(1)
Institute of Oncology “Prof. Ion Chiricuță”, Nuclear Medicine & Endocrine Tumors, Cluj-Napoca, Romania
“The eye sees only what the mind is prepared to comprehend”
Henri Bergson (Nobel prize awarded 1859–1941)
11.1 Overview
Positron emission tomography (PET) is a tomographic technique that computes the three-dimensional distribution of radioactivity based on the annihilation photons that are emitted by positron emitter-labeled radiotracers. The use of PET/CT fusion scanners has been demonstrated to significantly increase accuracy of lesion detection, combining the high anatomical definition of CT with the high sensitivity of PET. Advanced functional MR imaging techniques such as DW imaging, MR spectroscopy, and perfusion-weighted imaging used with PET can further enhance detection and characterization of malignant lesions for prognosis assessment, biopsy and pretreatment planning, patient selection for certain therapeutic agents, and response prediction and assessment. PET allows noninvasive quantitative assessment of biochemical and functional processes. The most commonly used tracer at present is the glucose analogue F18-FDG (F18-fluoro-2-deoxy-d-glucose). F18-FDG accumulation in the tissue is proportional to the amount of glucose utilization. Increased consumption of glucose is a characteristic of most cancers and is in part related to the overexpression of the GLUT-1 glucose transporters and increased hexokinase activity. The PET radiotracer F18-FDG has obtained a large acceptance in clinical oncology due to its excellent diagnostic performance in many cancers such as lung, colorectal, lymphoma, melanoma, esophagus, pancreas, breast, ovary, and testicle. However, F18-FDG has reduced performance in some other cancers, less aggressive and most differentiated ones, such as prostate cancer or endocrine tumors. In these cancers, it is mandatory to perform PET with tracers “beyond F18-FDG,” specific tracers with particular structure analogue with the examined organ or tumor.
The main indications of PET/CT examinations are:
- 1.
Diagnosis of the primary site of the tumors:
Unknown primary malignancy
Differentiation of benign/malignant lesions, for example, a solitary lung nodule
- 2.
Staging on presentation: non-small-cell lung cancer, esophageal cancer, Hodgkin disease, non-Hodgkin lymphoma, locally advanced cervical cancer, neuroendocrine tumors with risk factors, and locally advanced breast cancer
- 3.
Response evaluation to treatment
- 4.
Restaging in the event of potentially curable relapse (for F18-FDG avid tumors)
- 5.
Establishing and localizing disease sites as a cause for elevated serum markers (e.g., colorectal, thyroid, ovarian, cervix, melanoma, breast, and germ cell tumors)
- 6.
Image-guided biopsy (e.g., brain tumors) and radiotherapy planning
The most important differences of SPECT-PET might be summarized as follows:
SPECT has a lower resolution and sensitivity.
Different radiotracers are used in PET, which are positron emitters.
The presence of collimators in SPECT reduces significantly the efficiency of the detection.
Both techniques by fusing with CT increase the effective dose of the body, due to irradiation. The CT component contributes 54–81% of the total combined dose, a fact that leads to a new concept of low-dose CT or so-called localization CT. In this case the parameters used during the CT acquisition are modulated to the lowest efficient level, the aim being for localization of the metabolic process detected by PET and not the highly sensitive diagnosis. It was demonstrated that by decreasing one CT parameter (kV) from 140 to 80 kV, the total measured dose is reduced with 67% (Fahy 2009).
The latest years brought impressive achievements in the field of hybrid imaging. The results of multicenter trials and studies were published in the last 2–3 years, and after 15 years, since the method was introduced in the clinical practice, the impact of PET/CT is considered essential:
PET/CT changes from an intended nontreatment to a treatment plan, in 28.3% of cases.
8.2% of cases changed from treatment to nontreatment.
A major change in intended management occurred in 30.3–39.7% depending on the indication.
Overall, physicians changed their intended treatment plan in 36.5% of cases after PET/CT.
In the present chapter, the focus will be mainly on PET/CT; the new technique of PET/MRI is still not on large, and routine availability and the indication in endocrinology are limited. Table 11.1 is presenting the main advantages and disadvantages of one method over the other one.
Table 11.1
PET/CT and PET/MRI strengths and weaknesses
PET/CT | PET/MRI | |
|---|---|---|
Strengths | • Lung and compact bone imaging • Attenuation correction | • Brain and bone marrow imaging • Excellent soft tissue contrast • Lesser radiation dose from MRI • Simultaneous multimodality preclinical imaging • Plenty of tracers available for PET • Enables good visualization, quantification, and translational studies |
Weaknesses | • Brain and soft tissue imaging • Metal artifacts • Higher radiation dose due to CT | • Lung and compact bone imaging • Attenuation correction • It requires high initial capital cost • There is lack of protocol and standardization due to huge variations in MR protocols • No combined reporting of PET and MR components • Limited flexibility of combined PET/MR systems • High acquisition times of up to 60 min |
In the majority of endocrine diseases, except pituitary pathology, MRI is better than CT imaging, but PET/MR seems to be equal to PET/CT, all lesions seen on PET are also seen on MR, and information is redundant. Great strides have been made to solve technical inadequacies of PET/MR in the last 5 years, and the task is to define reasonable PET/MR imaging protocols mainly in oncology, “rule out metastases” protocols (brain, liver), and neurology “rule out other pathologies” protocols (Gustav K. von Schulthess, Zurich).
With respect to endocrine pathologies, the role of PET/MR is still undefined, limited experience being achieved all around the world, considering that the first commercial whole-body system used in humans was in 2010. The following chapter will focus on PET/CT imaging, based on authors’ experience in this field.
The main indications of PET/CT in endocrinology are as follows:
Detection of radiological occult lesion
Characterization of the functional, metabolic behavior of the detected lesion
Staging
Evaluation of treatment response
Evaluation of prognosis in endocrine malignant diseases
11.2 PET/CT F18-FDG
Radiopharmaceutical:
F18-fluorodeoxyglucose (F18-FDG)
Principle:
F18-FDG accumulation in tissue is proportional to the amount of glucose utilization. The malignant tissues are highly glucose consuming. F18-FDG is proportionally trapped with the intensity of the glucose metabolism and vascularization, so it is an excellent imaging marker of the aggressiveness of the disease.
Technique:
Patient preparation: the main purpose of the patient preparation is the reduction of tracer uptake in normal tissue (kidneys, bladder, skeletal muscle, myocardium, brown fat, digestive tract) while maintaining and optimizing tracer uptake in the target structures (tumor tissue).
Patients are not allowed to consume any food or sugar for at least 6 h prior to the start of the PET study.
Medication can be taken as prescribed.
Adequate prehydration is important to ensure a sufficiently low FDG concentration in urine and for radiation safety reasons.
Parental nutrition and intravenous fluids containing glucose should be discontinued at least 4 h before the PET/CT examination. In addition, the infusion used to administer intravenous prehydration must not contain any glucose.
During the injection of FDG and the subsequent uptake phase, the patient should remain seated or recumbent and silent to minimize FDG uptake in muscles.
The patient should be kept warm starting at 30–60 min before the injection of FDG and throughout the following uptake period and PET examination to minimize FDG accumulation in the brown fat (especially relevant if the room is air-conditioned). Moreover, all patients must avoid (extreme) exercise for at least 6 h before the PET study.
Patients with diabetes mellitus type II (controlled by oral medication) should take their medication and be in fasting condition. Special condition is metformin that should be changed 2–4 days prior to the examination in order to avoid its high uptake in the bowel.
In patients having type I diabetes mellitus and insulin-dependent type II diabetes mellitus, ideally, an attempt should be made to achieve normal glycemic values prior to the PET study.
The blood glucose level of the patient is checked before starting any procedure.
Essential information should be given prior to scheduling the test: last surgical intervention, recent radiotherapy, chemotherapy, administration of growth factors, etc. (minimum of 10 days after the last cycle).
Dose: the dose is calculated depending on the weight of the patient and the type of the instrument used and the protocol:
5 MBq/kg body weight dose, which may vary according to the mentioned data
Dose calibration.
Injected I.V.
It is necessary to wait 60 min after injection.
Patient position: supine.
Acquisition: specific parameters of PET and CT according to producers.
The CT parameters should be adjusted for every patient, in order to achieve the maximum benefit from a low-dose CT with minimum irradiation (decrease accordingly the kV and mA).
Processing:
Both uncorrected and attenuation-corrected images need to be assessed in order to identify any artifacts caused by contrast agents, metal implants, and/or patient motion.
Criteria for visual analysis must be defined for each study protocol.
SUV is a measurement of the uptake in a tumor normalized on the basis of a distribution volume.
It is calculated as follows:
SUV = activity in tumor volume (MBq/mL)/activity administered (MBq/body weight); there are a multitude of other types of SUV considering the glucose level, the body surface, min, mean, max, etc.
Necessary additional examinations:
Clinical examination: remember to discuss and to examine the patient before the injection in order to limit the hazardous radiation exposure.
Because this examination occurs frequently after performing the conventional imaging tests, it is important to have the results for data corroboration.
Comparison with previous examinations should be part of the PET/CT report. PET/CT examinations are more valuable if they are interpreted in the context of results of other imaging examinations (e.g., CT, PET, PET/CT, MRI) and relevant clinical data. If a PET/CT examination is performed in the context of the assessment of response to a therapy, the extent and the intensity of the FDG uptake should be documented. The European Organization for Research and Treatment of Cancer (EORTC) has published the criteria for the assessment of therapy response with FDG as metabolic marker. At present, relative changes in SUV under therapy represent the most robust parameter.
Comments:
The place of PET/CT in the assessment of malignant diseases is well established by the international algorithms of diagnostic and treatment in order to obtain the maximum benefit with reduced risks.
Reports:
The reports respect the general format of the department with all the identification data of the patient, the institution, and the physician.
The description of the localization, the extent, and the intensity of pathologic FDG accumulations related to normal tissue, the description of relevant findings in CT, and their relation to pathologic FDG accumulations.
FDG accumulation should be reported as mild, moderate, or intense and compared to the background uptake. However, the criteria for visual interpretation must be defined for each study protocol and/or type of cancer because they may differ for different tumor locations and types.
If possible, a definite diagnosis should be stated whenever possible. Alternatively, an estimate of the probability of a diagnosis should be given.
If relevant, differential diagnoses should be discussed.
If appropriate, repeat examinations and/or additional examinations should be recommended to clarify or confirm findings.
11.3 PET/CT F18-FCH
Radiopharmaceutical:
F18-fluorocholine (F18-FCH)
Principle:
F18-choline is an essential component for the formation of new cell membrane components, and the current understanding is that malignancy-induced upregulation of choline kinase leads to the incorporation and trapping of choline in the tumor cell membrane.
Technique:
Patient preparation: no special requirements
Dose: the dose is calculated depending on the weight of the patient and the type of the PET/CT equipment used and the protocol:
FCH 3 MBq/kg of body mass, which may vary according to the mentioned data
Dose calibration
Injected I.V.
Low-dose CT (100–120 kV, 30–50–80 mA) acquired first.
Subsequently, with the patient staying inside the tunnel of the PET/CT camera, the FCH dose is administrated intravenously in an infusion line connected to saline.
Immediately after injection, PET dynamic acquisition is performed during 10 min with the detector ring centered on the neck, immediately followed by a “static” PET acquisition (2 min per bed position) ranging from the skull to mid-thighs for men (in order not to miss potential prostate foci) and to the lower limit of the liver for women.
Dynamic images may be reframed by summing up images from the second to the eighth minute to facilitate interpretation.
Processing:
Both uncorrected and attenuation-corrected images need to be assessed in order to identify any artifacts caused by contrast agents, metal implants, and/or patient motion.
Criteria for visual analysis must be defined for each study protocol.
SUV is a measurement of the uptake in a tumor normalized on the basis of a distribution volume. The type of SUV should be defined and reported by the laboratory (SUVbsa, lbm, bw, min, max, mean, etc.).
Necessary additional examinations:
Clinical examination: remember to discuss and to examine the patient before the injection in order to limit the hazardous radiation exposure.
The positive diagnosis frequently refers to the recurrence of the hyperparathyroidism and to the surgical options. Comparison with previous examinations should be part of the PET/CT report. PET/CT examinations are more valuable if they are interpreted in the context of results of other imaging examinations (US, Tc-99m MIBI scan, etc.) and relevant clinical data.
Comments:
The examination is not the first-line option, all studies trying to compare the results with the gold standard method of Tc-99m MIBI.
Reports:
The reports respect the general format of the department with all the identification data of the patient, the institution, and the physician.
The description of the localization of parathyroid adenoma, if it is in normal or ectopic position, its relation to thyroid, and previous surgery.
The quantification of uptake in case of F18-FCH used for HPT is less important.
11.4 PET/CT Ga-68 DOTATOC/DOTANOC/DOTATATE (Ga-68 SSTR)
Radiopharmaceutical:
DOTA (tetraazacyclododecane-tetraacetic acid):
Ga-68 DOTATOC: Ga-68 DOTA-Phe1-Tyr3-Octreotide
Ga-68 DOTANOC: Ga-68 DOTA-Nal3-Octreotide
Ga-68 DOTATATE: Ga-68 DOTA-Thy3-Thre8-Octreotide (octreotate)
Principle:
Ga-68 SSTR F18-choline is an essential component for the formation of new cell membrane components, and the current understanding is that malignancy-induced upregulation of choline kinase leads to the incorporation and trapping of choline in the tumor cell membrane.
Technique:
Patient preparation:
Discontinuation of somatostatin analogue treatment before PET/CT is desired but not mandatory and has been shown not to influence results.
Fasting is not required.
Dose:
The recommended dose of Ga-68 SSTR is usually 132–222 MBq (4–6 mCi), but should not be less than 100 MBq.
Dose calibration.
Injected I.V.
Acquisition:
CT is acquired first using low-dose CT protocol (120 kV, 30–50–80 mA).
PET/CT is acquired 45–60 min postinjection, with the general consensus that best images are obtained at 60 min.
Images are acquired from the skull (must include the pituitary gland) to mid-thigh.
Additional views can be taken as and when required.
Use of intravenous contrast during CT part of PET/CT is controversial, with few studies advocating their use.
Processing:
The images are reconstructed using iterative reconstruction using standard protocols.
Both uncorrected and attenuation-corrected images need to be assessed in order to identify any artifacts caused by contrast agents, metal implants, and/or patient motion.
Criteria for visual analysis must be defined for each study protocol.
SUV is a measurement of the uptake in a tumor normalized on the basis of a distribution volume.
Necessary additional examinations:
Clinical examination: remember to discuss and to examine the patient before the injection in order to limit the hazardous radiation exposure.
Frequently, these examinations are not in the first line, so patients already have CT, MRI, and even other functional tests, like I-123/I-131 MIBG, SRS, and F18-FDG PET/CT. The positive diagnosis refers to staging and affinity for these tracers; during follow-up, if PRRT is done, the results should mention the assessment of therapy response.
Comments:
Despite different affinities, there is currently no evidence of a clinical impact of these differences in SSTR binding affinity, and therefore no preferential use of one compound over the others can be advised.
Reports:
The reports respect the general format of the department with all the identification data of the patient, the institution, and the physician.
The description of the localization of pathologic uptake.
The quantification of uptake should be done and reported.
11.5 PET/CT and PET/MR in Pituitary Gland Pathology
Pituitary tumors are the most common pituitary disorder. However, they are not, in the great majority of cases, life-threatening. Pituitary tumors can disrupt the gland’s normal ability to release hormones and also, by local invasion, produce cerebral effects. There are two types of pituitary tumors—secretory and nonsecretory. These hormonal imbalances can cause problems in many different areas of the body. The “gold standard” of diagnosis is pituitary MRI. Nowadays, by increasing the indication of PET/CT in different oncology areas, the incidental pathological findings in the pituitary gland became more frequent.
Incidental pituitary uptake on whole-body F18-FDG PET/CT was studied in a multicenter study, published by Jeong et al. in 2010. Focally increased pituitary F18-FDG uptake on PET/CT was found in 30 of 40,967 patients, accounting for an incidence of 0.073%. The conclusion of the study was that incidental pituitary F18-FDG uptake was a very rare finding. Cases with incidental pituitary F18-FDG uptake were diagnosed primarily with clinically nonfunctioning adenomas, and there were also a few functioning adenomas. Further evaluations, including hormone assays and pituitary MRI, are warranted when pituitary uptake is found on F18-FDG PET/CT.
The most frequent diseases that might affect pituitary gland in their evolution are breast and lung cancers, colonic cancer, less common non-Hodgkin lymphoma and malignant melanoma, or thyroid carcinoma. The most common symptom seems to be diabetes insipidus, reflecting a predominance of metastasis to the posterior lobe. Komninos et al. (2004) cited in their review a study of 40 symptomatic cases, where diabetes insipidus occurred in 70%, whereas only 15% had one or more anterior pituitary deficiencies.
The role of PET/CT F18-FDG in pituitary gland is related to a correct assessment of the primary tumor, knowing and considering that this gland might be affected during the metastatic process (Fig. 11.1).
Fig. 11.1
PET/CT F18-FDG (a) transversal slice of CT, (b) transversal slice of PET and (c) transversal slice of fused PET/CT showing an increased, pathologic uptake in the pituitary gland, in a case of metastatic breast cancer
PET/MR has a special role in the diagnosis and evaluation of pituitary gland, mainly in malignant metastatic diseases, due to its better sensitivity and lesser radiation dose, with brain and cardiology being until now the main indications of this hybrid imaging. Figure 11.2 is presenting a case of pituitary adenoma visualized in PET/MR with somatostatin analogue tracer (Ga-68 DOTATOC).
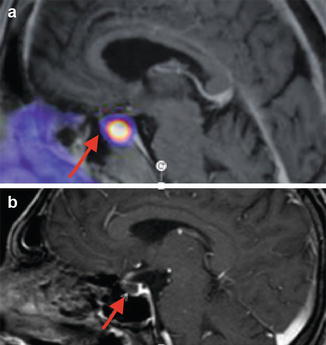
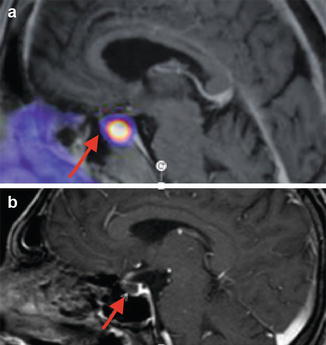
Fig. 11.2
PET/MR Ga-68 DOTATOC ((a) sagittal slice) and MR ((b) sagittal slice) showing an increased uptake in the pituitary gland, normally being visualized due to its somatostatin receptors; in this case is a pituitary adenoma
11.6 PET/CT in Parathyroid Gland Pathology
The place of parathyroid scintigraphy in the assessment of hyperparathyroidism is being largely presented in Chap. 8; the use of SPECT/CT improved specificity, but unfortunately could not improve importantly sensitivity. The most challenging clinical issue is the association of multinodular goiter with primary hyperparathyroidism due to parathyroid adenoma; researchers worldwide trying to find one modality were able to depict optimally the two entities. Many studies were carried on trying to find the best imaging method and protocol, but until now, beyond Tc-99m MIBI scan, all other methods need to be compared with it.
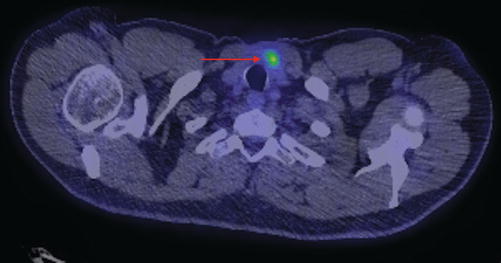
In this light, PET/CT introduced, in the last years, a new tracer: F18-fluorocholine (F18-FCH), with some promising results (Fig. 11.3). First description of F18-fluorocholine uptake in hyperfunctioning parathyroid glands was in 2013. The indications of the method consist in:
Diagnosis of primary HPT
Indication for parathyroid surgery
US and SPECT nondiagnostic/inconclusive
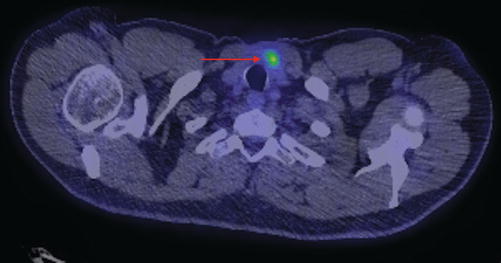
Fig. 11.3
PET/CT F18-FCH (transversal slice) showing an increased, pathologic uptake in a right parathyroid adenoma
Some pilot studies already published that in patients with hyperparathyroidism and with discordant or equivocal results on scintigraphy or on ultrasonography, adenomatous or hyperplastic parathyroid glands can be localized by F18-FCH PET/CT with good accuracy. One pilot study (Michaud et al. 2014) confirmed that F18-FCH PET/CT is an adequate imaging tool in patients with primary or secondary hyperparathyroidism, since both adenomas and hyperplastic parathyroid glands can be detected. The authors underlined that the sensitivity of F18-FCH PET/CT was better than that of US and similar to that of dual-phase dual-isotope I-123/Tc-99m scintigraphy. Unfortunately, the study involved a limited number of patients, 12 patients, so the conclusions are not strong enough to affirm the method. Considering Tc-99m MIBI scan as “gold standard,” further studies should evaluate whether F18-FCH could replace this one as the functional agent for parathyroid imaging (Michaud et al. 2015).
Similar, the introduction of F18-FCH PET/MRI should bring better data, especially in case of HPT associated with multinodular goiter.
11.7 PET/CT in Thyroid Pathology
Among all the endocrine malignancies, the thyroid carcinoma is the most frequent, accounting for about 5% of thyroid nodules and being responsible for the mortality caused by cancer in 0.12–1.2% of cases. The differentiated thyroid cancer forms represent about 80–90% of all thyroid cancers, with a good prognosis and with a very specific treatment strategy based on surgery and radioiodine therapy.
In the last decade, more aggressive natural history of this cancer was reported, and new investigation methods were developed. The metabolic F18-fluoro-2-deoxy-d-glucose has already been accepted as an essential tool in staging, restaging, and therapy response assessment of many tumors.
The PET/CT investigation in the thyroid pathology is related to three major subjects:
- 1.
The evaluation of thyroid nodules
- 2.
The role of PET/CT in different forms of thyroid carcinoma
- 3.
The diagnosis of other malignancies associated with thyroid carcinomas
11.7.1 PET/CT in the Differential Diagnosis of Benign Thyroid Nodules and Malignant Thyroid Nodules
Normally, there is no significant F18-fluoro-2-deoxy-d-glucose uptake in the thyroid bed. The presence of this radiotracer in the area of the thyroid in a PET/CT examination indicated for another type of pathology is described in literature as “metabolom.” If focal F18-FDG uptake is described on a PET/CT image, it is important to refer the patient to the endocrinologist in order to make a clinical examination, thyroid function tests, and thyroid ultrasound.
The study of Seong et al. published in September 2009 regarding the incidental thyroid lesions detected by F18-FDG PET/CT demonstrated that prevalence and risk of thyroid cancer in these lesions are very low. F18-FDG PET/CT was performed on 3379 patients for evaluation of suspected or known cancer or cancer screening without any history of thyroid cancer. Among them, 285 patients (8.4%) were identified to have F18-FDG uptake on thyroid area, 99 patients with focal or diffuse F18-FDG uptake underwent further evaluation, and 22 patients were diagnosed with thyroid cancer. The cancer risk of incidentally found thyroid lesions on F18-FDG PET/CT was 0.65% (22/3379), a fact that underlines that this examination is not recommended as screening of thyroid carcinoma.
Regarding the differential diagnosis between the benign and malignant nodules, there is a factor that may play a role in the decision of further thyroid evaluation after the discovery of a “metabolom”: there is a significant difference in the standardized uptake value (SUV) between the benign and malignant nodules (3.35 ± 1.69 vs 6.64 ± 4.12). If SUV maximum is suspicious, an examination in the endocrinology department is indicated.
Soelberg et al. published in 2012 a very important and consistent study referring to the evaluation of thyroid carcinomas discovered incidentally in patients or healthy volunteers by F18-FDG PET systematically searched in the PubMed database from 2000 to 2011. There were 22 studies comprising a total of 125,754 subjects. Of these, 1994 (1.6%) had unexpected focal hypermetabolic activity; a diagnosis was assigned in 1051 of the 1994 patients with a focal uptake, 366 of whom (34.8%) had thyroid malignancy. In the eight studies reporting individual maximum SUV, the mean SUV(max) was 4.8 ± 3.1 in benign lesions and 6.9 ± 4.7 in malignant lesions.
Considering the above studies, a cutoff value of SUVmax of 6 is highly suspicious for malignancy in a case of focal thyroid F18-FDG uptake in PET/CT (Fig. 11.4).
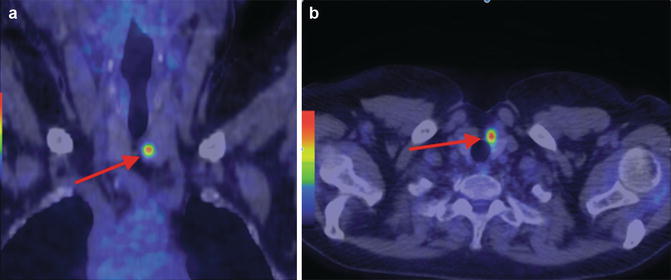
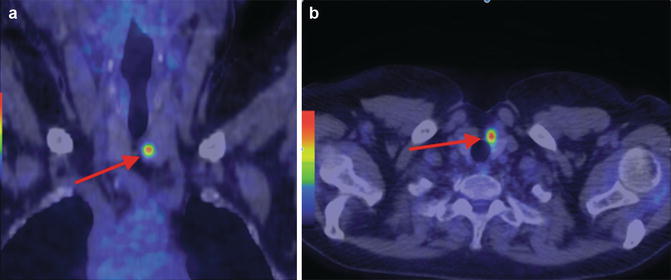
Fig. 11.4
F18-FDG PET/CT showing incidental focal uptake in the left thyroid lobe, in a patient performing the examination during the monitoring protocol for a malignant melanoma ((a) coronal slice; (b) transversal slice). The patient was operated and the histological specimen confirmed a papillary thyroid carcinoma
In case of diffuse thyroid uptake, the malignancy is less probable and the diagnosis of thyroiditis should be mentioned (Fig. 11.5).
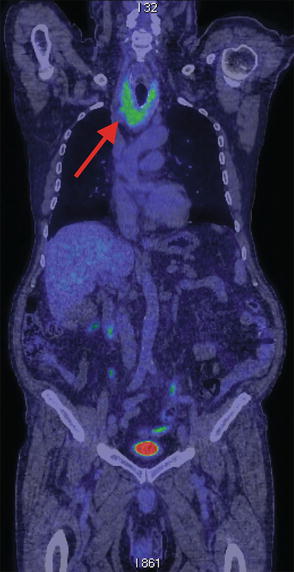
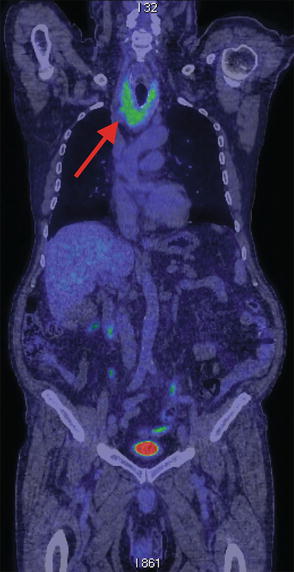
Fig. 11.5
F18-FDG PET/CT showing incidental diffuse uptake in the thyroid gland, in a patient performing the examination for a restaging of a colon cancer (coronal slice); the image is highly suggestive for chronic Hashimoto’s thyroiditis
The evaluation of thyroid gland in case of F18-FDG PET/CT performed for other oncological clinical cases is important to be mentioned, both with respect to possible synchronous neoplasia and in order to exclude possible metastases in thyroid.
A nodular goiter with no F18-FDG uptake discovered in a patient with a primary known cancer is essential to be pointed. Figure 11.6 is presenting a case of breast cancer with incidental nodular goiter discovered at PET/CT with no F18-FDG uptake, being highly probable to be a benign thyroid pathology, with no impact in the assessment of the primary cancer (Fig. 11.6). Similarly, in a case of colon cancer, with nodular goiter, without FDG uptake in PET/CT is presented in Fig. 11.7.
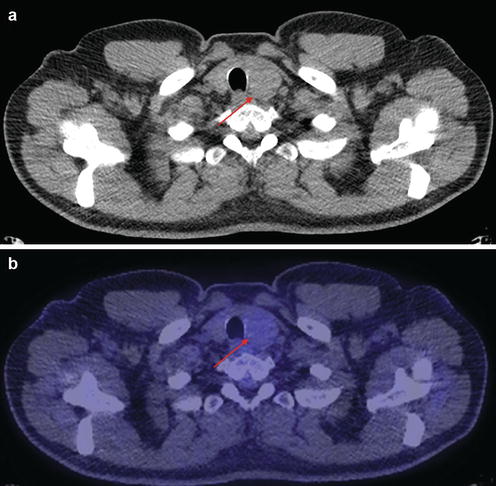
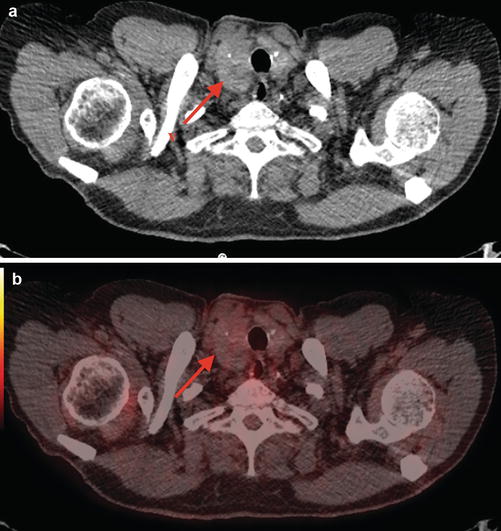
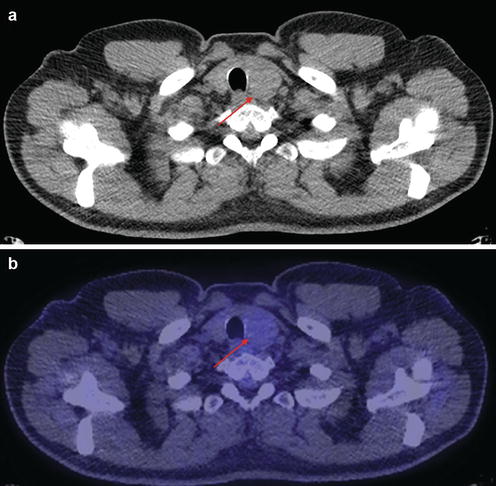
Fig. 11.6
F18-FDG PET/CT in a patient with breast cancer showing incidental nodule in the left lobe of the thyroid gland, with no F18-FDG uptake, being highly probable to be a benign nodule ((a) CT transversal slice; (b) PET/CT transversal slice)
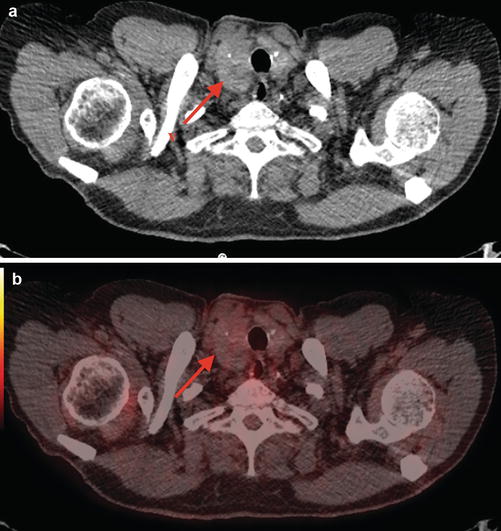
Fig. 11.7
F18-FDG PET/CT in a patient with colon cancer showing multinodular goiter, with no pathologic F18-FDG uptake, being highly probable to be a benign macronodular goiter ((a) CT transversal slice; (b) PET/CT transversal slice)
Thyroid incidentaloma is commonly defined as a thyroid uptake incidentally and newly detected by imaging techniques performed for an unrelated and non-thyroid purpose. Its management is challenging for referring clinicians and for nuclear medicine physicians because it needs further investigation to clarify its nature. The overall reported incidence of F18-FDG PET or PET/CT thyroid incidentalomas varies from 0.2 to 8.9%, whereas the prevalence of thyroid cancer in these incidental lesions ranges from 8 to 64%, and the most significant conclusions regarding this issue are summarized as follows (Bertagna et al. 2012):
- 1.
