Intraarterial Chemotherapy
William D. Ensminger
Intraarterial therapy is significantly more complex, difficult to correctly perform, and carries more risks than conventional standard systemic intravenous or oral therapy in the treatment for cancer. Hence, it is only reasonably applied when administered systemic agents have insufficient efficacy, and/or locoregional approaches are, in turn, unable to eradicate regionally confined cancer. Therefore, advances in cancer treatment using the much more widespread conventional systemic approaches tend to constrain the use of intraarterial therapy. A prime example of this is the development of standard effective systemic chemotherapy regimens for colorectal cancer, which subsequently virtually eliminated the application of hepatic arterial (HA) floxuridine (FUDR) with surgically implanted pumps to treat liver metastases.1,2 In addition, the number of oncologists who believe that there is a role for intraarterial therapy and who are skilled in its application is relatively small. As will be seen later, almost all of the current application of intraarterial therapy utilizes interventional radiographic techniques and the active participation of the radiologist in the therapy. This chapter will describe the rationale for, the principles of, and the major applications of intraarterial therapy.
The natural history of many solid tumors includes a period of confinement to a specific body region. Even with metastatic tumors, there may be one specific organ that is the primary (and sometimes sole) site of tumor growth and resultant morbidity and mortality. The limitation or concentration of metastases to a single organ or several organs has been highlighted as a clinically significant situation termed the oligometastatic state.3 Tumors generally induce a blood supply from the organ in which they grow; therefore, the arterial supply to such an organ provides direct access to the tumor as a potential means to obtain higher tumor exposure to the therapeutic agent in question. The objective of intraarterial therapy is to achieve increased tumor regression in the body region served by the artery infused relative to tumor regression possible with systemic oral or intravenous therapies. Although decreased systemic toxicity is desirable, often it is not the primary aim in as much as the dose is usually escalated to the maximum-tolerated toxicity, whether regional or systemic. Decreased systemic toxicity is important, however, if one wants to add systemic therapy to intraarterial therapy without compromise of either. Factors influencing the achievement of the goals of intraarterial therapy are discussed in the following text.
Surgical resection, radiotherapy, and ablative procedures (radiofrequency/cryosurgery) are locoregional approaches sharing the same objective as intraarterial therapy. These treatment modalities may compete for a segment of the patient population having regionally confined tumors, although they may be used in combination with each other and intraarterial therapy in the treatment for primary and metastatic tumor of the liver. The constraints of each of these three regional treatment modalities are similar: inability to treat systemic disease in other organs, incomplete locoregional tumor eradication, and limiting regional tolerance. As will be described in the following text, treatments combining intraarterial therapy with either surgical resection and/or radiotherapy have been applied to further regional tumor control with particular success in hepatocellular carcinoma (HCC).4,5,6
REQUIREMENTS FOR SUCCESSFUL INTRAARTERIAL THERAPY
Anatomic Considerations
Regional Tumor Confinement
Several anatomic considerations bear on the appropriateness of intraarterial therapy. The first consideration is the necessity to have a regionally confined tumor. Therefore, although the liver is frequently involved with metastatic lung cancer, breast cancer, and melanoma, these tumor types are almost uniformly systemic and involve other organs. Eradication of these tumor types within the liver usually would have little benefit, as morbidity and mortality in other sites would quickly come to the fore because of the aggressive metastatic nature of these cancers. Although many patients with colorectal cancer metastatic to the liver seem to have metastases limited to the liver, effective control of the liver metastases allows time for other metastatic sites to develop and become obvious.7 Nonetheless, the fact that an increasing number of patients with countable numbers of liver metastases from colorectal cancer can be cured with the application of effective systemic chemotherapy aided by surgical resection suggests that the liver can sometimes be the only site of metastatic disease in this type of cancer.8 Additionally, the fact that liver transplantation can cure some 70% of patients with 3 or fewer nodules <3 cm in size or 1 <5 cm of hepatocellular cancer nodules demonstrates that this tumor type does not uniformly metastasize outside of the liver.9 As will be seen below, there is benefit for the regional treatment for HCC and many neuroendocrine liver metastases because of the vast majority of the tumor burden being resident in the liver for an extended period and causing symptoms therein. Such is not generally the case for lung cancer, breast cancer,
and melanoma. Therefore, regional tumor confinement and the duration of such confinement are major considerations in defining the potential benefit of intraarterial therapy.
and melanoma. Therefore, regional tumor confinement and the duration of such confinement are major considerations in defining the potential benefit of intraarterial therapy.
Tumor Blood Supply
The most current intraarterial therapy is directed against liver tumors (which has been the case historically). The rationale for HA infusions is well-defined. The liver is unique among large organs in having a dual blood supply. Most of the nutrient supply to the normal liver is through the portal vein, and occlusion of the hepatic artery is fairly well-tolerated.10,11,12 On the other hand, tumors within the liver receive approximately 95% of their blood supply from the hepatic artery. Agents given into the hepatic artery selectively can affect the tumor with sparing of uptake into normal liver.13 The relatively large size of the hepatic artery makes its catheterization relatively easy, and the widespread knowledge about the segmental arterial supply allows for selective catheterization of quite small arteries supplying tumor nodules.
To obtain the benefits of intraarterial therapy, the tumor blood supply must be accessible and unique. Furthermore, therapeutic agents must be given directly into the arterial supply feeding the tumor within an organ or body region. When the attempt is to treat the entire organ because of the probable presence of scattered occult cancer, achievement of this aim can be very difficult because of anatomic variation as described earlier in patients undergoing HA therapy with implanted pumps and HA catheters for FUDR.14 It is not sufficient, however, to assume that there is uniform distribution of an agent within the blood flowing through the artery into which the agent is injected or infused.15,16 Streaming because of laminar flow can occur as low-flow rates relative to blood flow, leading to high concentrations of the therapeutic agent going into some tributaries of the artery being infused and negligible concentrations going into others. Tumors exposed to high concentrations of agent have the potential to respond, whereas others not being directly infused will not.17 Controversy exists about the degree to which streaming occurs within an artery and accounts for inhomogeneous tumor regression as seen when low-flow rate FUDR is administered via an implanted system.16,18
The flow rates used for the injection of agents used in the embolization procedures to be described later are much higher and equivalent to or greater than arterial blood flow. The high injection rates used in HA embolization therapies causes turbulent mixing and achieves a relatively homogeneous distribution throughout the arterial bed being injected.
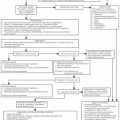
In addition to ensuring flow to the tumor-bearing region, the application of a tracer agent is important in preventing toxicity because of direct flow to other organs that may not be as tolerant as the target organ. Currently, a pretreatment angiographic procedure is utilized before subsequent injection of yttrium 90 microspheres into the hepatic artery for treatment (see below). During this procedure, vessels are occluded so as to direct all flow to the liver tumor. Radiolabeled 99mTc-MAA injection and a nuclear medicine scan are used to define the best catheter position and provide guidance in the embolization/occlusion of vessels necessary to confine flow to the region desired.19,20 Delivery of a cytotoxic agent to the stomach or duodenum can produce severe injury to these organs.21,22
The distribution of tumor within the organ or region infused is an important consideration relative to the other two major regional treatment modalities, that is, surgery and radiation. For example, whereas a countable number of hepatic colorectal or neuroendocrine cancer nodules might be excised, many small nodules throughout the liver would not be removable for cure, but could be treated by intraarterial therapy. Similarly for external beam radiotherapy, whereas a limited number of isolated tumors might be effectively treated with refined dosimetry techniques such as stereotactic body radiotherapy, organ or regional tolerance might not allow for enough dosage for radiotherapy alone to treat multiple, widely dispersed tumor nodules effectively.6,23 The best clinical practice is to evaluate the location of regionally confined tumors and to consider how best to apply available treatment modalities individually or in combination. In this regard, comparison of the effectiveness of one regional modality with another must involve great care to make sure the disease processes being treated are similar. For example, patients having a countable number of resectable hepatic colorectal tumor metastases have a different intrinsic prognosis than those patients having several pancreatic liver metastases or those with 80% of their liver replaced by innumerable nodules of multifocal carcinoma.8
