HORMONES
CHEMICAL CLASSIFICATION
Most hormones can be classified into one of several chemical categories: amino-acid derivatives (e.g., tryptophan → serotonin and melatonin; tyrosine → dopamine, norepinephrine, epinephrine, triiodothyronine, and thyroxine; L-glutamic acid → γ-aminobutyric acid; histidine → histamine), peptides or polypeptides (e.g., thyrotropin-releasing hormone, insulin, growth hormone, nerve growth factor), steroids (e.g., progesterone, androgens, estrogens, corticosteroids, vitamin D and its metabolites), and fatty acid derivatives (e.g., prostaglandins, leukotrienes, thromboxanes).
SOURCES, CONTROLS, AND FUNCTIONS
Previously hormones were thought to be synthesized and secreted predominantly by anatomically discrete and circumscribed glandular structures, called ductless glands (e.g., pituitary, thyroid, adrenals, gonads). However, many microscopic organoid-like groups of cells and innumerable other cells of the body contain and secrete hormones (see Chap. 175).
The classic “glands” of endocrinology have lost their exclusivity, and although they are important on physiologic and pathologic levels, the widespread secretion of hormones throughout the body by “nonglandular” tissues is of equal importance. Most hormones are known to have multiple sources. Moreover, the physiologic stimuli that release these hormones are often found to differ according to their locale. The response to a secreted hormone is not stereotyped but varies according to the nature and location of the target cells or tissues.
TRANSPORT
TYPES OF SECRETORY TRANSPORT
Hormones have various means of reaching target cells. In the early decades of the development of the field of endocrinology, hormones were conceived to be substances that traveled to distal sites through the blood. This is accomplished by release into the extracellular spaces and subsequent entrance into blood vessels by way of capillary fenestrations. The most appropriate term for such blood-bone communication is hemocrine (Fig. 1-1).
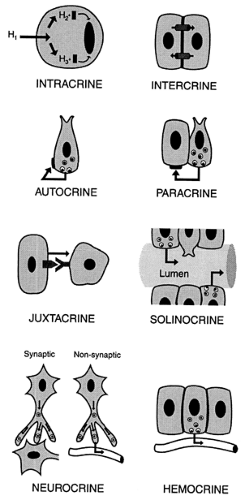 FIGURE 1-1. Different types of hormonal communication detailed in the chapter. The darkened areas on the cell membrane represent receptors. (H, hormone.) See text for explanations. |
Several alternative means of hormonal communication exist, however. Paracrine communication involves the extrusion of hormonal contents into the surrounding interstitial spaces; the hormone then interacts with receptors on nearby cells (see Fig. 1-1 and Chap. 4 and Chap. 175).1 Direct paracrine transfer of cytoplasmic messenger molecules into adjacent cells may occur
through specialized gap junctions (i.e., intercrine secretion).2 Unlike hemocrine secretion, in which the hormonal secretion is diluted within the circulatory system, paracrine secretion delivers a very high concentration of hormone to its target site. Juxtacrine communication occurs when the messenger molecule does not traverse a fluid phase to reach another cell, but, instead, remains associated with the plasma membrane of the signaling cell while acting directly on an immediately adjacent receptor cell (e.g., intercellular signaling that is adhesion dependent and occurs between endothelial cells and leukocytes and transforming growth factor-α in human endometrium).3,4
through specialized gap junctions (i.e., intercrine secretion).2 Unlike hemocrine secretion, in which the hormonal secretion is diluted within the circulatory system, paracrine secretion delivers a very high concentration of hormone to its target site. Juxtacrine communication occurs when the messenger molecule does not traverse a fluid phase to reach another cell, but, instead, remains associated with the plasma membrane of the signaling cell while acting directly on an immediately adjacent receptor cell (e.g., intercellular signaling that is adhesion dependent and occurs between endothelial cells and leukocytes and transforming growth factor-α in human endometrium).3,4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree