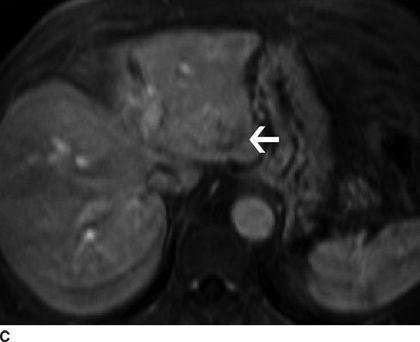
FIGURE 31.1 Hepatocellular carcinoma visualized by multiphasic contrast-enhanced MRI of the liver. A. Arterial phase of the study shows a mass within the left lobe of the liver enhancing earlier than the rest of the liver parenchyma (arrow). Note the prominent intratumoral arterial network. B. Portal venous phase of the examination shows that the mass is relatively hypervascular (arrow) compared to the surrounding liver parenchyma. C. Delayed phase of the study shows that enhancement characteristic of the mass has excreted the contrast earlier than the liver parenchyma and now shows relatively less enhancement (arrow). Early contrast uptake and early contrast clearance is called “washout phenomenon” and is a characteristic of hypervascular malignancies.
Magnetic resonance contrast agents are crucial in liver lesion detection and characterization. There are many MR contrast agents with different properties. Examples of extracellular contrast agents include the gadolinium chelates, gadopentetate dimeglumine (Gd-DTPA) and gadoterate meglumine (Gd-DOTA). These agents function similar to iodinated CT contrast agents by rapidly diffusing from the intravascular space to the extracellular space. Hepatobiliary specific agents such as gadoxatate (Gd-EOB-DTPA) and gadobenate dimeglumine (Gd-BOPTA) increase the signal intensity of the normal liver and hepatocyte-containing lesions such as focal nodular hyperplasia. This increased signal intensity improves the contrast difference between the liver parenchyma and nonhepatocellular lesions (such as metastases) during the delayed phase images.
Positron Emission Tomography Scan
The liver demonstrates diffusely increased fludeoxyglucose (FDG) activity physiologically and is used as a qualitative comparison point for other foci of uptake in the body (e.g., pancreatic and gallbladder lesions). Activity that is equal to or greater than that in the liver raises concern for pathologic processes. Overall, most metastatic tumors are FDG avid and readily detectable using PET–CT. FDG-PET imaging of hepatocellular carcinoma is somewhat limited due to the activity of glucose-6-phosphatase, which is found in varying degrees in this tumor. Hepatocellular carcinoma is more FDG avid than the liver in approximately 55% of cases; it is equal to or less avid in 30% and 15% of cases, respectively. Generally, PET detects only 50% to 70% of hepatocellular carcinomas, but is useful in detection of distant metastases (extrahepatic disease) as well as in evaluation of recurrence. In FDG avid hepatocellular carcinoma, PET–CT imaging is helpful for staging, especially in the assessment of distant metastatic disease.
GALLBLADDER
Ultrasound
Real-time transabdominal sonography is the most widely used diagnostic examination for the gallbladder since it is quick and easy to perform. The gallbladder is visible on sonograms in virtually all fasting patients despite body habitus or clinical condition. The success rate of obtaining a diagnostic study is very high; therefore, ultrasound should be considered as the first line of study for primary gallbladder pathology (Fig. 31.2). The examination can be performed at the bedside and, since no ionizing radiation is used, is safe in pregnant and pediatric patients.

FIGURE 31.2 Abnormal gallbladder by ultrasound. Gray-scale image of the gallbladder and liver is shown. There is a round gallstone (GS) located within the neck of the gallbladder; note the posterior shadowing seen as black. There is abnormal and irregular gallbladder wall thickening (arrow). Comet tail artifacts visualized in the gallbladder wall indicates adenomyomatosis of the gallbladder. This is a diagnosis specifically made by the ultrasound.
Computed Tomography
The gallbladder in fasting patients is nearly always identified on CT scans of the upper abdomen. Although calcified gallstones are frequently visible, CT is not used as a primary examination for detecting gallstones because of its lower sensitivity for gallstones and higher cost compared with ultrasound. The main indication for CT in gallbladder disease is for the diagnosis and staging of gallbladder carcinoma and evaluation of the complications of cholecystitis such as perforation and pericholecystic abscess.
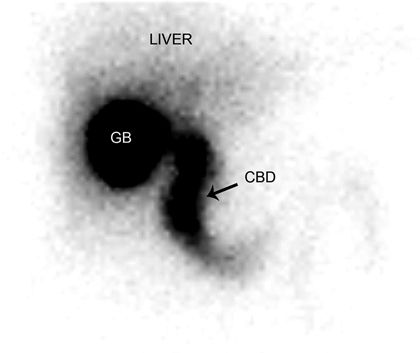
Cholescintigraphy
Cholescintigraphy is used primarily for the diagnosis of acute cholecystitis. This study is performed by injecting Technetium-99m iminodiacetic acid (99m Tc-IDA) compounds intravenously, and the tracer is taken up by the liver and rapidly excreted into bile without undergoing conjugation, allowing visualization of the gallbladder and bile ducts. Serial images are obtained up to 1 hour. Delayed imaging up to 4 hours and possibly 24 hours may be necessary in some instances. Nonfilling of the gallbladder on cholescintigraphy indicates functional obstruction of the cystic duct and is highly sensitive and specific for the diagnosis of acute cholecystitis in the appropriate clinical setting (Fig. 31.3). Other uses for scintigraphic evaluation of the biliary tract include assessment of gallbladder ejection fraction, patency or bile leak after cholecystectomy, or biliary enteric anastomoses. Long-term function of Roux-en-Y biliary–enteric anastomosis may be evaluated by scintigraphy with delayed imaging.