DRUG-DELIVERY MECHANISM
Arterial Access
Radiologic versus Surgical Catheter Placement
Intraarterial therapy requires a mechanism of access so that a therapeutic agent can be infused into the appropriate artery feeding the tumor confined to the specific body region.24 Short-term access (minutes to hours) is most conveniently achieved using a plastic catheter percutaneously inserted into a major arm or leg artery with advancement and radiologic/fluoroscopic positioning of the tip into the appropriate regional artery to receive the therapeutic agent. The techniques involved in such catheter tip positioning and, initially, in defining the correct artery for infusion, fall within the domain of interventional angiography.14 For reasons that will be outlined below, chronic arterial access (weeks to years) is usually achieved with surgically implanted silicone rubber catheters. Nearly all catheter placements for intraarterial delivery of therapeutic agents are conducted by interventional radiologists and involve shortterm access in the outpatient setting. In those limited situations where chronic arterial access (weeks to years) is desired, surgically implanted silicone rubber catheters are most appropriate. In the short term, radiologic catheters can be positioned precisely with minimal impact on the clinical state of the patient. The physiologic stress of surgical catheter placement is much greater. Radiologic catheter placement is generally considerably less costly than surgical catheter placement. Surgical catheters
are usually connected to subcutaneously implanted access ports or pumps, resulting in totally implanted systems that, once placed, are more acceptable to patients for chronic treatments. Table 10-1 compares radiologic catheter placement with surgical catheter placement.
are usually connected to subcutaneously implanted access ports or pumps, resulting in totally implanted systems that, once placed, are more acceptable to patients for chronic treatments. Table 10-1 compares radiologic catheter placement with surgical catheter placement.
Table 10-1 Comparative Characteristics of Radiologic versus Surgical Catheters in Intraarterial Therapy | |||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||
With percutaneously inserted, angiographically positioned catheters, there is rarely sufficient catheter tip stability to allow for long-term infusions. One factor in catheter tip stability relates to catheter movement generated by motion of the insertion site. When the femoral artery is used, patients must refrain from walking, and such immobility carries the risk of deep venous thrombosis of leg veins. Insertion of angiographic catheters through the left brachial artery provides the safest route for protracted access (1 to 2 weeks) in that patients remain mobile and right-handed patients can use their dominant arm. The left arm is preferable to the right because there is less risk of vertebral artery thrombosis or emboli as the origin of the left-vertebral artery is directly from the aorta.
Motion of the organ or body region being infused can lead to catheter tip displacement. For example, catheter tip motion occurs naturally with liver movement during diaphragmatic excursions with respiration. Movement of the hepatic artery so induced can lead to the tip migrating either distally or proximally in the artery. The position of the tip of surgically placed catheters relative to the artery being infused is generally defined at the time of operation, with the fixation site within several millimeters of the tip.22 For that reason, catheter tip migration is much less common, making surgical catheter placement the mechanism of choice for long-term (months to years) intraarterial access. Even with surgically placed catheters, attention to the detailed arterial anatomy and the acquisition of sufficient surgical experience are prerequisites for a high success rate.25,26
As is true with systemic cancer therapies, the cost of the therapeutic agents delivered via the catheter is generally much greater than the procedure cost, be it an interventional radiologic angiogram or a surgical catheter placement.