Thyroid incidentalomas are relatively frequent, ranging from 0.2 to 8.9%, and the pooled incidence is 2.46%.
- 2.
Diffuse uptakes are commonly benign.
- 3.
Most focal uptakes are benign, but about one-third of focal uptakes are malignant.
- 4.
All thyroid incidentalomas need further investigation and clinical evaluation.
- 5.
The most frequent malignant histological type responsible for F18-FDG PET/CT thyroid incidentaloma is PTC.
- 6.
There is no safe SUV cutoff over which it is certain or reasonably safe to suspect or rule out malignancies.
The workup for an incidentally increased thyroid uptake of F18-FDG in PET/CT is presented in Fig. 11.8.
Fig. 11.8
The workup for an increased thyroid uptake of F18-FDG in PET/CT
11.7.2 PET/CT in the Follow-Up of Thyroid Carcinoma
In case of thyroid carcinoma, the experience regarding the use of hybrid imaging shows an increasing role and a very well-defined place of PET/CT. The changes in the behavior and aggressiveness of thyroid cancer represent an important indication for F18-FDG PET/CT. The most important situations, where the hybrid method brings essential information, are:
Biochemical evolution of the disease, with no clinical and imaging signs
Increasing serological tumor markers, negative WBS I-131
Radioiodine-refractory differentiated thyroid cancer (DTC)
Aggressive course of the disease
Progressive disease in medullary thyroid cancer (MTC)
Anaplastic thyroid cancer (ATC)
Thyroid lymphoma
Association with other malignancies
11.7.2.1 PET/CT in the Follow-Up of Differentiated Thyroid Carcinoma (DTC)
DTC is not one of the types of cancers where PET/CT is a standard indication or is included in the guidelines of diagnosis and treatment. Despite that, there is a very well-defined situation where PET/CT plays a major role, so-called TENIS (Tg elevated and negative I-131 scan) syndrome:
Confirmed DTC with radical treatment
Detectable serum Tg or dynamic rising of Tg and/or anti-Tg
WBS I-131 negative
The American Thyroid Association affirms in the guidelines of thyroid cancer in 2009 (ATA 2009): “if after an empiric dose of 100–200 mCi, I-131 WBS fails to localize the tumor, especially in patients with unstimulated serum Tg level of 10–20 ng/mL, F18-FDG-PET should be considered.”
The same recommendation is given by the National Comprehensive Cancer Network (NCCN 2016) on thyroid cancer guidelines in 2011. From 2003, the insurance system (Medicare) from the USA pays for this condition of thyroid cancer patients who have the indication for this examination and also in most of the European countries.
The recent guidelines (ATA 2015; BTA 2014; ETA/ESMO and NCCN 2016) introduced precisely the indication and the place of PET/CT in the management of thyroid cancers.
ATA (2015)
Recommendation 68
A, strong recommendation
F18-FDG PET scanning should be considered in high-risk DTC patients with elevated serum Tg (generally >10 ng/mL) with negative WBS I-131 imaging; according to multiple studies published recently, the sensitivity of the method was 83% (ranging from 50% to 100%), and the specificity was 84% (ranging from 42% to 100%) in non-131I-avid DTC.
B, weak recommendation
A part of initial staging in poorly differentiated thyroid cancers and invasive Hurthle cell carcinomas, especially those with other evidence of disease on imaging or because of elevated serum Tg levels
A prognostic tool in patients with metastatic disease to identify lesions and patients at highest risk for rapid disease progression and disease-specific mortality
An evaluation of posttreatment response following systemic or local therapy of metastatic or locally invasive disease
BTA (2014)
In case of TENIS syndrome, BTA guidelines recommend:
Chest CT without contrast.
F18-FDG PET/CT.
Neck MRI.
CT.
Spine MRI.
Bone scan.
I-131 WBS.
Very occasionally In-11 octreotide or Ga-68 DOTATATE PET/CT may be positive.
Positive F18-FDG PET/CT indicates histologic transformation from low- to high-risk poor prognosis tumors, as F18-FDG uptake reflects dedifferentiation.
Patients with positive F18-FDG PET/CT scan have been shown to have a markedly reduced 3-year survival compared with F18-FDG PET/CT scan-negative patients. If PET imaging is positive, I-131 imaging is typically negative and the patient is I-131 refractory.
The most frequent situation of indication for F18-FDG PET/CT in DTC consisted in:
Radical treatment of DTC: surgery, radioiodine therapy, and suppressive hormonal treatment
No clinical signs of disease
Dynamic rising of serum level of Tg or/and anti-Tg
WBS I-131 negative
Neck ultrasound negative or doubtful
Conventional imaging negative (thorax radiographies, cervical and mediastinum computed tomography)
No other acute or chronic severe diseases that may lower life expectancy under 1 year
Financial support available, where the examination is not reimbursed by national health insurances
The F18-FDG PET/CT is indicated with respect to a minimum level of serum Tg above 2 ng/mL if all previous mentioned criteria are fulfilled; also it is important to have demonstrated that in the same conditions of sample analysis, in two consecutive determinations at 6-month interval, there was a significant dynamic rising of the value of Tg.
Regarding the F18-FDG PET/CT in DTC, there is a special detail that is important to be stressed: the role of TSH in the F18-FDG uptake. The elevated TSH serum level (withdrawal of thyroid hormonal treatment or using the rhTSH) influences the F18-FDG uptake. Petrich et al. published in 2002 that the sensitivity of FDG PET was 53% during TSH suppression and 87% following rhTSH stimulation. Other authors showed that there is no influence of TSH in F18-FDG uptake, but the higher sensitivity is seen on Tg value >20 ng/mL.
Iagaru A et al. (2007) published that F18-FDG PET/CT had excellent sensitivity (88.6%) and specificity (89.3%) in this patient population. Metastatic lesions were reliably identified but were less F18-FDG avid than recurrence/residual disease in the thyroid bed. TSH levels at the time of PET/CT did not appear to impact the FDG uptake in the lesions or have the ability to detect disease. In the setting of high or rising levels of Tg, their study confirms that it is indicated to include PET/CT in the management of patients with differentiated thyroid cancer; ATA 2015 set the cutoff value at 10 ng/mL.
According to BTA 2014, thyroid hormone withdrawal (THW) or recombinant human TSH (rhTSH) administration has been shown to increase the sensitivity of F18-FDG PET/CT scan; this issue recently was amended by other authors, being clearly demonstrated that is related to the level of Tg. So, the level of Tg, no matter if in understimulated condition or not, is recommended to be >10 ng/mL in order to have the maximum sensitivity of PET/CT F18-FDG in DTC.
If in the previous edition of this book, this issue was debatable, to date, there is no evidence that TSH stimulation improves the prognostic value of F18-FDG PET imaging. Singh et al. published in 2017 the results of their study, and they underline a significant association of SUV with thyroglobulin (Tg) level (P = 0.035) but not with thyroid-stimulating hormone (TSH) level (P = 0.85).
As a commentary, from the personal experience of the author, the level of Tg is less important than the aggressiveness of the histology: very low detectable levels of Tg, even <5 ng/mL, may lead to a severe positive scan in F18-FDG PET/CT, if the course of the disease is highly aggressive (see examples in the clinical cases presented below).
Iodine 124 emits positrons, allowing PET/CT imaging in DTC patients. It is used as a dosimetric and also as a diagnostic tool to localize disease. I-124 PET/CT permits an accurate measurement of the volume and uptake in positive lesions on the scan, allowing a reliable individual dosimetric assessment for each neoplastic focus.
The sensitivity of I-124 PET for the detection of residual thyroid tissue and/or metastatic DTC was reported to be higher than that of a diagnostic I-131 planar WBS, but is not yet widely available for clinical use and is primarily a research tool at this time.
11.7.2.2 PET/CT in the Follow-Up of Medullary Thyroid Carcinoma (MTC)
As in DTC situation in MTC, there is a strict place of F18-FDG PET/CT: radical treatment, serum calcitonin level rising, and conventional imagery negative. The overall sensitivity of F18-FDG PET/CT is less than 75%, but the new radiotracers such as F18-dihydroxyphenylalanine, F18-DOPA, and Ga-68-labeled somatostatin analogues give optimistic horizons. As is known in literature, in MTC, there is a lack of sensitivity of many investigations: F18-fluoro-2-deoxy-d-glucose PET/CT, 78%; pentavalent Tc-99m dimercaptosuccinic acid (DMSA), 33%; Tc-99m sestamibi (MIBI), 25%; indium-111 pentetreotide, 25%; CT, 50%; and MRI, 82%. Even if the specificity may raise to 100% (MIBI), these low rates of sensitivity justify the efforts to develop new radiotracers for PET. Recent studies (Giraudet et al. 2016) established that PET/CT using F18-FDOPA is the most sensitive radiopharmaceutical for localizing persistent/recurrent MTC, its sensitivity being related to a threshold value serum calcitonin of around 150 pg/mL. The authors recommend F18-FDG PET/CT in MTC when there is a short calcitonin or CEA doubling time; this underlines the aggressiveness of the disease (Fig. 11.9). Same results were published also by Archier et al. in 2016: F18-DOPA PET/CT enables early diagnosis of a significant number of patients with distant metastases. It has a limited sensitivity in the detection of residual disease but provides high performance for regional analysis.
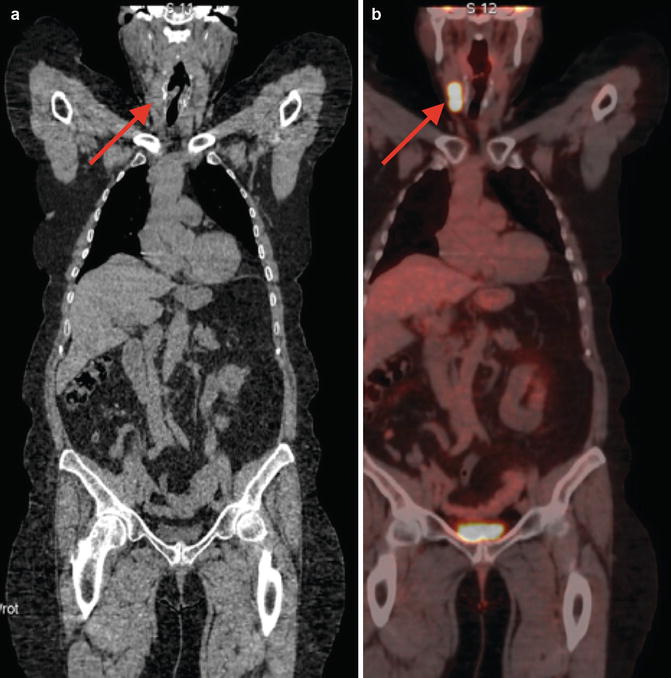
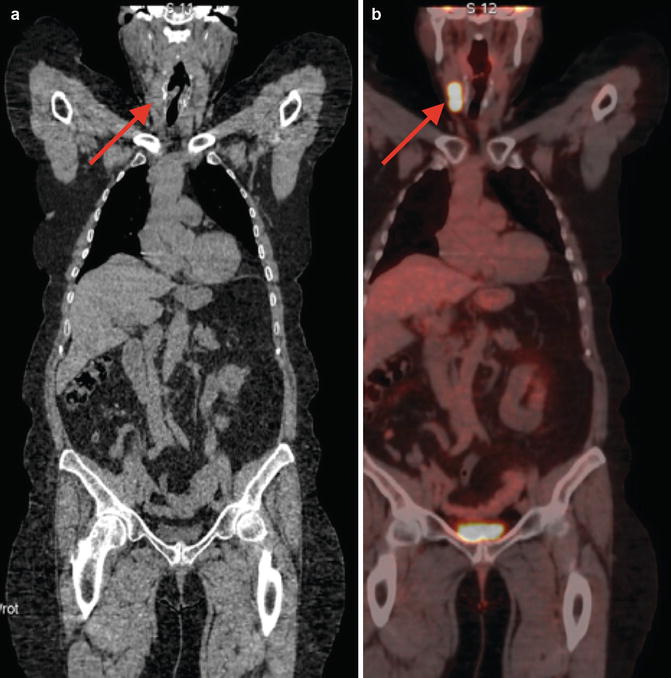
Fig. 11.9
F18-FDG PET/CT coronal slice (a) CT and (b) PET/CT in a patient with aggressive medullary thyroid cancer, with rapid progression of lymph node metastases
Considering that metastatic MTC is an incurable disease, the management aims are to provide locoregional disease control; palliate symptoms of hormonal excess, pain, or bone fracture; and control metastases that threaten life. In this light, all efforts should be done to find the best imaging tool able to visualize earlier the persistent, recurrent, or metastatic disease.
11.7.2.3 PET/CT in the Follow-Up of Anaplastic Thyroid Carcinoma (ATC)
Unfortunately, this examination does not have significant importance in this case because of the very aggressive natural history of the disease, of the rapid local evolution, and of the often-limited medical intervention. Frequently, CT and MRI are able to establish the extension of the disease.
If disease is controllable, consider F18-FDG PET/CT 3–6 months after initial therapy (NCCN 2016). The aggressiveness of the disease makes anaplastic thyroid cancer very sensitive to F18-FDG PET/CT, lesions presenting high FDG uptake (Figs. 11.10 and 11.11).

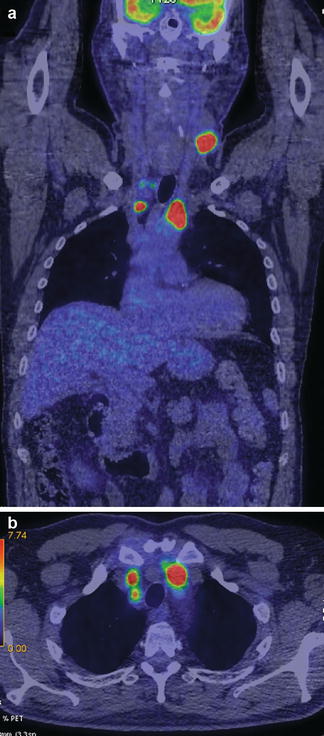

Fig. 11.10
F18-FDG PET/CT coronal slice in a patient with aggressive anaplastic thyroid cancer, with tracheostomy
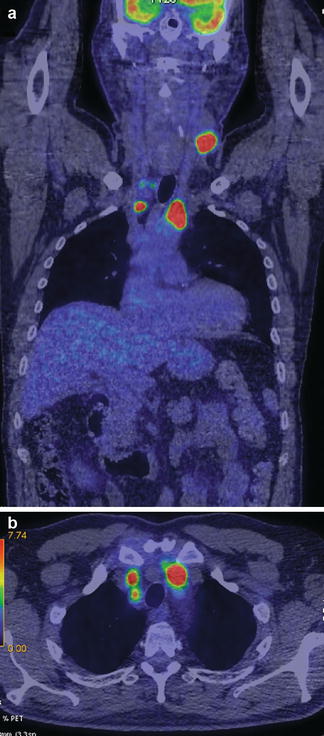
Fig. 11.11
F18-FDG PET/CT coronal slice (a) and transversal slice (b) in a patient with aggressive anaplastic thyroid cancer of the left lobe and lymph node metastases
Scintigraphy with radiolabeled somatostatin analogues (SRS) has proven useful in diagnosing somatostatin receptor-positive tumors (SSTRs). Recently, PET-SSTR analogues with Ga-68 have been successfully introduced. The content of SSTR is important for the success of SSTR therapy with or without radiolabeling. There are some studies about the SSTR status of thyroid cancer patients (DTC radioiodine non-avid, MTC, ATC) comparing the recently described radiopharmaceutical Ga-68 DOTA-LAN and established Ga-68 DOTATOC by PET imaging for patient selection for peptide receptor radionuclide therapy (PRRT).
11.7.3 The Role of PET/CT in Other Malignancies Associated with Thyroid Carcinoma
In the situation of second malignancies, PET/CT gives the chance of a better prognosis to patients, so synchronic or metachronic cancers benefit from early detection. A multicenter study performed in 13 medical centers in Europe, Canada, Australia, and Singapore showed a 30% increased risk of second primary cancer after thyroid cancer and increased risks of thyroid cancer after various primary cancers. Also, North American researchers published similar results.
The author (Piciu et al. 2016) published from the personal database that second primary malignancies occurred after DTC in 1990 patients treated between 1970 and 2003. The mean long-term follow-up period was 182 months. The relative risk of development of second malignancy in DTC patients was increased (p < 0.0001) for breast, uterine, and ovarian cancers compared with the general population. The overall risk concerning the development of second primary malignancies was related to the presence of DTC, but not to exposure to the low and medium activities of radioiodine administered as adjuvant therapy.
The oncologists published the relation between disorders in the thyroid and breast leading to carcinomas, so in both cancers there is a special attention given to screening. The PET/CT has an important role in these situations.
A special attention should be given to thyroid lymphoma, where the pathology is treated as a hematological disease, and the diagnosis and monitoring protocols are those established by the specific committees. A standard place is reserved to F18-FDG PET/CT, due to its importance in the algorithm of follow-up. The intensity of F18-FDG uptake expressed by SUV is considered an essential tool in the treatment response assessment. The Deauville criteria (the five-point scale) introduced for the assessment of response to therapy might be also applied in particularly affected thyroid gland.
The German authors published (Baras et al. 2017) that the increased risk of subsequent primary malignancies (SPM) in survivors of adult-onset Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL) in 128, 587 patients registered during more than 20 years was significantly increased over twofold for HL survivors and 1.5-fold for NHL survivors compared with the general German population. These cancers consisted in lip/oral cavity, colon/rectum, lung, skin melanoma, breast, kidney, and thyroid. Significantly increased SIRs for esophagus, stomach, liver, pancreas, testis, prostate, and brain/central nervous system were observed following NHL only.
Considering these data, the consistent screening by PET/CT in lymphoma should be essential in early diagnosis and correct assessment of both diseases.
Some clinical examples will be detailed in this chapter, keeping in mind that:
Thyroid cancer might be associated with other malignancies, so during PET/CT performed for the specific indication of TC, these pathologies are discovered.
Thyroid might be the host for metastases from other cancer, mainly renal, breast, lung, and melanoma.
Other malignancies during their monitoring protocols by PET/CT might be associated with thyroid cancer, expressed by increased focal uptake in the thyroid.
Case 1: Papillary Thyroid Carcinoma and Colon Cancer
History:
A 62-year-old male, with the diagnosis of papillary thyroid carcinoma operated 2 years before with total thyroidectomy and selective lymph node dissection, was irradiated with 100 mCi (3.7 GBq) I-131. He was examined in the follow-up.
T3N1aM0—stage III.
Clinical examination:
The patient was under L-thyroxin 150 μg/daily, in normal thyroid status; he had no signs of thyroid dysfunction.
The neck examination revealed a post-thyroidectomy scar, without any palpable tumor mass or lymph nodes in the cervical area. No other signs or symptoms to be mentioned.
Examinations:
Ultrasound—no thyroid tissue remnant, no lymph nodes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree