Abdominal wound infection following cesarean section or gynecologic surgery is a common complication that accounts for significant extension of hospital stays and adds considerable cost to hospital bills. For example, it is estimated that the incidence of wound infections ranges from 3% to 15% for cesarean deliveries and 3% to 8% for abdominal hysterectomies. The direct cost of a wound infection has been estimated recently at $4,000. A wound is defined as “infected” if pus discharges and as “possibly infected” if the wound develops the signs of inflammation or serous discharge. For more than 40 years, a standard classification of surgical wounds has been used
(see Table 21.1).
Pathogenesis
Two overall factors determine whether a wound will become infected: the amount of bacterial contamination and the resistance of the patient. Bacterial contamination is either endogenous, from the patient’s own microbial flora, or exogenous, from the environment. The source of endogenous bacteria in obstetric or gynecologic abdominal wound infections is either the abdominal skin or the flora of the vagina and cervix.
The condition of the wound is important in determining local resistance and to a large extent is a reflection of surgical technique. Gentle tissue handling, complete hemostasis, debridement of devitalized tissue, adequate blood supply, obliteration of dead space, and closing of the wound without tension are principles of good surgical technique. Hematomas or foreign bodies in the wound predispose to the development of infection. Hemoglobin interferes with leukocyte migration and phagocytosis. An inadequate blood supply leads to lower oxygen tension and acidosis in the wound, with the resultant inability of macrophages to kill bacteria.
In general surgery, identified risk factors for wound abscess are bacterial contamination of the wound, older age, obesity, hypothermia, stress, inadequate nutrition, longer operating time, use of drains, increased duration of preoperative hospitalization, diabetes, malnutrition, use of steroids (in some studies), puncture of the surgeon’s gloves, and shaving or clipping of hair at the operative site (compared with use of a depilatory cream or no hair removal).
Risk factors for wound abscess after cesarean delivery include obesity, diabetes, chorioamnionitis and postoperative endometritis (as well as risk factors for these latter two infections including longer duration of labor, longer interval from rupture of membranes to delivery, increased number of vaginal examinations, and longer duration of internal fetal monitoring).
Microbiology
In
Table 21.2, we display the organisms found in wound infections after cesarean delivery in two studies. In one study, the authors noted that wound infections caused by cervical/vaginal flora were associated with prolonged labor, longer duration of fetal monitoring, larger number of vaginal examinations, and with organisms isolated from the endometrium at cesarean section. In comparison, infections associated with
Staphylococcus aureus had neither prolonged labor nor
S. aureus isolated at cesarean section. They reasoned that the former wound infections resulted from ascending infection from genital organisms, whereas the infections with
S. aureus presumably arose from exogenous sources.
Clinical Presentation and Treatment
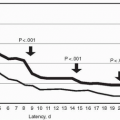
Most wound infections become apparent on postoperative days 4 to 7, but in one study about 25% were evident on day 3 or sooner and about 10% on or after day 8. Timing of the onset of wound infection may provide a diagnostic clue about the infecting organism.
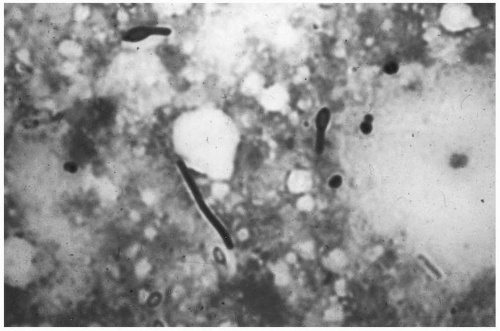
Early-onset wound infection occurs within the first 48 hours postoperatively often in the initial 12 to 24 hours. Patients present with an elevated temperature and an alteration in appearance of the abdominal wound. This may be a spreading cellulitis or discoloration of the skin in association with an advancing margin of active infection. Early-onset wound
infection usually is caused by a single bacterial pathogen, most commonly group A streptococcus or
Clostridium perfringens (Fig. 21.1). Gram stain of material aspirated from the active margin of infection may be diagnostic. Gram-positive rods are strongly suggestive of clostridia; gram-positive cocci indicate the probable presence of group A streptococci. Infection caused by group A streptococci should be suspected if the patient develops a diffuse cellulitis, systemic illness, or both. Group B streptococci may present a similar picture. In clostridial infection, cellulitis of the skin and subcutaneous tissue may appear with a watery discharge, followed by the characteristic bronze appearance of the skin and crepitation in the vicinity of the wound.
The treatment of early-onset wound infection consists of antibiotics and excision of necrotic tissue. Penicillin is the antibiotic of choice for both clostridia and group A streptococcus,
but broader spectrum therapy is used initially for cellulitis as the identification of infecting organisms is not known initially. If the wound cellulitis is not extensive, it is reasonable to treat with antibiotics initially and local wound care such as warm soaks. However, extensive debridement and excision of necrotic tissue is often required.