Thrombosis
Thrombotic events influence arterial infusion in two ways. First, thrombosis of the vessel being infused removes the potential for further intraarterial therapy in most instances and may seriously compromise blood flow to the organ in question. For example, thrombosis of the internal carotid artery during a drug infusion of a brain tumor would be catastrophic. Second, clot formation on or caused by the catheter may lead to thrombotic emboli. Such emboli can cause strokes when they go to the brain and ischemia in the extremity bearing the insertion site for percutaneously placed catheters. Thrombotic events bear a relation to several factors, including intimal damage by the catheter tip, catheter material, area of the catheter exposed in the arterial stream, induction of turbulence by the catheter, duration of exposure to the catheter, and the thrombotic potential of the patient (which may be increased in some cancer patients).
Intimal damage by the catheter tip occurs more frequently with radiologic catheters than with surgical catheters.22,27 Plastic radiologic catheters are stiff, and the tip configuration and motion relative to the arterial wall are critical with considerable potential for an angled tip to tear into the intima and lead to thrombosis. Radiologic catheters can cause arterial thrombosis at their percutaneous arterial insertion site, whereas surgically placed catheters cannot. Surgically placed silicone rubber catheters are much softer and, the tip is generally secured so that it does not abut/tear into the arterial wall. In addition, lack of motion relative to the arterial wall (as is the case with surgically placed catheters) decreases the chance of intimal trauma. Essentially, the entire length of the radiologic catheter (which may be 50 to 100 cm) is within the arterial system and rubbing on the arterial walls, whereas only 0.1 cm or so (the tip) of the surgical catheter is within the arterial flow. The potential for turbulence is variable and relates to catheter tip configuration relative to blood flow. It is difficult to evaluate turbulence in vivo. Turbulence that produces an increased chance of thrombosis and intimal damage may favorably influence drug mixing in the artery.16 Comparative clinical data in controlled studies evaluating the intrinsic thrombogenic potential of plastic catheters versus silicone rubber catheters in intraarterial therapy are not available, although research continues on new catheter materials. The thrombotic potential of intraarterial therapy is certainly increased in some cancer patients owing to a relative hypercoagulable state. Unfortunately, no easy test can evaluate the risk in any given patient.
Infections and Pumps
The topic of infections and that of implanted pumps is wellcovered in the fourth edition of this book. Both of these topics are applicable to chronic intraarterial infusions and not to the currently utilized therapies described below.
EFFECTIVE AND APPROPRIATE DRUG
Dose-Response Effect
As outlined in Table 10-2, there are several properties essential to the appropriateness of using a drug intraarterially in a given tumor type situated in a particular body region. One consideration is that tumor cytotoxicity be proportional to the level of exposure to the drug in question. Knowledge of the dose-response curve can allow for the assessment of the potential additional antitumor effect possible when intraarterial therapy can achieve definable increases in the level of regional drug exposure relative to those possible with conventional intravenous administration. Despite improved regional drug exposure, antitumor effect may not be significantly better for tumors that are either too sensitive or too refractory.28 For tumors that are very sensitive to a given drug, intravenous administration may suffice to generate maximal antitumor effect (i.e., the dose-response curve is such that the response has already reached a plateau at concentrations/exposures achievable by the intravenous route). If a tumor is absolutely resistant to all concentrations of a given drug (a phenomenon observed in tumor cell culture systems), then the increased exposure generated through an intraarterial infusion of drug will be of no benefit. Unfortunately, few dose-response or response versus concentration data exist for most tumors in the clinical situation.
Consideration of the selectivity of dose-response effects must take into account the tolerance of the normal tissues within the distribution of the artery being infused. Although tolerance of a systemic tissue may ordinarily be dose limiting with systemic drug administration, regional drug infusions may raise the exposure of normal tissues in the infused region to such a level that they soon become dose limiting instead. For example, HA infusion of FUDR can lead to hepatobiliary toxicity, which is not seen with intravenous infusions.22,29,30 Intraarterial infusions of agents in head and neck cancer can generate mucositis, and arterial infusion of tumors of the extremities can lead to dermatitis in the distribution of the infused arteries.31,32 The localized regional toxicities that develop from intraarterial infusion are indicative of the higher locoregional drug exposure being achieved with intraarterial treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree