(1)
State University of New York at Buffalo Kaleida Health, Buffalo, NY, USA
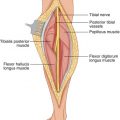
In patients with carcinoma of the common hepatic duct close to the junction of the right and left hepatic ducts, wide resection of this area of tumor includes dissection in the hepatic parenchyma, with removal of a portion of the right and left hepatic ducts. The result is a situation of two or three hepatic duct openings from each lobe of the liver visible within the excavated area of the porta hepatis. Duct-to-mucosa anastomosis is the preferred method of constructing a safe anastomosis between a biliary duct and a Roux-en-Y loop of the jejunum. If there are only two hepatic ducts (right and left) at the depth of the wound in the porta hepatis, it is not difficult to perform an individual duct-to-mucosa anastomosis to a Roux-en-Y loop for these two ducts. If multiple hepatic duct openings are exposed, however, it is not possible to perform an individual duct-to-mucosa anastomosis with each opening. This situation occurs either when the tumor is early and is confined in the lumen of the common hepatic duct or when it protrudes only anterior to the hepatic duct, so that a minimal anterior dissection and removal of hepatic tissue around the tumor is necessary. In this instance, the tumor is not protruding into adjacent tissues posterior to the hepatic duct, where the hepatic artery and the portal vein are located (Fig. 26.1).
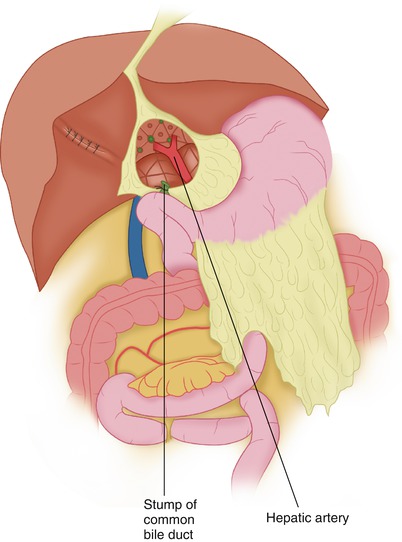
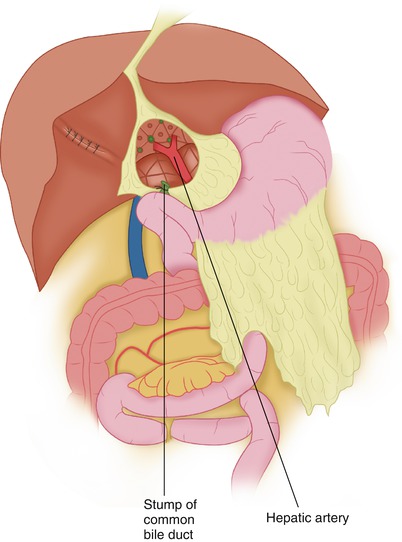
Fig. 26.1
Multiple ductal openings are visible in the cored-out hepatic parenchyma at the porta hepatis
In these cases, a Roux-en-Y loop may be used, which is sutured to Glisson’s capsule and fibrous tissue around the excavated area of the porta hepatis by making an anastomosis between this edge and a suitable opening in the antimesenteric border of the Roux-en-Y loop. Absorbable or nonabsorbable material may be used, with the knots on the inside for the posterior row (Fig. 26.2) and the knots on the outside for the anterior row, to facilitate an accurate and secure tying of the knots. If nonabsorbable material is used, stone formation does not seem to be a problem in such a wide-lumen anastomosis. There is no need to place stents within each of the exposed smaller hepatic ducts as long as the hepatic ducts have been cut flush with the hepatic parenchyma, thus avoiding the protrusion of devitalized hepatic duct wall, which may collapse (lacking support) and scar over time. Drains are placed at the foramen of Winslow near the anastomosis, to provide ample drainage of any bile that may leak from the recent anastomosis over the first few postoperative days. The bile leak usually stops after a few days, and the patient’s postoperative course is generally unremarkable.