Susan E. Cohn, Rebecca A. Clark Keywords antiretroviral therapy in women; bacterial vaginosis; breast-feeding; cervical dysplasia; contraception; fertility desires; genital HIV shedding; heterosexual transmission; human immunodeficiency virus (HIV); human papillomavirus (HPV); perinatal transmission; preconception counseling; pregnancy; pregnancy management; sexually transmitted disease (STD); sexually transmitted infection (STI); women
Human Immunodeficiency Virus Infection in Women
Human immunodeficiency virus (HIV) infection has had a profound impact on the health of women worldwide. By the end of 2011, more than 50% of the more than 34 million people living with HIV infection were women.1 HIV infection and the resultant acquired immunodeficiency syndrome (AIDS) are the leading causes of death among women in their reproductive years (ages 15 to 49).2,3 Sub-Saharan Africa remains the most severely affected region, with nearly 1 in 20 adults (4.9%) living with HIV infection (more than half of whom are women) and accounting for 69% of all people living with HIV infection worldwide.1 In the United States, 7% of all cases of AIDS reported as of 1985 occurred in women; this proportion increased to 26% of all AIDS cases newly diagnosed in 2001 and has stabilized at 25% to 27% through 2011.4,5 With the advent of increasing access to potent HIV antiretroviral therapy (ART) worldwide, new HIV infection rates have decreased overall and by 50% or more in many countries, including some in sub-Saharan Africa.1,3 Half of all the reductions in HIV infections recently have been among children, with increasing use of ART for prevention of mother-to-child transmission (PMTCT). However, people infected with HIV continue to face stigma, discrimination, and injustice; and women and girls continue to be at higher risk for HIV infection because of gender inequity and sexual violence.1
In this chapter, the epidemiology of HIV infection in women, transmission of HIV to women, prevention of heterosexual HIV transmission, pregnancy and risk for perinatal transmission, and clinical manifestations and management issues for women infected with HIV are discussed.
Epidemiology
United States
When AIDS first was recognized in 1981 it was considered to be a disease of men who have sex with men (MSM) and of injection drug users. With the rapid increase in the number of women infected with HIV has come an increased understanding of the potential for heterosexual transmission of HIV infection. By 2001, women accounted for 26% of new AIDS diagnoses (11,164/43,158 cases), 18% of the 816,149 cumulative AIDS cases, and 32% of newly reported HIV diagnoses (11,394/35,575 cases); and this percentage has remained fairly stable over time, with over 280,000 women among the 1.1 million people living with HIV infection and AIDS in the United States as of 2011.4,6 Overall, in the United States, AIDS rates continue to be lower in women than in men: 6.0 per 100,000 women compared with 19.1 per 100,000 men in 2011.5
Women are acquiring HIV infection primarily through heterosexual contact, with a decrease in injection drug use–associated cases since 1992. Since 1995, heterosexual contact has become the predominant mode of exposure for women in the United States, accounting for 78% of new HIV infections among women in the United States in 2011, with 20% due to injection drug use.5,7 Although most diagnoses of HIV infection among women aged 13 years or older were attributed to heterosexual transmission, in 2009 18% were attributed to injection drug use among women 45 years and older compared with 9.6% among women aged 13 to 19 years.8 The 9,500 new HIV infections among women in 2010 reflect a significant 21% decrease from the 12,000 new infections among women in 2008.9 Transmission patterns have shifted over time within the United States, with most new HIV infections occurring through male-to-male sexual contact (63% in 2010). New infections among MSM increased from 2008 to 2010, as has the growing proportion among heterosexuals.6 Bisexually active men also may be contributing to the spread of HIV infection to women because, at least in a Boston cohort, they were more likely to have unprotected sex with their female partners than with their male partners.10,11 Black men who have sex with both men and women but who do not identify as gay or disclose their bisexual activities to main female partners, also known as men “on the down low,” have been cited as one of the reasons for the increase in HIV infections in black women.12
HIV disproportionately affects women of color; cases in black and Hispanic women accounted for 83% of reported AIDS cases in 2011.5 The AIDS case rate for black women was 33.7 per 100,000 or 22 times the rate for white women (1.5).6 The case rate for Hispanic women of 7.1 was five times the rate for white women.6 In 2010, black women accounted for 64% of new AIDS diagnoses among women ages 13 and older but only 13% of the U.S. population of women.6 Hispanic women are also overrepresented, accounting for 17% of new AIDS diagnoses, compared with 14% of the U.S. female population ages 13 and older.6 The highest rates of AIDS diagnoses were among black women living in the northeastern (52.4/100,000) and southern (36.1/100,000) states.8 HIV infection is predominantly a disease of women of childbearing age; in 2009, 68% of new HIV infections among women were diagnosed in girls and women between 13 and 44 years of age. With the aging of the HIV epidemic among women, the percent of HIV-infected women older than 50 continues to grow; however, underrecognition of HIV may be common and older women typically present for medical attention with advanced disease and are unaware of their risk for HIV infection.4,13,14 A study of women older than 50 with AIDS found that they were more likely than younger women to live alone (24% vs. 11%), to have not completed high school (63% vs. 37%), to be tested for HIV infection while hospitalized (51% vs. 32%), and to have never used a condom before diagnosis of HIV infection (86% vs. 67%).15 Within the United States, more than 1.1 million people are living with HIV infection and 18.1% are unaware of their infection.9 The gravity of the HIV epidemic among U.S. women is often not appreciated by those at risk and by the broader community.16 A recent cohort study of high-risk women in the northeastern and southeastern states found an annual HIV incidence of 0.32%; and older age, substance use, and knowing that a partner had HIV were associated with HIV prevalence.17 With the increasing use of routine, rapid HIV testing of adults in the United States, it is hoped that more people will be identified earlier and started promptly on ART.18
The AIDS epidemic has had a major impact on morbidity and mortality among young women. By 1992, AIDS was the fourth leading cause of death among women 25 to 44 years old in the United States and was the leading cause of death among women in the same age group in 15 primarily eastern coastal cities.19 By 1995, HIV infection was the third leading cause of death in women in this age group and the leading cause of death among African-American women.20 Deaths from AIDS peaked in 1994 and 1995 and then began decreasing in 1996. The percentage decrease in mortality was smallest among African-American women and women from southern states; the highest death rates were among the population below the poverty level.21 In 2008, death rates from HIV were highest among African-Americans (22.1 per 100,000, 10 times higher than among whites, and nearly four times higher than the rate for Hispanics).8 Decreased mortality has been attributed to improved combination regimens, including protease inhibitors and non-nucleoside reverse-transcriptase inhibitors (NNRTIs), rather than to advances in the prevention of HIV transmission; there continue to be approximately 50,000 new HIV diagnoses annually in the United States, with 25% being female.22 Medical advances and programs aimed at prevention and medical care have reached many but not all people with or at risk for HIV infection. Although 82% of people with HIV infection are diagnosed, and 66% are linked to care, fewer remain in regular care (37%) and are prescribed ART (33%), with only 25 being virally suppressed. The percent with viral suppression is even lower among blacks (21%) and young people aged 25 to 34 (15%).22 In July 2010, the U.S. Government released the National HIV/AIDS Strategy, a comprehensive plan to address the HIV epidemic. The strategy has three primary goals—reduce new infections, increase access to care, and improve health outcomes—along with reduction of HIV-related health disparities.23
The epidemiology of drug use affects the epidemiology of HIV infection among American women. In 1996, after exclusion of the 24% of women whose initial mode of transmission was not reported, two thirds of HIV-infected women reported injection drug use (45%) or heterosexual contact with an injection drug user (18%).24 By 2001, after excluding the 42% of women without a reported risk behavior, only one third of women with newly diagnosed AIDS reported injection drug use and 14% reported heterosexual contact with an injection drug user.4 In 2009, the percentage of HIV infections attributed to injection drug use was highest among white women (23%), followed by Hispanic (17%) and black women (13%); older women with HIV aged 35 to 44 and 45 and older had the highest percentage attributable to injection drug use of 15.9% and 17.9%, respectively.8 Since the mid-1980s, heroin has become less popular whereas cocaine and other drugs have been used increasingly. When used intravenously, these newer drugs typically are injected more frequently and are associated with increased needle sharing.25 The use of smokable freebase (“crack”) became widespread after its first appearance in New York City in 1985 because of its low cost and high addictive potential. Although smoking crack cocaine itself does not transmit HIV, the tendency of persons who use crack to engage in unsafe behaviors, such as increased sexual activity with multiple partners and exchange of sex for drugs, has resulted in the increased spread of HIV infection and other sexually transmitted infections (STIs), including syphilis.26,27
Female-to-female sexual transmission of HIV is exceedingly rare. Moreover, in populations of women with HIV infection who report having sexual contact only with women, most have had a history of injection drug use and the rest had received a blood transfusion in the first few years after HIV infection was identified; no cases were attributable to female-to-female sexual transmission.21,28 In a study of 498 lesbian and bisexual women frequenting public venues in San Francisco and Berkeley, California, 6 (1.2%) were HIV infected.29 This population showed high rates of high-risk behaviors (10% reported injection drug use, and 40% reported unprotected sex with men, some of whom were bisexual men and male injection drug users), and no evidence of sexual transmission between women was found. These data and other more recent studies suggest that the frequency of female-to-female HIV transmission remains very low.30
HIV transmission through intravaginal insemination of donor semen has been reported.31–33 Use of assisted reproductive technologies, which include sperm washing and intracytoplasmic sperm injection, seems to have an extremely low risk for horizontal transmission from an HIV-infected man to an HIV-negative woman or vertical transmission to children born as a result of these procedures.34,35,36–40 Although these techniques seem to be promising, they are rarely available in the United States outside a research setting, require specialized laboratories, are quite expensive, and typically are not covered by insurance and thus are not accessible to most couples (see “Strategies to Prevent Heterosexual Transmission” and “Fertility Issues”). Given their remarkable success, many experts now advocate that assisted reproduction with sperm washing not be denied to serostatus-discordant couples in developed countries and, where possible, should be integrated into a global public health initiative for HIV infection in health care resource–constrained regions.41
Worldwide
New estimates from the World Health Organization (WHO) indicate that HIV infection continues to be prevalent worldwide, having resulted in more than 60 million infections.1 As of December 2012, there were an estimated 34 million people living with HIV infection, over half of whom are women, and nearly 30 million people have died of HIV infection–related causes since the start of the epidemic.2 HIV infection has been reported from all over the world, but most infected persons (97%) reside in low- and middle-income countries and more than two thirds live in sub-Saharan Africa.2 Approximately 2.5 million people were newly infected with HIV in 2011, which equates to more than 7,000 a day. The rate of new HIV infections has decreased in several countries, but globally these favorable trends are at least partially offset by increases in new infections in other countries.1 As treatment access continues to increase, the annual number of HIV-associated deaths, at 1.7 million deaths in 2011, has fallen, a decrease in 24% since 2005.3 However, new infections continue to outstrip access to treatment, with two new infections occurring for every person starting treatment. Globally, as access to services for PMTCT has increased, the number of children being born with HIV infection has decreased, with 370,000 children newly infected in 2009, a decrease of 24% from 5 years earlier.1,3
Worldwide, HIV infection is spread primarily through heterosexual contact, although injection drug use and its contribution to exposure to HIV vary geographically. Because female drug users have sexual partners who are at high risk for HIV infection and because injection drug use can lead to exchange of sex for drugs or money, there may be underrecognition and underreporting of cases spread through heterosexual contact. Several recent studies suggest that unprotected anal sex between men is probably a more important factor in the epidemics in sub-Saharan Africa than is commonly believed. In Zambia, one in three (33%) surveyed MSM tested HIV positive.1 In the Kenyan port city of Mombasa, 43% of men who said they had sex only with other men were found to be living with HIV infection.42 In virtually all regions outside sub-Saharan Africa, HIV disproportionately affects injection drug users, MSM, and sex workers.1
The most recent international epidemiologic data contain some favorable news. In some countries in Asia, Latin America, and sub-Saharan Africa the annual number of new HIV infections is decreasing.1 In western, central and eastern Europe, central Asia, and North America the rates of annual new HIV infections have been stable for at least the past 5 years.1 However, there has been a resurgence of HIV infection in several high-income countries among MSM. In eastern Europe and central Asia, high rates of HIV transmission continue to occur in networks of people who inject drugs and their sexual partners. The estimated rate of AIDS deaths has also decreased, in part as a result of increased availability of ART as well as decreased incidence of HIV infection, including increased access to successful PMTCT programs in health care resource–limited settings.1
The geographic region hardest hit by HIV/AIDS is sub-Saharan Africa, accounting for 67% of all new HIV infections and 80% of the world’s HIV-positive women.43 Almost 90% of the 2 million HIV-infected children live in sub-Saharan Africa. In 2011, new HIV infections in children were 43% lower than in 2003 and 24% lower than in 2009, demonstrating that elimination of new infections in children may be possible.2 Women account for 59 percent of adults with HIV in sub-Saharan Africa, and this is primarily the result of unprotected heterosexual intercourse.3 Most epidemics in sub-Saharan Africa appear to have stabilized, although often at very high levels, particularly in southern Africa. Additionally, in a growing number of countries, adult HIV prevalence has been decreasing. For the region as a whole, women are disproportionately affected compared with men, with especially stark differences between the sexes in HIV prevalence among young people 15 to 24 years of age. In southern Africa, decreases in HIV prevalence are especially striking in Zimbabwe, where HIV prevalence in pregnant women attending antenatal clinics decreased from 26% in 2002 to 18% in 2006.1 The 26% HIV prevalence found in adults in Swaziland in 2009 is the highest prevalence in the world.1,44 In Botswana, where ART coverage exceeds 90%, the estimated annual number of AIDS-related deaths declined in half from 2002 to 2009, whereas the estimated number of children newly orphaned by AIDS fell by 40%.1,44 Despite more recent positive trends, these countries all face massive challenges not only to sustain and expand prevention efforts but also to provide adequate treatment (including ART), care, and support to the millions of people living with HIV infection and AIDS or orphaned by the epidemic.1 The extensive provision of ART in Botswana has averted approximately 50,000 adult deaths and could lead to an estimated reduction in 130,000 deaths there through 2016.44
In eastern Europe and central Asia, the estimated number of people living with HIV increased to 1.4 million in 2009, compared with 760,000 in 2001.1 The HIV epidemic in the Russian Federation continues to grow, fueled by a rise in HIV infection among injection drug users, sex workers, and their various sexual partners.1,44 In the Russian Federation, more than a third (37%) of the 1.8 million injection drug users are believed to be infected with HIV, with surveys of injection drug users yielding HIV prevalence rates as high as 88% in the city of Kryvyi Rih.1 By 2009, approximately 45% of the HIV-infected population living in Ukraine were women, up from 41% in 2004; an estimated 35% of women probably acquired HIV through injection drug use, whereas an additional 50% were probably infected by partners who used injection drugs.1
The Asian HIV epidemic with an estimated 4.9 million people living with HIV in 2009 is largely stable.1 The epidemic is varied, being driven by injection drug users, sex workers, and MSM in countries throughout Asia. HIV has spread heterosexually among people who became infected when they sold their blood to collecting centers that improperly adhered to safety procedures.1 More recent economic and social unrest in Indonesia seems to be associated with a sharp increase in injection drug use and with it a significant increase in HIV infections. After an initial explosion in seroprevalence rates among female commercial sex workers in Thailand, government-sponsored prevention efforts have resulted in dramatically decreasing incidences.1 Many of the new HIV infections in Thailand now seem to be occurring in the sexual partners (and wives) of men who were infected by sex workers in the 1990s.1 In India, a significant proportion of women with HIV have probably been infected by their regular partners who have had a history of paying for sex.1
The HIV epidemic is well established in Central and South America, yet the HIV prevalence continues to rise even with improved access to ART. The epidemic is concentrated in and around networks of MSM. Social stigma has kept many of these MSM hidden, and fear of being stigmatized has led many MSM to also have sexual relations with women. In Central America, more than one in five MSM reported having sex with at least one woman in the previous 6 months.1 Efforts to control HIV spread among sex workers have been successful, with reported high condom use rate and low HIV prevalence among female sex workers in Santiago, Chile.1
The high mortality rate for HIV/AIDS continues to have a major impact on families. At the end of 2011, 17.3 million children and adolescents worldwide had been orphaned by loss of one or both parents to AIDS.1 More than 80% of children orphaned as a result of AIDS were in sub-Saharan Africa.45 Saving lives of parents through access to ART in health care resource–limited countries and helping to alleviate poverty and improve education are central to the global response to the orphan crisis.45
Transmission
Heterosexual Transmission
Efficiency of Transmission
Globally, heterosexual transmission accounts for the spread of HIV infection in approximately 90% of persons living with AIDS.2 Mechanisms of heterosexual transmission, however, remain poorly understood.46 HIV has been isolated from semen of HIV-infected men and from cervicovaginal secretions of HIV-infected women. Although heterosexual transmission seems more efficient from men to women than from women to men, HIV-infected women can spread HIV to their uninfected sexual partners.47–49 The most likely explanation for this difference in ease of HIV spread from men to their partners relates to the larger volume of semen compared with cervicovaginal secretions and to the higher concentration of HIV on average in seminal fluid.
HIV is not transmitted consistently by sexual contact. Although some persons become infected after a single sexual exposure or artificial insemination with HIV-infected semen,32 others remain uninfected despite hundreds of exposures.50–52 This lack of transmission may be due to the amount of virus, the host immune response, the relative virulence of HIV isolates, or some combination thereof.
The efficiency of heterosexual transmission of HIV between women and men has not been characterized fully. The efficiency of transmission of gonorrhea, a well-studied sexually transmitted disease (STD), is approximately 25% after a single male contact with an infected woman and close to 90% for transmission by infected men to uninfected female partners.53,54 HIV is much less efficiently transmitted; however, the extremely long incubation period of HIV disease has hindered specific inferences about the relative rates and efficiency of sexual transmission because many persons do not learn of their infection until years after the relevant exposure. Estimates of infectivity for each sexual contact have ranged from 3 per 100 for the most efficient transmitters in a male homosexual cohort study55 to less than 1 per 10,000 contacts in studies of heterosexual couples discordant for HIV serostatus.47,50,56 In a California study of heterosexual HIV serostatus-discordant couples, the risk for male-to-female transmission was 17 times higher than the risk for female-to-male transmission.48 An Italian study of 730 discordant heterosexual couples found the transmission of HIV from men to women to be twice as efficient as from women to men.57 More recent studies of monogamous HIV-discordant partners in Uganda suggest that the efficiency of HIV spread may be more similar between men and women than was appreciated initially.56
Associated Factors
Factors that have been associated with the greater likelihood of transmitting HIV between heterosexual partners include viremia of greater magnitude or more advanced immunodeficiency in the infecting partner, the presence of any STD, including ulcerative and nonulcerative disease; sexual activity during menses; receptive anal sex; unprotected vaginal sex; traumatic sex; increased number of sexual contacts; and infectivity of the HIV-infected partner.55,58–60 Baeten and associates demonstrated that genital HIV type 1 (HIV-1) RNA independently predicted HIV-1 transmission risk even after adjusting for plasma HIV-1 quantity, suggesting that genital HIV viral load could be used as a marker of HIV-1 sexual transmission risk.61 Male circumcision62–65 was shown in randomized trials in Africa to decrease female-to-male HIV transmission by 60%.66 Because male circumcision provides only partial protection, higher risk behaviors could nullify the effect of circumcision. Additionally, circumcision among HIV-infected men may not directly decrease male-to-female HIV transmission among discordant couples, according to a study from eastern and southern Africa of 1096 heterosexual serostatus-discordant couples in which the HIV-infected partner was male.63,66 To realize its optimal protective benefit in areas of highest HIV prevalence, implementing male circumcision will require consistently safe sexual practices, with increased emphasis on surgical training, aseptic techniques, acceptability, availability, and cultural considerations.64
Recent work has delineated the complexity of the female reproductive tract, the cyclical sex hormones, and the immune defenses, creating a “window of vulnerability” to HIV and other infectious agents when the humoral, cell-mediated, and innate immune defenses are suppressed during the ovulatory phase of the menstrual cycle.67 Cervical mucus and cervicovaginal mucus have recently been shown to impede the diffusion of HIV, helping to examine why conditions such as bacterial vaginosis that can disrupt mucus have been associated with increased HIV transmission.68
Hormonal contraception has intermittently been associated with increased risk for HIV-1 transmission and acquisition, mostly from retrospective studies or from studies designed to assess different outcomes.69–71 Heffron and co-workers conducted secondary data analyses from the Partners in Prevention HSV/HIV Transmission Study on 3790 heterosexual HIV-discordant couples enrolled in two longitudinal studies in seven African countries.69 Incidence of HIV infection among female hormonal contraception nonusers was 3.8/100 person-years, compared with 6.9/100 person-years among users of injectable forms of contraception (P = .04) and 5.9/100 person-years in oral contraceptive users (P = 0.33). Among men, the incidence of HIV infection was 1.5/100 person-years in partners of HIV-positive hormonal contraception nonusers, compared with 2.6/100 person-years in partners of those using injectable drugs (P < .05) and 2.5/100 person-years in men whose HIV-infected partners used oral contraceptives (P = .31).69
There were several confounding factors that could not be controlled, including misreporting of condom use, especially given the high pregnancy rates among the serostatus-discordant couples.70 Clinicians and patients need to weigh the potential risk for hormonal contraception with known risks for unwanted pregnancies with its known morbidity and mortality.70 In February 2012, the WHO convened a technical consultation regarding hormonal contraception and HIV acquisition, progression, and transmission to consider whether the current WHO guideline Medical Eligibility Criteria for Contraceptive Use should be changed.72 After the current data were summarized, it was concluded that there should be no restrictions on the use of any hormonal contraceptive method for women at high risk for HIV infection or living with the infection. However, the group recommended that a new clarification be added that women at high risk for HIV infection or living with HIV infection and using hormonal contraception should be strongly advised to always use condoms, male or female, and other HIV preventive measures because hormonal contraceptives are not protective against HIV transmission or acquisition. In June 2012, the Centers for Disease Control and Prevention (CDC) issued a similar statement of clarification to the U.S. Medical Eligibility Criteria for Contraceptive Use73 stating that women at high risk for HIV infection using progestin-only injectable contraception should be strongly advised to also always use condoms (male or female) and take other preventive measures to avoid HIV transmission.73
For HIV-infected women, hormonal contraception prevents unintended pregnancy, excess maternal morbidity, and vertical HIV transmission. Given their global widespread use, concern was raised that hormonal contraception might lead to more rapid HIV disease progression. Heffron and colleagues studied 2269 chronically HIV-infected women from their African cohort.74 They found that there was no evidence that the use of hormonal contraception overall or the use of either injectable or oral contraception use, respectively, led to accelerated disease progression.74
Huijbregts and associates explored the role of medroxyprogesterone acetate (MPA), the active component of depot medroxyprogesterone acetate (DMPA), the most widely used progestin-only injectable contraceptive, on the immune system.75 They showed that MPA inhibited the cytokine and chemokine production by peripheral blood cells and activated T cells and that MPA prevented the downregulation of HIV-1 co-receptors CXCR4 and CCR5 on the surface of T cells after activation and increased HIV-1 replication in activated peripheral blood mononuclear cell cultures, suggesting that MPA may suppress both innate and adaptive arms of the immune systems, thus resulting in a reduction of host resistance to invading pathogens.75 Numerous studies and recent reviews of hormonal contraception and HIV acquisition have not demonstrated a statistically significant increase in risk for HIV infection. However, the ongoing uncertainty, especially with respect to injectable hormonal use, underscores the need for dual protection with condoms and other preventive methods and the need for diverse contraceptive options for women at risk for HIV infection.76–78
Other less well-documented factors that are believed to increase the risk for heterosexual transmission include cervical ectopy or use of nonoxynol-9 (Table 128-1). A chemokine receptor gene mutation (i.e., a 32-base pair deletion in CCR5) seems to confer resistance to HIV in persons who are homozygous for this trait.59 Although persons with more advanced disease are more likely to transmit HIV, consistent with their increased viral burden, the data are incomplete. Using data from a study of HIV serostatus-discordant couples in Rakai, Uganda, Hollingsworth and colleagues79 estimated that those with primary infection and late-stage infection were 26 and 7 times, respectively, more infectious than those with asymptomatic infection. High infectiousness during primary infection was estimated to last for approximately 3 months after seroconversion, whereas high infectiousness during late-stage infection was estimated to be concentrated between 19 months and 10 months, respectively, before death.79
TABLE 128-1
Risk Factors Associated with Sexual Transmission of HIV
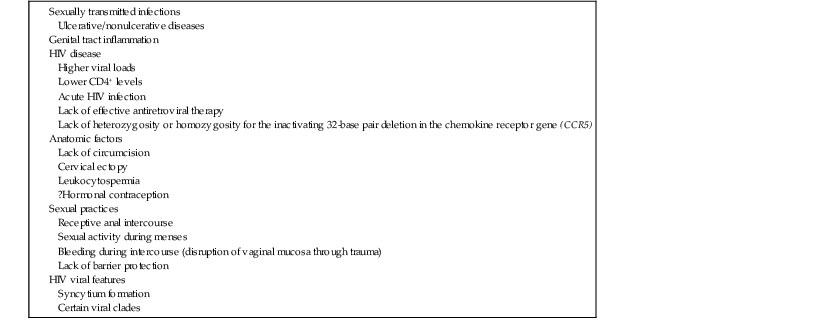
HIV, human immunodeficiency virus.
In some men receiving potent ART, HIV was cleared successfully from the blood to below the level of detection of some laboratories (e.g., <400 copies/mL), but the men still were able to transmit HIV, suggesting a compartmentalization of HIV between semen and plasma.80 Many investigators have found that treatment-induced changes in HIV viral load generally are associated with a corresponding change in the amounts of seminal and cervicovaginal HIV RNA, supporting the hypothesis that potent ART may reduce the spread of HIV.81–85 Observational studies among HIV-1 serostatus-discordant couples have associated ART initiation with a reduction in HIV transmission of 80% to 92%, and a recent randomized trial demonstrated that earlier initiation of ART (at CD4 counts of 350 to 550 cells/mm3) in the context of virologic monitoring and adherence support resulted in a 96% reduction in HIV transmission.86,87
STDs, particularly diseases associated with genital ulcers, increase the efficiency of HIV transmission and the susceptibility to HIV infection.84 Genital ulcerative diseases, which include syphilis, chancroid, and genital herpes, are thought to enhance the access of HIV to mucosal tissues, lymphatic drainage, and systemic lymphocytes.85,88 HIV also may be transmitted through intact mucosal membranes, presumably by infecting dendritic cells within the mucous membranes of the genital tract.89 Epidemiologic studies suggest that ulcerative and nonulcerative STDs increase the susceptibility to HIV infection; female sex workers in Zaire had an increased risk for HIV seroconversion if they had nonulcerative STDs,90 and among HIV serostatus–discordant sex partners, seroconversion was more likely if the previously HIV-negative sex partner had ulcerative and nonulcerative STDs.91 Nonulcerative STDs, such as gonorrhea, chlamydial infection, and trichomoniasis, seem to increase the number of lymphocytes, monocytes, and Langerhans cells in the endocervix in susceptible seronegative women and provide more potential targets for HIV infection.84 Similarly, nonulcerative STDs may increase the number of HIV-infected cells in the genital tracts of HIV-positive transmitters. Cohen and associates92 found that HIV-infected men with urethritis had seminal plasma HIV-1 RNA eight times the levels in seropositive men without urethritis. Treatment of urethritis was associated with significant decreases in HIV-1 concentration in semen, suggesting a decrease in infectivity with successful STD treatment.
Bacterial vaginosis has been associated with higher concentrations of HIV RNA in the genital tract of HIV-infected women,93 increased risk for HIV transmission to male partners,94 and a 60% increased risk for HIV acquisition in women.95 Recently, Cohen and co-workers studied 2236 HIV-seropositive women and their HIV-uninfected male partners from the African Partners in Prevention HSV/HIV Transmission Study to see if bacterial vaginosis was associated with increased HIV transmission. They found the HIV incidence in men whose HIV-infected female partners had bacterial vaginosis was 2.91 versus 0.76 per 100 person-years in men whose female partners had normal flora (hazard ratio [HR], 3.62; 95% confidence interval [CI], 1.74 to 7.52).94 After controlling for sociodemographic factors, sexual behavior, male circumcision, STIs, pregnancy, and plasma HIV-1 RNA levels in female partners, bacterial vaginosis was associated with a greater than threefold increased risk for female-to-male HIV-1 transmission (adjusted HR, 3.17; 95% CI, 1.37 to 7.33).94 However, there were several limitations affecting the generalizability of their results, including that all the participants were involved in a clinical trial and underwent couples HIV counseling and testing and index participants had baseline CD4 counts greater than or equal to 250 cells/mm3 and were herpes simplex virus type 2 (HSV-2) seropositive. Mitchell and associates studied 54 HIV-infected U.S. and Kenyan women prospectively and found in the women on ART that HIV shedding was greater if they were coinfected with certain bacterial vaginosis–associated species compared with women not on ART.93 Vaginal Lactobacillus species were associated with lower risk for genital HIV shedding, whereas the presence of certain bacterial vaginosis–associated species may increase that risk.93
The use of ART has led to significant decreases in morbidity and mortality due to HIV infection. Epidemiologic data suggest that ART has contributed to a resurgence of unsafe sexual practices, especially among some MSM.6,96 ART is believed to be associated with a loss of fear of acquiring and transmitting HIV, decreased use of condoms, and more unsafe sex among HIV-discordant and HIV-concordant couples, especially if they have responded well to ART. Other current factors associated with potential increases in sexual transmission of HIV include use of the Internet to identify potential sex partners (e.g., serosorting),97,98 increased use of erectile dysfunction medications (e.g., sildenafil [Viagra]) as recreational drugs, and increased desire of HIV-infected persons to have children.96,99,100,101,102
HIV Infection within the Genital Tract
Much research has been dedicated to isolation, identification, and quantification of the amount of HIV present within cervicovaginal secretions. The presence of HIV in the female genital tract is necessary for heterosexual transmission of HIV61 and for perinatal transmission of HIV during labor and delivery. HIV-1 has been isolated from cervical and cervicovaginal secretions obtained using cervicovaginal lavage and vaginal or cervical swabs or wicks.103 Although viral loads in genital secretions tend to be lower after initiation of effective antiretroviral medications, detectable HIV in genital secretions has been reported in men and women with undetectable plasma HIV levels.104,105 Patients with a low plasma virus burden still may potentially transmit HIV to a sexual partner or perinatally to an infant, although the risk is low.
HIV has been detected in menstrual blood, and having intercourse during menses increases the risk for infecting the male partner.106 Menstruation introduces approximately 80 mL of blood into the genital tract over a 3- to 5-day period.107 This menstrual blood is likely to contain HIV-infected cells and free virus, reflecting the HIV viral load of peripheral blood. Menstrual blood increases the pH in the vagina to the neutral range, improving the viability of HIV shed in menses and HIV in semen deposited in the vagina during intercourse.108 Higher levels of HIV in the genital tract may be seen with conditions that increase the vaginal pH, such as blood in the vagina, bacterial vaginosis, lack of Lactobacillus, menopause, intercourse, and possibly the use of some forms of birth control.109–112 More recent studies confirmed that although plasma HIV-1 viral load remained constant during the menstrual cycle, genital viral loads are lower in the periovulatory phase and highest during menses.113–115 These results suggest that local factors may affect the genital viral load compartment independent of plasma viral load.113–115
Research is under way to develop intravaginal microbial agents capable of decreasing the heterosexual and perinatal transmission of HIV-1.116 Although nonoxynol-9, a commonly used spermicidal agent, has anti-HIV activity in vitro, there have been safety concerns after reports of vaginal ulceration and inflammation during clinical studies.117,118 A placebo-controlled trial of nonoxynol-9 in sex workers in four countries did not show a protective effect of nonoxynol-9 on HIV-1 transmission.119 The risk for acquiring HIV was higher in the women in the nonoxynol-9 group who used a mean of 3.5 applicators or more per working day compared with women who used fewer administrations per day or the placebo. Nonoxynol-9 may cause toxic effects enhancing HIV-1 infection and should not be used as a potential HIV prevention method.
Assessment of other microbicides and antiretroviral preparations is under way, and some results have recently been published (see “Fertility Issues”).120–125 Current microbicides in trials can be categorized into vaginal defense enhancers, which help maintain the vaginal pH or facilitate the colonization of vaginal lactobacilli; surfactants (or detergents), which disrupt viral membranes; HIV entry inhibitors; and HIV reverse-transcriptase inhibitors.116 Cleansing the birth canal with chlorhexidine has been studied in Malawi; it did not decrease perinatal HIV transmission126 but did decrease early neonatal and maternal postpartum infectious problems.127
Strategies to Prevent Heterosexual Transmission
The introduction of potent combination ART in 1996 and the public health approach to HIV treatment in health care resource–limited settings in 2002 have changed the course of the epidemic.128,129 ART to reduce the infectiousness of individuals with HIV and oral and topical preexposure prophylaxis (PrEP) for uninfected individuals to prevent HIV acquisition are the most promising approaches for decreasing the spread of the virus.86 ART given to HIV-infected partners with the purpose of achieving and maintaining full virologic suppression has been shown to prevent linked HIV transmission in an African cohort of serostatus-discordant couples.87 In a meta-analysis of studies reporting HIV transmission rates, ART histories and viral loads of the HIV-positive partners, Loutfy and co-workers concluded that there is minimal risk for sexual transmission for heterosexual serostatus-discordant couples when the HIV-positive partner has full viral suppression, with caveats regarding lack of information on sexual intercourse type, STIs, and condom use.130 ART should be a key component for all combination prevention strategies, and the challenge now is to improve access to ART and use more effective, better tolerated, and more durable ART. A health care system should be developed that can seamlessly link and retain patients in care and implement necessary improvements, such as easier to use point-of-care assays for virus load.131
Treatment of STDs is likely to decrease transmission of HIV and susceptibility to HIV infection. In a Tanzanian clinical trial conducted among persons in rural communities, universal STD screening and treatment of symptomatic cases of STD resulted in a 40% decrease in HIV incidence compared with that in a village in which no STD screening or treatment was available.132 However, a randomized, placebo-controlled trial in HIV-negative, HSV-2–seropositive women in Africa and MSM in Peru and the United States demonstrated that acyclovir, 400 mg twice daily, was able to suppress HSV-2 genital ulcers but was not effective in reducing HIV-1 acquisition in HSV-2–seropositive women and MSM.133
Barrier contraceptives constitute an effective means of preventing HIV transmission. de Vincenzi91 found no heterosexual transmission among 124 HIV serostatus-discordant couples who used condoms consistently but a seroconversion rate of 4.8 per 100 person-years for the 121 serostatus-discordant couples who used condoms inconsistently. The use of barrier contraceptives such as condoms should be promoted as a means of contraception and as partial protection against HIV infection and other STDs.
The CDC expanded its prevention activities to include the Serostatus Approach to Fighting the Epidemic, a program that especially targets HIV-infected persons.134 This program encourages people to know their HIV status and, if infected, encourages them to seek high-quality care and prevention services, helps them adhere to treatment regimens, and supports them in adopting and sustaining HIV risk-reduction behavior. By ensuring quality care for the HIV infection and focusing on behavioral interventions to prevent HIV transmission, it is hoped that the 1.1 million persons living in the United States with HIV infection will limit their spread of the virus to others.22 However, approximately 18% are unaware of their HIV status and therefore unable to access clinical care and life-sustaining treatment.22 In September 2006, the CDC released revised guidelines recommending universal, routine, and voluntary HIV screening in public and private health care settings for all adults and adolescents between the ages of 13 and 64.135 Unfortunately, despite the cost-effectiveness of HIV testing and treatment in the United States,136 these guidelines have been difficult to implement fully across states and communities.137
Another strategy to decrease the sexual transmission of HIV involves the use of ART for primary prevention (i.e., PrEP). Even after more than 30 years of the HIV epidemic, the number of new infections both worldwide and in settings with highly available health care resources such as the United States has been stable. The majority of new HIV infections occur in countries with low to moderate levels of health care resources, and key populations for prioritizing novel HIV prevention interventions include young women, who face a very high incidence particularly in southern Africa, heterosexual HIV serostatus-discordant couples, and commercial sex workers.138 The past few years have seen significant advances in knowledge regarding antiretroviral-based PrEP, including definitive evidence that PrEP works for HIV prevention at least in some populations.138 Other advances include regulatory approval for combination oral emtricitabine/tenofovir disoproxil fumarate (FTC/TDF) as the first PrEP agent with a label indication for prevention of sexual HIV acquisition and the development of guidelines for delivery of PrEP in clinical settings.138 Still, many questions remain about how best to motivate uptake by populations at risk for HIV infection, how much use is sufficient to achieve protection from the virus, and are there newer, simpler PrEP agents such as a monthly injection that may be effective in the future.138 Seven randomized, double-blind, placebo-controlled clinical trials of oral and topical TDF-based PrEP for HIV prevention have been conducted in the context of HIV prevention services. These have included HIV and risk-reduction counseling to participants and their partners, screening and treatment for STIs, provision of condoms, referrals for male circumcision, and provision of ART to HIV-infected partners.138 Table 128-2 highlights the key PrEP studies in women, their primary findings, and the fact that not all clinical trials of PrEP have demonstrated efficacy for HIV prevention in women. There is much that is not yet understood in terms of PrEP for women, such as what is the optimal drug concentration necessary to prevent HIV transmission, how should ART be given (e.g., orally, vaginally, parenterally), what is the optimal timing of dosing (around coitus or daily administration) and for how long, and how can we promote effective use of prevention strategies.138
TABLE 128-2
Preexposure Prophylaxis Antiretroviral Therapy–Based Clinical Trials in Women
| STUDY POPULATION | LOCATION | INTERVENTION | OUTCOME | COMMENTS | |
| CAPRISA 004121 | 889 women; at high risk; aged 18-40 yr | South Africa | TDF vaginal gel vs. placebo; coitally associated use | 39% protection (95% CI, 6%-60%; P = .017) | Detection of high concentrations of TDF in cervicovaginal fluid associated with 74% reduced risk |
| TDF2123 | 1219 sexually active adults; 55% male, 45% female; approximately 90% age 21-29 yr | Botswana | Daily oral TDF/FTC vs. placebo | 63% protection (95% CI, 22%-83%; P = .01) | >30% did not complete study; greater TDF blood concentrations in those who remained HIV uninfected compared with those who acquired HIV; cannot draw definitive conclusions for women and men separately |
| Partners PrEP Study66 | 4758 heterosexual serodiscordant couples; 38% negative-female, 68% negative-male partner; median age 33 yr | Botswana, Kenya, Rwanda, South Africa, Tanzania, Uganda, Zambia | Daily oral TDF, TDF/FTC, or placebo | 67% protection with TDF alone; 75% protection with TDF/FTC; TDF vs. FTC/TDF: not statistically significant in primary analysis | TFV detected in blood samples from 82% of a subset of HIV-uninfected subjects vs. 31% of those who acquired HIV; detection of TFV in blood associated with 86%-90% protection |
| FEM-PrEP463 | 2120 heterosexual women at high risk for infection aged 18-35 yr | Kenya, South Africa, Tanzania | Daily oral TDF/FTC vs. placebo | Trial discontinued for lack of efficacy for HIV prevention in April 2011 | TFV consistently detected in blood samples from <30% of a subset of HIV-uninfected subjects |
| VOICE (MTN-003)124 | 5029 heterosexual women aged 18-45 yr in high-prevalence areas | South Africa, Zimbabwe, Uganda | Daily oral TDF, FTC/TDF, or placebo or daily vaginal TDF gel or placebo gel | TDF and TDF gel discontinued early owing to lack of efficacy for HIV protection. No study drug significantly reduced the risk for HIV acquisition: HIV incidence was 5.7 per 100 person-years (range, 0.8-9.9 per 100 person-years). Effectiveness was −48.8% for TDF; −4.2% for TDF/FTC; and 14.7% for TDF gel. | Adherence to study drugs was low: TFV was detected in 28% of the oral TDF arm, 29% in the oral TDF/FTC arm and 22% in the TDF gel arm |
| HPTN 05287 | 1763 heterosexual serostatus-discordant couples; 50% negative female, 50% negative male partner; 94% married; 61% aged 26-40 yr | Botswana, Kenya, Malawi, South Africa, Zimbabwe, Brazil, India, Thailand | Immediate or delayed antiretroviral therapy in HIV-infected partner | 96% protection | Suppression of viremia on therapy ensured by routine monitoring |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








