Hypothyroidism in Infants and Children: Neonatal Screening
Guy Van Vliet
Johnny Deladoëy
Neonatal Screening
Population-based biochemical screening of newborn infants for congenital hypothyroidism became possible in the 1970s after the development of methods for assaying thyroxine (T4) (1) and thyrotropin (TSH) (2) in blood collected on filter paper. This type of blood sampling had been introduced a decade earlier for the detection of phenylketonuria (3). This procedure has proven to be an important public health breakthrough, because the societal burden of intellectual disability caused by congenital hypothyroidism far exceeds the costs of the screening program (4).
Rationale for Biochemical Screening for Congenital Hypothyroidism
Most infants with congenital hypothyroidism appear normal at birth, and the diagnosis is rarely suspected clinically in the first few weeks of life. At the authors’ institution, only 2 of 300 cases of congenital hypothyroidism diagnosed following biochemical screening were suspected clinically. Yet, it is during the first few weeks and months of life that irreversible brain damage occurs in infants with hypothyroidism who are not treated (5). Before biochemical screening of newborn infants for hypothyroidism was introduced, the mean IQ of children with congenital hypothyroidism was 85 (4), mainly because less than 20% of the affected infants were diagnosed within 3 months after birth; even those with a normal IQ had deficits in fine motor control and learning disabilities (5).
When biochemical screening was implemented, it became clear that the disorder was present at birth, no matter how normal the infant looked. It has now been shown that patients with hypothyroidism treated soon after birth develop, on average, within the normal range (6). In the most severely affected, however, subtle cognitive and health impairments may persist (7,8) (see Chapter 54B).
Biochemical and Clinical Aspects of Screening for Congenital Hypothyroidism
Measurements of Thyroxine and Thyrotropin in Blood
Both T4 and TSH can be measured accurately in blood spotted on filter paper, the standard method for sample collection from newborn infants for screening tests. T4 refers to total T4, because methods to measure free T4 on blood spots are not widely available. In the early days of screening, the greater accuracy of T4 measurements around the cut-off values relative to that of TSH led to T4 being initially measured by a number of programs, with TSH being measured only on the samples with the lowest T4. This T4-first approach misses some infants who have functional disorders or ectopic thyroid tissue and who, under TSH stimulation, produce enough T4 so that the blood T4 concentration is above the cut-off value (9). The primary T4 approach can theoretically detect both central (secondary/tertiary) and primary hypothyroidism (10). However, the former is at least 10-fold less frequent than the latter and can be diagnosed on the basis of the clinical signs and symptoms of associated pituitary hormone deficiencies; furthermore, central hypothyroidism is generally milder than primary hypothyroidism and a T4 below the cut-off was only found in 19% of patients in one study (11). The primary TSH approach has the additional advantage that trends in neonatal TSH distribution can be used to assess changes in iodine status at the population level (see chapter 11D) and has now become the most widely used. Some programs measure T4 as a second step to guide decision-making when the blood-spot TSH value is only slightly elevated; this is the case of the Québec screening program, whose algorithm is shown on Fig. 54A.1.
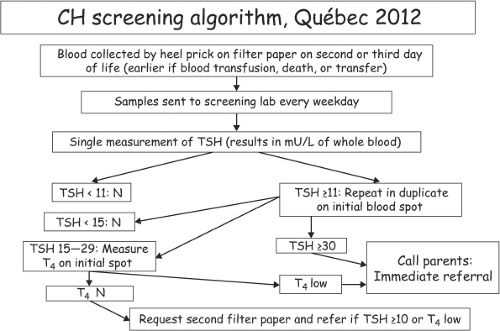 Figure 54A.1 Guidelines for biochemical screening for congenital hypothyroidism used in Québec in 2012. |
It is important to remember that when a disease is subjected to population-based biochemical screening, its prevalence usually increases, sometimes markedly. For congenital hypothyroidism, the birth prevalence has almost tripled, from about 1 in 6,700 newborns by clinical diagnosis to about 1 in 2,500 in the screening era. Further increases in prevalence likely reflect changes in screening algorithms rather than an increase in the true prevalence of the disease (12).
While most screening programs measure T4 or TSH in blood eluted from filter paper and collected a few days after birth, a few use umbilical cord serum (9). One limitation of cord-serum screening is that the likelihood of a falsely normal serum TSH value in the hypothyroid twin of a discordant pair, due to fetal blood mixing, is even higher than on blood spots obtained postnatally (13).
As noted above, screening for congenital hypothyroidism started after screening for phenylketonuria, and this led to the use of the same filter-paper blood spots, which were usually obtained several days after birth. As postnatal hospital stays have shortened, blood sampling has been done sooner after birth. TSH secretion rises abruptly immediately after delivery (see Chapter 53), and, although the surge usually lasts only hours, it results in blood-spot TSH values of 15 mU/L or higher in 2% to 3% of normal infants sampled within 24 hours of birth (9). Therefore, in Québec, infants whose first sample is
obtained within 24 hours after birth are systematically recalled for a second filter paper sample. However, a sample is accepted before 24 hours for infants who die or who are to be transferred to another hospital.
obtained within 24 hours after birth are systematically recalled for a second filter paper sample. However, a sample is accepted before 24 hours for infants who die or who are to be transferred to another hospital.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree