Indistinct and Spiculated Masses
A poorly defined mass on mammography is a primary sign of breast carcinoma. The majority of breast carcinomas have an infiltrative, irregular appearance with spiculation (1). A variety of benign lesions, including fibrocystic changes (fibrosis, cysts, hyperplasia), radial scars, fat necrosis, hematomas, abscesses, and scars may also present as poorly defined masses radiographically. In addition to the mammographic findings, clinical history and physical examination may be of help in differentiating these lesions. However, in many cases, biopsy is necessary to confirm the etiology of a poorly defined mammographic lesion.
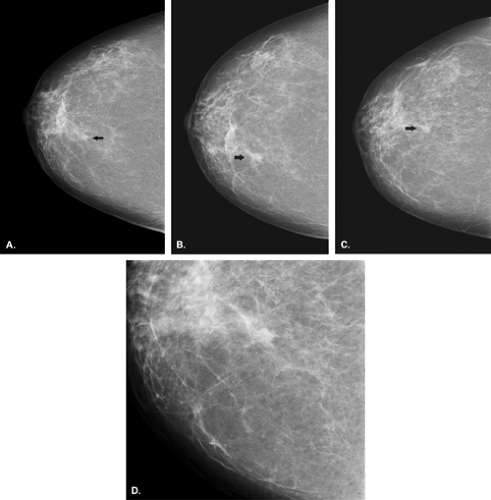
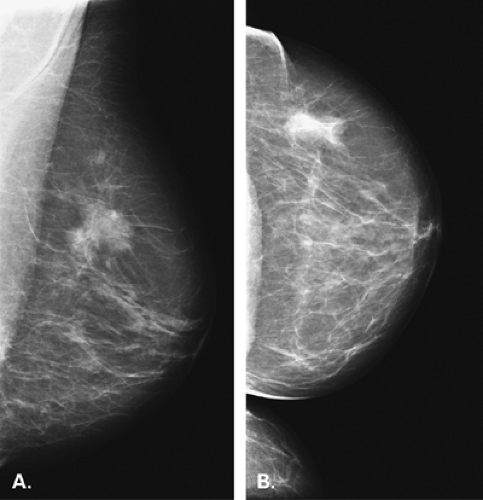
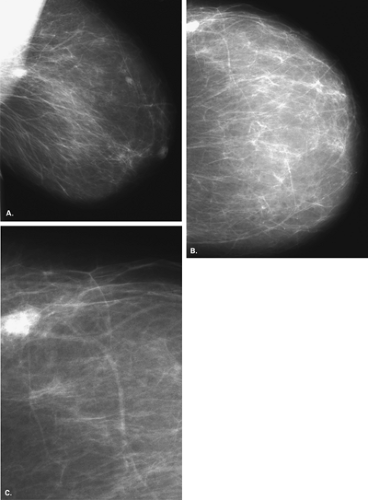
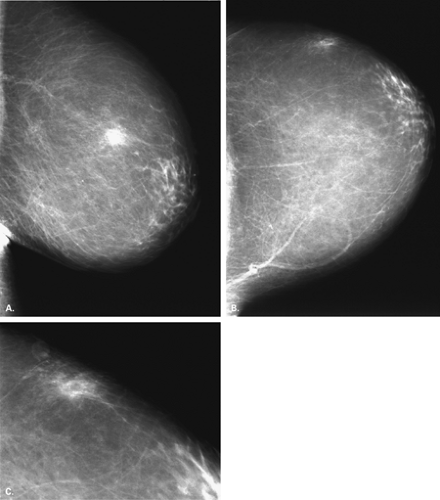
The BI-RADS® Lexicon (2) defines mass shapes as round, oval, lobular, and irregular and mass margins as circumscribed, obscured, microlobulated, indistinct, and spiculated. Indistinct masses are those in which a lesion or portion of the margin is fuzzy or poorly defined (Fig. 5.1). The shape of an indistinct mass may be any of those listed above. The importance of identifying an indistinctly marginated mass is that biopsy is necessary unless the mass represents a postsurgical finding. A spiculated mass (Fig. 5.2) has a margin that is composed of fine tendrils that surround the lesion. This pattern is highly suggestive of malignancy unless it represents a postsurgical scar. Therefore, history and clinical examination confirming the location of the scar are key to suggesting the correct diagnosis.
It is important to determine that an ill-defined lesion can be identified on two projections and is a true mass. Overlying glandular tissue can be visualized on one projection as an irregular density but on the orthogonal view is seen to disperse. If a density has a similar configuration on two projections, more complete evaluation is necessary. Spot-compression views of the lesion may be of help in evaluating its central density and in displacing the surrounding glandular tissue. The presence of a radiolucent center within a poorly defined density suggests a fibrocystic process as a likely etiology (3) or a radial scar, but it is not confirmatory. Ultrasound is also helpful in the assessment of a poorly defined mass. In particular, if a solid mass is identified on ultrasound, percutaneous biopsy with ultrasound guidance can be performed.
Secondary signs of malignancy, such as architectural distortion or microcalcifications associated with an irregular mass, are highly suspicious for carcinoma. The presence of pleomorphic or linear calcifications within and/or adjacent to an indistinct or spiculated mass increase the probability that the lesion is malignant. Even without secondary signs, if an irregular mass has high-density center and fine surrounding spicules, it is regarded as suspicious for carcinoma.
Fibrocystic Change
Cancer must be considered first when an indistinct or spiculated mass is identified on mammography. However, several benign lesions can be pseudoinfiltrative on pathology and produce an appearance on mammography that is suspicious for malignancy. Most often, false positives that manifest as suspicious mammographic masses are some form of fibrocystic change, including radial scar. These lesions may be associated with microcalcifications as well, which can increase the level of suspicion for malignancy.
Hermann et al. (4) found that lesions that mimic breast cancer on mammography because they present as indistinct or spiculated masses include fibrocystic changes, fibroadenomas, or residual parenchyma in an involuting breast. Keen et al. (5) described nine lesions that presented as masses simulating carcinoma because of their margination. Indurative mastopathy (radial scar) or sclerosing papillary proliferation were the diagnoses in four patients, infarcted papilloma in one, sclerosing adenosis in three, and fat necrosis in one. In these cases, the margins of the lesion on pathologic examination were irregular and pseudoinfiltrative, and this correlates with the mammographic appearance.
Sclerosing adenosis is a form of fibrocystic change characterized by a proliferation of lobules with surrounding fibrous sclerosis (6). When the condition is localized, it may masquerade as cancer on mammography and has been confused with carcinoma on histologic examination. In the early stages, there is a florid proliferation of epithelial cells. In later stages, stromal fibrosis occurs, in which coalescence of adjacent lobules produces areas of fibroepithelial proliferation and loss of normal lobular architecture (1). If the process is diffuse, the mammographic finding is diffuse, and small nodules with microcalcifications may be present. If the condition is localized, a mass with indistinct margins is often seen (1) (Figs. 5.3 and 5.4). In a series of 27 cases of sclerosing adenosis, Nielsen and Nielsen (7) reported an irregular density as the most frequent finding, but circumscribed and stellate masses were also seen. Although the density of the center of an area of sclerosing adenosis may not be as great as that of a malignancy, and the spicules may not radiate completely around the lesion, it is often impossible on mammography to differentiate such an area with certainty from a carcinoma. Therefore, sclerosing adenosis is a diagnosis made by biopsy and not by imaging alone.
A variety of forms of focal fibrocystic changes may appear as ill-defined lesions on mammography (Figs. 5.5,5.6,5.7,5.8,5.9,5.10). Focal fibrosis is a benign condition in which there is dense stromal fibrous tissue without cysts or epithelial changes (8). On mammography, fibrosis appears as dense tissue that is often irregularly marginated (9). Irregular microcalcifications that have a coarse pleomorphic appearance may be associated with fibrosis, and these may occasionally simulate carcinoma. Although biopsy is often necessary to confirm the nature of the lesion, the lack of fine linear tendrils around the border of the lesion suggests that malignancy is a somewhat less likely diagnosis. Harvey et al. (10) found that fibrous nodules that were diagnosed on core biopsy were most often masses with circumscribed or indistinct margins, but in about one fourth of cases, the findings were suspicious for malignancy.
An area of common epithelial hyperplasia or atypical ductal hyperplasia may occasionally present in a variety of ways, including as a small indistinct mass. Even a cyst or collection of cysts associated with surrounding fibrous stroma or inflammation may appear as a poorly defined
lesion. Because of the similarities in appearance of many types of fibrocystic change and in breast cancer, many biopsies performed for indistinct lesions are found to represent fibrocystic change on pathology.
lesion. Because of the similarities in appearance of many types of fibrocystic change and in breast cancer, many biopsies performed for indistinct lesions are found to represent fibrocystic change on pathology.
Pseudoangiomatous Stromal Hyperplasia
Pseudoangiomatous stromal hyperplasia (PASH) is a benign lesion first described by Vuitch et al. in 1986 (11). PASH may mimic breast cancer, because it may present as an irregular or indistinctly marginated mass, although often the lesion is circumscribed (12). PASH is a benign mesenchymal neoplasm composed of myofibroblasts sometimes with glandular hyperplasia.
PASH typically occurs in women younger than age 50 who typically present with a palpable mass. On mammography, PASH may present as a lobular circumscribed mass or as an indistinct distorted mass. The striking histologic feature is the complex pattern of large, empty anastomosing spaces in the dense collagenous stroma. Because of this appearance, PASH is sometimes mistaken for angiosarcoma on histology (13).
Radial Scar
Radial scar is a rosettelike proliferative breast lesion (14) that has also been described as sclerosing papillary proliferation (15), benign sclerosing ductal proliferation (16), nonencapsulated sclerosing lesion (17), infiltrating epitheliosis,
and indurative mastopathy (18). The lesion has been confused with cancer by mammographers (19) and pathologists.
and indurative mastopathy (18). The lesion has been confused with cancer by mammographers (19) and pathologists.
In a study of 32 cases of radial scar, Andersen and Gram (14) found most lesions to be small (mean diameter of 7 mm) and in a stellate configuration. On histology, a fibroelastic center is surrounded by lobules and ducts radiating outward. In 93% of cases, either papillomatosis or a benign epithelial proliferation was present. Small round microcalcifications were seen in 63% of cases (14). Because of the presence of elastosis with sclerosis and ductal distortion, a pseudoinfiltrative pattern occurs, and the lesion may be confused with carcinoma histologically (18).
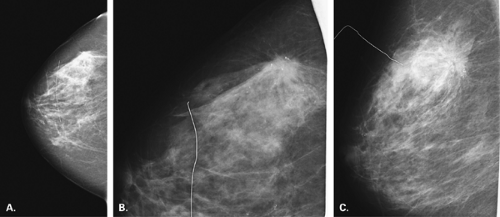
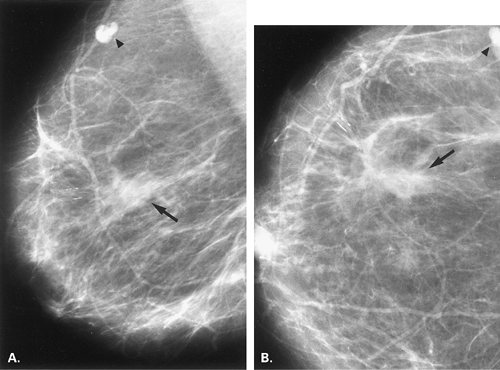
On mammography, a radial scar is a spiculated defined lesion that produces retraction and distortion of surrounding structure (20) (Fig. 5.11). Microcalcifications may be associated with radial scar. Mitnick et al. (21) found mammography to be unreliable in differentiating radial scar from infiltrating carcinomas. The presence of small radiolucencies with the lesion are more in favor of a radial scar than of malignancy (3), but histologic examination is necessary to confirm the diagnosis (20,21).
Posttraumatic Changes
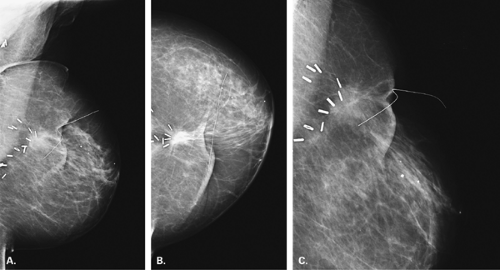
Intraparenchymal scars after biopsy appear as poorly defined masses, often with spiculated margins (22) (Figs. 5.12,5.13,5.14). Scars and posttraumatic changes are more visible in the first 6 months after biopsy and are less prominent after several years (23). A feature of scars that may help to differentiate them from cancers on mammography is that a scar tends to have a different configuration and density on the orthogonal views of the breast. In patients who have undergone lumpectomy and radiation therapy for treatment of primary breast carcinoma, a prominent area of scarring at the surgical site may resemble recurrent carcinoma (24,25). In these patients, it is particularly
useful to have an initial mammogram after surgery, before radiation therapy is started (26), to serve as a basis for future comparisons of the irregular postoperative density that may be present at the lumpectomy site.
useful to have an initial mammogram after surgery, before radiation therapy is started (26), to serve as a basis for future comparisons of the irregular postoperative density that may be present at the lumpectomy site.
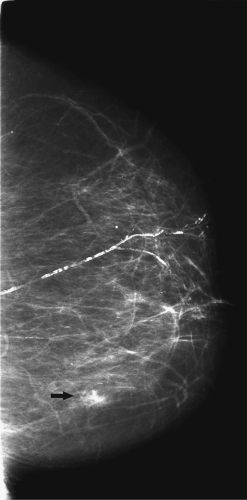
An acute response to trauma, such as a hematoma, may also appear as an indistinct mass (Fig. 5.15) or as a diffuse increase in density. Another radiographic feature of a hematoma that may simulate a cancer is the overlying skin thickening from the edema and bruising. Hematomas tend to resolve over a period of 3 to 4 weeks (27) but may occasionally persist for a longer time, particularly if they are of a large size. Clinical correlation is important in suggesting the correct diagnosis. Ultrasound also is helpful in demonstrating a fluid collection.
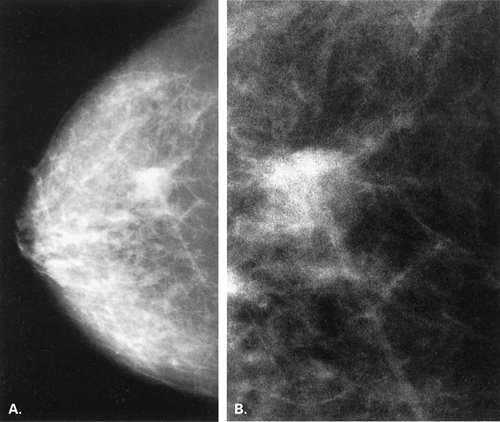
Fat necrosis is a nonsuppurative inflammatory response to trauma. Particularly if the area is associated with a desmoplastic reaction, fat necrosis may be confused with carcinoma on clinical examination. One manifestation of fat necrosis mammographically is an irregular mass that simulates carcinoma (1) (Figs. 5.16,5.17,5.18,5.19,5.20,5.21,5.22,5.23). Thickening and retraction of overlying skin may occur. On histologic examination of an area of fat necrosis, fibrous connective tissue proliferates at the periphery of the necrotic debris. The extent of fibrous response correlates with mammographic image. A marked response may appear on mammography as a spiculated mass resembling carcinoma, whereas a mild response occurs when a thin-walled radiolucent oil cyst is seen (26). Correlation with clinical history is the key in suggesting the presence of fat necrosis. The history of
a recent biopsy or severe blunt trauma in the area of abnormality should alert one to the possibility of fat necrosis. If there is any doubt about the location of a spiculated mass relative to a surgical scar, metallic markers or a wire should be placed over the scar and the film repeated to verify its position.
a recent biopsy or severe blunt trauma in the area of abnormality should alert one to the possibility of fat necrosis. If there is any doubt about the location of a spiculated mass relative to a surgical scar, metallic markers or a wire should be placed over the scar and the film repeated to verify its position.
Abscess
A breast abscess is often suspected on clinical examination because of the very tender, red, hot indurated area. Abscesses tend to occur in lactating breasts, but occasionally may occur in nonlactating women. If a lesion having the clinical appearance of an abscess is found in a nonlactating patient, it should be regarded with suspicion. Most abscesses occur in the subareolar area (20), and skin and areolar thickening may be present (Figs. 5.24,5.25,5.26). Because of the extreme tenderness and the level of clinical suspicion in patients with breast abscesses, mammography may not be performed in the acute stages. The clinical appearance of a breast abscess
may be difficult to differentiate from an inflammatory carcinoma, and needle biopsy is usually performed in the acute stages. Mammography is necessary after therapy to evaluate the remainder of the breast. In an older patient, in particular, abscesses are not common and may be associated with a nearby malignancy or a papilloma obstructing a duct (Fig. 5.27).
may be difficult to differentiate from an inflammatory carcinoma, and needle biopsy is usually performed in the acute stages. Mammography is necessary after therapy to evaluate the remainder of the breast. In an older patient, in particular, abscesses are not common and may be associated with a nearby malignancy or a papilloma obstructing a duct (Fig. 5.27).
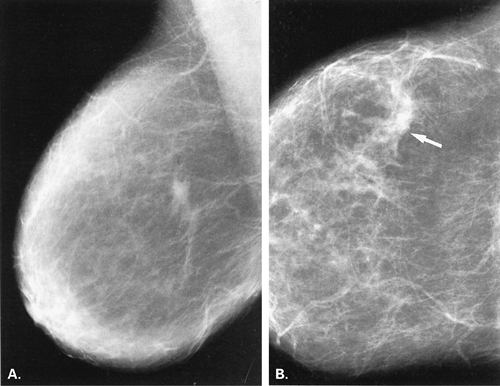
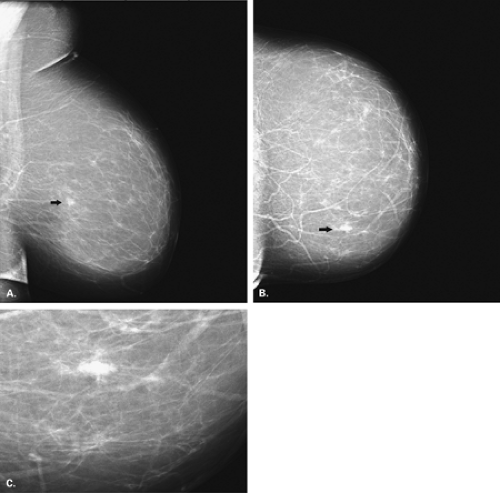
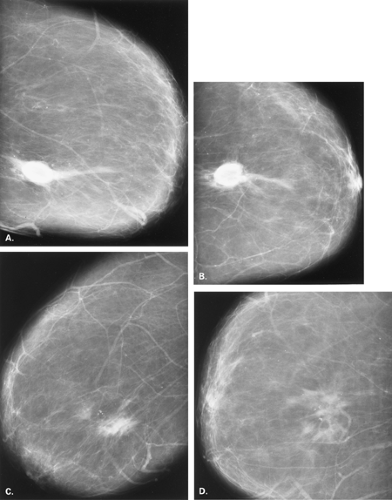 Figure 5.20 HISTORY: A 70-year-old gravida 6, para 6 woman for routine screening. MAMMOGRAPHY: Right ML (A) and CC (B) views and left MLO (C) and CC (D) views. The breasts show fatty replacement. In the 6 o’clock position of the right breast (A and B), there is a high-density mass appearing circumscribed on some margins and indistinct in other areas. Coarse microcalcifications are present in the periphery of this lesion. On the left (C and D) in the 6 o’clock position, there is a poorly defined mass, having a differing shape and density on the two views. Similar coarse calcifications are associated with this lesion. On both sides, but particularly on the left, some of the calcifications are round or ringlike, suggesting fat necrosis as the etiology of these densities. Because there was no definite history of trauma, biopsy was performed. IMPRESSION: Bilateral masses, favoring fat necrosis.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|