HYPOTHALAMIC–PITUITARY–GONADAL DEVELOPMENT
Part of “CHAPTER 91 – PHYSIOLOGY OF PUBERTY“
FETAL PERIOD
GnRH is present in the hypothalamus and LH and FSH are present in the pituitary, and responsive to GnRH, by 10 weeks of gestation.1 Hypothalamic GnRH and pituitary and plasma LH and FSH levels increase until midgestation, progressively stimulating gonadal maturation and hormone production. After midgestation, hypothalamic GnRH content, pituitary LH and FSH content, and serum FSH levels are greater for several weeks in the female fetus than in the male fetus; this establishes a relative sex difference early and is related to the negative feedback of the testosterone synthesized by the fetal testes. Although fetal testosterone production is necessary for male genital differentiation, whether it causes gender-specific differentiation of the male hypothalamus and pituitary is unclear. For example, adults of both genders are capable of positive feedback gonadotropin release in response to estrogens; therefore, positive feedback in the ovulating female may arise from the hormonal milieu rather than from hypothalamic differentiation. Unlike in male development, ovarian steroidogenesis, although present during fetal life, is unnecessary for female
genital differentiation. Nevertheless, gonadotropin stimulation may be required for normal ovarian development with oocyte and primordial follicle production. Whether estrogen is required for sex-specific differentiation of the female hypothalamus and pituitary is unclear. Observations in humans and animal experiments suggest that gonadal steroids do affect differentiation of the CNS–hypothalamus–pituitary in the fetus and the timing of puberty.5
genital differentiation. Nevertheless, gonadotropin stimulation may be required for normal ovarian development with oocyte and primordial follicle production. Whether estrogen is required for sex-specific differentiation of the female hypothalamus and pituitary is unclear. Observations in humans and animal experiments suggest that gonadal steroids do affect differentiation of the CNS–hypothalamus–pituitary in the fetus and the timing of puberty.5
NEONATAL AND CHILDHOOD PERIOD
Hormonal dynamics during the neonatal period reveal considerable HPG maturation.1 At birth, gonadotropin and sex steroid levels are high, but these levels decline during the first few days. Gonadotropin levels begin to rise again before 1 week of life, suggesting a negative feedback response to the decline in circulating levels of sex steroids originating from the placenta. During the next several weeks, plasma levels of LH and FSH are higher than during the rest of childhood in both sexes (female levels, particularly of FSH, are greater than male levels). Levels of testosterone in males and, less dramatically, levels of estradiol in females are also higher for children at this age than for older children, a finding that suggests pituitary gonadotropin stimulation of gonadal steroidogenesis. These data indicate that gonadotropin secretion, gonadal response with steroid production, and negative feedback mechanisms are all functional at this age. Circulating levels of gonadotropins and sex steroids peak at 2 to 3 months, after which they begin to drop to the low levels that persist for several years.
Inhibin B, the biologically active inhibin among males that appears to be produced primarily by Sertoli cells, also rises to peak levels at ˜3 months. Concentrations gradually fall over the next year or more; thus, the profile is more extended than for LH, FSH, or testosterone. Inhibin B may play a crucial role in seminiferous tubule development at this age.6,7
The fall in these hormone levels cannot be explained simply by an adjustment of the negative feedback mechanism, because a similar pattern with a drop in gonadotropin levels occurs among agonadal children. This phenomenon suggests that gonadotropin secretion is controlled by CNS differentiation and that sex steroid feedback is not an obligatory element in the decreased secretion during childhood. Although gonadotropin levels are lowest during midchildhood, levels usually are not only measurable and not completely suppressed but also indicate episodic release and diurnal (sleepenhanced) variation.2 Furthermore, gender differences persist, with female FSH levels being greater than male levels. Sex steroids, including estradiol,8 and also inhibin may be detectable at very low levels in some children.
PUBERTY
GONADOTROPIN-RELEASING HORMONE AND GONADOTROPINS
As noted, the HPG axis is active beginning early in fetal life. Potentially, the gonad is capable of adult hormonal and germinal function throughout childhood and will respond if stimulated with pubertal or adult levels of gonadotropins. The pituitary in the prepubertal child can also secrete gonadotropin whenever stimulated with GnRH. The pituitary is capable of adult function; thus, the restraint of pubertal maturation lies at the level of GnRH secretion or higher CNS loci. Because the pituitary and gonad are ready to respond, the controlling level is expressed by the magnitude and frequency of GnRH stimulation.
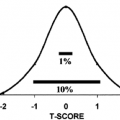
The increasing mean levels of gonadotropins that precede the onset and continue during the progression of puberty result from increased secretion of gonadotropins in an episodic fashion, reflective of episodic GnRH secretion. This change in GnRH stimulation initiates the increased secretion of gonadotropins of puberty. Prepubertal children already have an episodic pattern of gonadotropin release, with infrequent pulses of low amplitude and greater secretion occurring during sleep. As pubertal maturation approaches, the episodic pattern becomes more regular and pulses attain a greater amplitude. This enhanced episodic pattern of puberty initially becomes apparent during sleep, already the time of increased activity during childhood.1,2,9,10,11,12 and 13 Just before the clinical onset of puberty and during early puberty, episodic pulses and mean levels are distinctly higher during sleep than during wakefulness. These changes are more dramatic for LH than FSH, with the relative rise of LH being much greater than that of FSH during puberty. In the mature individual the LH episodic release occurs approximately every 90 minutes, with peak levels persisting for <20 minutes. The increases in FSH above the mean basal levels are less apparent, although episodic release occurs and values are greater during sleep than during waking hours.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree