommon following surgery. These patients must be thoroughly evaluated to ascertain whether they understand what is required following surgery.
Traditional literature has described the acute inflammatory phase of CNA as a contraindication to surgical reconstruction. Sydney Eichenholz has stated that“an arthrodesing procedure to stabilize a Charcot joint during the stage of development is doom to failure.“ Furthermore, he states that“the optimal time for surgery is at the completion of the reconstruction stage” (4). More recent literature, however, has shown that operative intervention during the early stages of CNA produces good outcomes. Shibata presented his results of ankle arthrodesis in Leprotic neuroarthropathy. Twenty-six ankles were reviewed in an average of 9.5 months following ankle arthrodesis. Four of the patients who underwent surgery were early-stage CNA that went on to primary union. However, seven of the 22 patients who were late-stage CNA developed a nonunion. He concluded that arthrodesis was more successful in earlier stages of CNA (5). Simon et al. presented 14 patients undergoing midfoot arthrodesis for CNA. All patients had stage I midfoot involvement. All procedures were successful with no report of ulcerations or complications. They concluded that early operative intervention may expedite the reversal of the destructive CNA process (6). Although the timing of surgical intervention is traditionally recommended in the quiescent stages of CNA, it remains somewhat controversial and should be based on the patient’s unique set of circumstances.
INDICATIONS
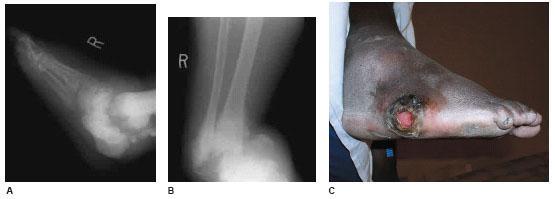
Indications for surgical reconstruction of CNA involving the hindfoot and ankle include a nonreducible deformity with increased plantar pressure, resulting in a nonhealing wound (Fig. 20.2). This includes patients with wounds that proceed to heal when offloaded, but recur when weight-bearing resumes. Surgical intervention to offload an at-risk foot is warranted when bracing and shoe therapy have not been effective or have failed to maintain these patients ulcer free.
The other primary indication for operative intervention is significant deformity with gross instability that is not amenable to brace treatment. Some patients may have significant difficulty tolerating brace therapy. Surgical management should be considered to impart stability to the limb such that brace therapy can be tolerated when gross instability is present.
The primary goals of surgical management are to maintain the patient’s ability to transfer or remain a short distance ambulator. Surgery should restore stability and alignment such that footwear and bracing can be effective.
ANCILLARY PROCEDURES
It is important that a completely plantigrade foot be obtained at the time of the surgery. Therefore, bony resection or realignment must be sufficient to completely reduce any existing deformity. Structural bone graft is rarely necessary in the majority of patients. The authors have found that patients tolerate limb shortening quite well, so long as the foot is plantigrade. Bone graft or bone graft substitutes are often used to enhance arthrodesis. The authors typically use regional bone graft such as the fibula. A bone mill or reamer can be used to morselize the fibula. Morselized autogenous bone can be combined with an orthobiologic substance such as demineralized bone matrix to provide an excellent enhancer to arthrodesis. Additionally, the fibula can serve as a source of structural bone graft should the need arise.
Posterior muscle group lengthening in the form of gastrocnemius recession or Achilles tendon lengthening is required in virtually all patients undergoing CNA reconstruction. This is especially important where there is complete loss of calcaneal inclination. Restoration of calcaneal inclination is difficult without some type of posterior muscle group lengthening.
INTRAMEDULLARY NAIL FIXATION
Intramedullary (IM) nail fixation is preferred when possible. An IM nail with interlocking screws will maintain alignment, length, and stability when bone loss or osteopenia is present. This is often the case in CNA involving the hindfoot and ankle.
Figure 20.2 A–C. Fixed Charcot hindfoot/ankle varus with secondary neurotrophic ulcer along the fifth metatarsal base area.
Additionally, delivery of an IM nail results in minimal disruption of soft tissue relative to fixation devices such as large plates. The proximal and distal interlocking screws impart excellent stability. Additionally, an IM nail serves as a rigid, load-sharing device. This is especially advantageous in CNA patients with poor-quality bone.
There are some contraindications to using an IM nail in CNA patients. An insufficient heel pad or a heel with previous ulceration is often a contraindication. These nails are delivered through the plantar aspect of the heel and soft tissue problems may result if the fat pad is insufficient or of poor quality. Any proximal deformity in the tibia is also a contraindication. Proximal deformity often results in delivery of an IM nail that is too short. Short nails are to be avoided because there is an increased incidence of tibial stress fractures. Lastly, the inability to obtain collinear reduction between the tibia, talus, and calcaneus is an obvious contraindication. A straight IM nail cannot be delivered without collinear reduction of all osseous components.
The IM nails used in hindfoot and ankle reconstruction have evolved to provide greater compression and rotational stability. The first IM nails used in foot and ankle surgery were distal femoral nails designed for supracondylar femur fracture fixation (7,8). The interlocking screws were directed from lateral to medial. Second generation nails added calcaneal locking in the posterior-to-anterior direction to provide rotational stability. In addition, these IM nails allowed compression across the arthrodesis site. Second-generation nails have been shown to provide excellent biomechanical stability. The biomechanical strength can be attributed to the dense bone purchased near the sustentaculum tali and by neutralizing sagittal plane forces at the ankle joint (7–10). Humeral nails have also been evaluated in foot and ankle surgery. The curve in the distal portion of the humeral nail allows for insertion of the nail without medialization of the foot (11). This eliminates the necessity of an additional medial incision and partial resection of medial malleolus or extensive medial malleolar dissection to achieve medial translation (8,11,12).
In several biomechanical studies, the IM nail has been shown to provide stability similar to other forms of fixation. Investigations of primary stability following tibiotalocalcaneal (TTC) arthrodesis with various implants have not proved one implant more superior to another (13,14). Comparative studies between IM nail fixation and blade plate has shown varied results (15,16). In view of the fact that all implants are similar, factors such as osteopenia, quality of soft tissue envelope, and surgeon preference should determine the choice of implant.
IM nails have become a useful device to obtain stability in the foot and ankle. Pinzur et al. reported on 21 CNA ankle fusions with retrograde locked IM nails. They showed 20 cases achieved fusion at 12 to 31 months when talectomy was not required. Overall, they describe their results to be satisfactory (17). The authors prefer to use an IM nail supplemented by a static external fixator whenever possible.
TECHNICAL EXECUTION
Surgery is performed under general inhalation or spinal anesthesia. The authors typically employ a pneumatic thigh tourniquet until osteosynthesis has been achieved. Thereafter, the pneumatic tourniquet is released and hemostasis is achieved prior to a closure. There should be a sandbag or blankets placed under the ipsilateral hip such that the foot can be easily accessed and manipulated from medial to lateral. The foot is usually suspended over a large sponge block or a set of blankets to enhance intraoperative imaging.
The procedures are performed through a combination of medial and lateral incisions. The lateral incision extends from the distal one third of the fibula to the sinus tarsi. Full-thickness dissection is typically employed. All soft tissues are completely elevated and the fibula is resected and saved for possible use as a bone graft. All soft tissues are dissected from the anterior and posterior aspect of the ankle and subtalar joint. Depending on the nature of the deformity, the subtalar joint is thoroughly denuded of all cartilaginous tissues. Small osteotomes can be used to methodically break the subchondral plate. This can also be performed with a side-cutting burr. Attention is then directed to the medial aspect of the ankle, where an incision is made along the anterior aspect of the medial gutter. Care must be taken to tie off vessels that are part of the anterior ankle capsule. The incision is then carried down through the ankle joint capsule and all soft tissues are elevated from the ankle. This gives complete visualization of the ankle joint. The joint is then resected with the use of a sagittal saw. Joint and bony resection depends on the nature and extent of the deformity. One must thoroughly evaluate this area for avascular bone or fibrotic soft tissue. Avascular bone and diseased soft tissue must be thoroughly evacuated. It is important to carry out débridement down to a level of healthy cancellous bone to enhance primary union between bony segments.
Following bony resection and joint preparation, the osseous segments are aligned in a collinear fashion. The talus and calcaneus must be translated medial for proper positioning because the position of the calcaneus is about 1 cm lateral to the distal tibia. Failure to medially translate the foot may result in fracture of the medial cortex of the calcaneus or damage to vital neurovascular structures. Positioning of the foot under the leg to achieve optimal alignment is the most critical aspect of the procedure. Failure to medially translate the foot may result in placement of the IM nail in a valgus angle which can lead to a stress riser along the cortex of the tibia. At times, it may be necessary to resect a portion of the medial malleolus to allow for adequate translation; however, this is uncommon. After translation has been achieved, evaluation of rotational (transverse plane) deformity should be performed to ensure the ankle is not in excessive internal or external position. Alignment should be confirmed with image intensification, including anteroposterior (AP) and lateral view of the ankle and a calcaneal axial view. These three views are usually adequate to ascertain reduction of the osseous segments. Provisional fixation can be obtained with Steinmann pins. An IM nail is then delivered in standard fashion. The exact steps for nail delivery depend on the type of the nail that is being used. Placement of the IM nail should be anterior to the weight-bearing aspect of the calcaneus and slightly lateral to avoid neurovascular structures. Sequential reaming is required for preparation of the intramedullary canal. Most IM nail manufacturers recommend reaming 0.5 mm larger than the nail diameter being inserted. The nail is then delivered with the amount of countersink into the plantar calcaneus, depending on placement of lateral-to-medial screws. Orientation of the screws will be lateral-to-medial at the level of the calcaneus and talus. A posterior-to-anterior screw is also available in some nails, which has been shown to offer better rotational stability. The tibial screws are inserted and can be placed in a medial-to-lateral or lateral-to-medial direction. The nail is inserted in an internally rotated position to bring the interlocking screw holes to a position anterior to the fibula. Every attempt should be made to obtain complete bone-nail interface. This can be difficult because of the small calcaneal bone at the site of insertion and the medially placed nail. A medially placed IM nail may not leave adequate bone for purchase with the lateral-to-medial screws. Compression can be achieved after the proximal screws have been inserted through a mount-ing device. The distal screws are then inserted in either a lateral-to-medial (LM) or posterior-to-anterior (PA) direction. Although the PA screw may provide additional torsional stability to the construct, the surgeon should consider complications of the screw as well. Soft tissue breakdown at the screw head in this area of poor soft tissue coverage can occur. This entire process is performed under image intensification to ensure appropriate alignment, cortical screw purchase, and appropriate screw length. The authors sometimes supplement this construct with large-diameter screws to increase stiffness. The pneumatic ankle tourniquet is then released and hemostasis achieved. Bone graft is then placed to augment arthrodesis sites and/or provide structural support. A close suction drain is beneficial. A static external fixator, which serves as a neutralization device, is often applied.
The nail length should extend beyond the distal isthmus of the tibia. The surgeon should consider using a nail that is as long as possible in the majority of these cases. Longer nails provide for additional stability, particularly in neuropathic patients. Additionally, the use of a longer nail often reduces the incidence of stress risers. Noonan et al. performed a biomechanical analysis of nail length on cadavers that included a strain gauge analysis of cadaver tibiae. They performed an analysis of standard-length IM nails versus longer nails. The standard-length nails increased strain of the posterior tibial cortex at the level of the proximal interlocking screw 5.3 times than that of the longer nail. They concluded that the longer retrograde nails may be more appropriate in patients with neuropathy or osteopenia (18).
The primary goal is complete reduction of frontal plane deformity. Ultimately, a plantigrade foot should be obtained at the time of surgery. Often this requires extensive bony resection and secondary shortening of the extremity. Shortening is usually acceptable and well tolerated in the majority of the patients. However, there are unique situations in which shortening may be rather extensive and a structural bone graft may be necessary. The fibula provides an excellent source of structural autograft if it is viable. The authors also use frozen femoral head allograft, which is osteoconductive and provides volume (Fig. 20.3). This provides an adequate source of structural bone graft. Otherwise, the authors morselize the fibula and combine it with an orthobiologic substance such as demineralized bone matrix. The IM nail is delivered following resection and realignment. The foot segment is then distracted distally over the nail until adequate length is obtained. Interlocking screws are then delivered and the structural bone graft is placed into the deficit (Fig. 20.4). However, this is rarely necessary. More often than not, shortening is well tolerated and easily accommodated with postoperative bracing and shoe therapy (Fig. 20.5).
POSTOPERATIVE MANAGEMENT
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree