The herpes viruses are responsible for a wide range of diseases in patients following transplant, resulting from direct viral effects and indirect effects, including tumor promotion. Effective treatments and prophylaxis exist for the neurotropic herpes viruses HSV-1, HSV-2, varicella zoster virus, and possibly HHV-6. Antivirals seem to be less effective at prevention of the tumor-promoting effects of Epstein-Barr virus and HHV-8. Reduction in immunosuppression is the cornerstone to treatment of many diseases associated with herpes virus infections.
The herpes viruses comprise a large group of enveloped DNA-containing viruses that characteristically cause latent infection in their respective hosts. There are 8 known herpes family viruses associated with human infection: herpes simplex virus (HSV) types 1 and 2, varicella zoster virus (VZV), Epstein-Barr virus (EBV), Cytomegalovirus (CMV), Human herpesvirus 6 (HHV-6), Human herpesvirus 7 (HHV-7), and Human herpesvirus 8 (HHV-8). Of these, CMV has received the most attention as a cause of morbidity and mortality among transplant recipients and is discussed separately in articles by Ljungman, Strasfeld, Hirsch, and Einsele in this issue. The remaining herpes viruses are also responsible for significant disease in the transplant patient population. The role of each of these viruses as a cause of disease in the transplant population is discussed in this article.
HSV-1 and HSV-2
The α-herpes viruses, HSV-1 and HSV-2, are responsible for oral and genital mucocutaneous ulcers in the general population. HSV-2 is generally considered to be sexually transmitted and primarily infects the urogenital mucosa, whereas HSV-1 predominantly affects the oral mucosa and is often transmitted through nonsexual contact. Both viruses are neurotropic and primarily infect neurons in their latent forms. Reactivation of HSV is common among transplant recipients, and is the second most common cause of viral infection after transplantation.
Most HSV-1 and HSV-2 infections occur in the setting of reactivation rather than primary infection, although primary HSV infections are well documented, particularly among younger patients. Primary infection from transplanted tissue is uncommon but has been observed in renal transplant recipients. The high percentage of cases attributed to reactivation is undoubtedly a result of a high baseline population seroprevalence of HSV-1 and HSV-2. Seroprevalence increases with age and varies by geographic, racial, socioeconomic, and ethnic characteristics among the general population. Antibodies to HSV-1 were found in 50% to 96% of people in previous seroprevalence studies. Analysis of Americans from the National Health and Nutrition Examination Survey showed the seroprevalence of HSV-1 to be 65% and HSV-2 to be 26% by age 49 years. Higher rates of seropositivity were found in women and minorities in the same survey. The greatest risk factor for reactivation of HSV following transplantation is lack of antiviral prophylaxis.
Before the introduction of acyclovir, reactivation of HSV infection was estimated to occur in up to 80% of patients receiving hematopoetic stem cell transplant. Lower, but still substantial, reactivation rates were described in solid-organ transplant recipients in the years before effective antiviral prophylaxis. The clinical manifestations of HSV infection range from limited mucocutaneous outbreaks to disseminated infections involving visceral organs and the central nervous system (CNS).
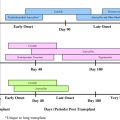
The most common manifestations of HSV are mucocutaneous outbreaks, usually involving the oral and genitourinary mucosa. These infections, which can lead to extensive mucosal involvement, typically occur in the first 30 days following transplantation if prophylaxis is not administered. Less common manifestations of HSV involving the lungs and viscera are also described. Pneumonia as a result of HSV-1 and HSV-2 is typically preceded by gingivostomatitis, however pulmonary involvement from disseminated infection and airway manipulation may also occur. The diagnosis of HSV pneumonia is complicated because viral shedding within the airways is common in immunosuppressed and critically ill adults and does not necessarily reflect true pneumonia. The use of acyclovir in critically ill patients with HSV isolated from respiratory secretions has not been shown to influence mortality, ventilator dependence, or length of hospitalization. Therefore, caution should be taken in interpreting results from viral cultures, direct fluorescent antibody staining, and nucleic acid assays without associated cytopathic evidence of infection on tissue biopsy.
Hepatitis is an uncommon manifestation of HSV that is described in several case reports and case series. When HSV presents with hepatitis there is often evidence of disseminated disease with involvement of the skin and mucous membranes. Patients may seem well initially, with elevated liver function tests as the only sign of infection. More often, patients present with nonspecific flulike symptoms of fever, malaise, and myalgias. Increasing levels of aspartate aminotransferase and alanine aminotransferase, sometimes 10 to 20 times the upper limit of normal, are often observed. Cross-sectional imaging may appear normal, but in some cases liver infiltration with microabscesses has been observed. Most cases occur within 30 days of transplant, however some cases have occurred years after transplant. Nearly all HSV hepatitis cases in the literature occurred in patients while off antiviral prophylaxis. Diagnosis is made by liver biopsy with culture and antibody staining for HSV-1 and HSV-2. Pathology typically reveals necrotic hepatitis with loss of lobular architecture. Other visceral manifestations of HSV infection in immunosuppressed hosts include esophagitis, gastritis, and colitis.
Encephalitis as a result of HSV infection is rare in the transplant population. On presentation, confusion, fever, and behavioral changes are the predominant findings. Up to one-third of patients present with seizure and one-fifth with focal neurologic findings. Cerebrospinal fluid (CSF) typically has a lymphocytic pleocytosis and increased protein level. The diagnosis of HSV encephalitis is now usually made by polymerase chain reaction (PCR) from CSF rather than brain biopsy. In the general population, on which most research on HSV encephalitis has been conducted, significant neurologic compromise is common following HSV encephalitis. The early initiation of high-dose acyclovir was shown to significantly decrease the morbidity and mortality from HSV encephalitis. In a large cohort of immunocompetent and immunosuppressed patients, long-term neurologic deficits were common despite antiviral treatment. There are insufficient data in the era of antiviral prophylaxis to know if outcomes are worse in transplant recipients.
The introduction of oral and intravenous acyclovir in the 1980s markedly decreased the incidence of serious HSV infections following transplantation. Several small randomized trials demonstrated intravenous and oral acyclovir to be safe and effective as a prophylactic regimen against HSV infections. Acyclovir appeared to abbreviate viral shedding and expedite healing from mucocutaneous outbreaks in hematopoetic stem cell transplant recipients. Since the introduction of acyclovir, related compounds such as valacyclovir and famciclovir have also been used successfully for treatment of HSV and varicella zoster infections following transplantation. Ganciclovir also has activity against HSV, and its use in the posttransplant population has been shown to significantly decrease rates of reactivation. Resistance to acyclovir and its derivatives does occur and typically reflects prolonged exposure to inadequate dosing of acyclovir at the time of viral reactivation. The highest rates of acyclovir resistance are found in allogeneic stem cell transplant recipients with estimates ranging from 1% to 14% of patients with resistant virus. Second-line treatment with foscarnet is typically used if acyclovir resistance is detected.
VZV
VZV, the α-herpes virus responsible for chickenpox and shingles, causes symptomatic infection through reactivation or primary infection in approximately 1% to 20% of solid-organ transplant recipients, with lung transplant recipients having the highest rates. The rate of VZV disease approaches more than 40% in hematopoetic stem cell transplant recipients. Reactivation of VZV is the most common route of VZV disease in adult transplant recipients, with more than 90% of adults in the United States estimated to have antibodies against VZV. In previous series, the median time frame for reactivation ranged from 9 to 23 months following solid-organ transplant. In hematopoietic cell transplant recipients most cases of VZV disease tends to occur within the first 12 months following transplantation, with up to 26% of transplant recipients developing disease following discontinuation of antiviral prophylaxis. Suggested risk factors for VZV disease in solid-organ transplant include mycophenolate use, recent treatment of rejection, induction therapy, and age greater than 50 years. All solid-organ transplant candidates should be tested before transplantation for VZV antibodies in an effort to determine the risk for primary infection. Solid-organ transplant candidates with VZV IgG negative status should undergo vaccination with the live attenuated Oka strain VZV vaccine before solid-organ transplant. The vaccine should not be given after transplant because it is a live vaccine and there are currently insufficient data to determine its safety in immunosuppressed transplant recipients. The rate of VZV disease (primary and reactivation) in allogeneic stem cell transplant recipients remains high regardless of VZV serostatus before transplant. An investigational inactivated varicella vaccine was successfully used to prevent disease in autologous hematopoetic stem cell transplant recipients; however it is currently not available.
As with HSV, the clinical manifestations of VZV disease are wide ranging, but can be severe and associated with increased mortality, especially in the early posttransplant period. Primary infection with VZV in the posttransplant setting can be severe, with disseminated infection presenting with skin, lung, and visceral organ involvement. Donor-derived VZV infections are rare, but have been reported. The most common presentation of VZV is cutaneous infection, typically with single dermatomal involvement. However, multiple dermatome involvement occurs in a sizable minority of cases. In cases of disseminated disease, typical vesicular skin lesions remain a common marker of disease. It is notable that the rash is not always vesicular in immunosuppressed hosts; consequently biopsy of the skin may be required for viral identification either by direct fluorescence or nucleic acid detection or culture. Patients may present with other symptoms of disseminated disease, including abdominal pain or hepatitis before the onset of rash. CNS involvement with VZV can present with encephalitis, myelitis, or meningoencephalitis. Unlike disseminated cutaneous infections, CNS VZV often presents without skin or other organ involvement. The diagnosis of VZV CNS infection is typically made by detection of VZV in the CSF using nucleic acid testing in conjunction with a compatible clinical presentation. CSF typically shows a lymphocyte predominant pleocytosis, moderately increased protein level and normal to low-normal glucose level. All cases of disseminated zoster should be placed in isolation once the diagnosis is suspected in an effort to prevent spread to other immunocompromised patients and susceptible health care workers.
Treatment of VZV disease is generally recommended for all transplant recipients. High-dose acyclovir or its analogues has been successfully used for the treatment of localized and disseminated VZV infections. In cases of disseminated disease and CNS infection, intravenous acyclovir (30 mg/kg/d in 3 divided doses) is preferred as initial therapy. Ganciclovir has not been studied specifically in the treatment of VZV, however it has been used successfully for treatment in several reports. Oral agents, such as valacyclovir (1 g every 8 hours), acyclovir (800 mg 5 times each day) and famciclovir (500 mg every 8 hours) are reasonable choices for localized infections. In rare cases where acyclovir resistance occurs, foscarnet can be used.
Several studies have shown acyclovir and ganciclovir to be effective as prophylaxis against VZV reactivation in the posttransplant period. Other methods of preventing primary infection in VZV-negative transplant recipients (who were not vaccinated before transplant or failed to mount a detectable VZV antibody titer) include vaccinating household and close contacts at risk for primary infection, preferably before transplant. VZV seronegative patients exposed to persons with active VZV (either chicken pox or shingles) should ideally be given postexposure prophylaxis with intravenous varicella zoster immunoglobulin (VZIG) given within the first 96 hours of exposure. Unfortunately, VZIG is no longer available in the United States. An intramuscularly dosed formulation of concentrated VZV IgG (VariZIG, Cangene Corp, Winnepeg, Canada) is available through an investigational new drug expanded access protocol from the Food and Drug Administration ( http://www.fda.gov/BiologicsBloodVaccines/SafetyAvailability/ucm176029.htm ). There are currently insufficient data to support the use of antiviral agents after VZV exposure, and it is currently not recommended by the Centers of Disease Control’s Advisory Committee on Immunization Practices.
VZV
VZV, the α-herpes virus responsible for chickenpox and shingles, causes symptomatic infection through reactivation or primary infection in approximately 1% to 20% of solid-organ transplant recipients, with lung transplant recipients having the highest rates. The rate of VZV disease approaches more than 40% in hematopoetic stem cell transplant recipients. Reactivation of VZV is the most common route of VZV disease in adult transplant recipients, with more than 90% of adults in the United States estimated to have antibodies against VZV. In previous series, the median time frame for reactivation ranged from 9 to 23 months following solid-organ transplant. In hematopoietic cell transplant recipients most cases of VZV disease tends to occur within the first 12 months following transplantation, with up to 26% of transplant recipients developing disease following discontinuation of antiviral prophylaxis. Suggested risk factors for VZV disease in solid-organ transplant include mycophenolate use, recent treatment of rejection, induction therapy, and age greater than 50 years. All solid-organ transplant candidates should be tested before transplantation for VZV antibodies in an effort to determine the risk for primary infection. Solid-organ transplant candidates with VZV IgG negative status should undergo vaccination with the live attenuated Oka strain VZV vaccine before solid-organ transplant. The vaccine should not be given after transplant because it is a live vaccine and there are currently insufficient data to determine its safety in immunosuppressed transplant recipients. The rate of VZV disease (primary and reactivation) in allogeneic stem cell transplant recipients remains high regardless of VZV serostatus before transplant. An investigational inactivated varicella vaccine was successfully used to prevent disease in autologous hematopoetic stem cell transplant recipients; however it is currently not available.
As with HSV, the clinical manifestations of VZV disease are wide ranging, but can be severe and associated with increased mortality, especially in the early posttransplant period. Primary infection with VZV in the posttransplant setting can be severe, with disseminated infection presenting with skin, lung, and visceral organ involvement. Donor-derived VZV infections are rare, but have been reported. The most common presentation of VZV is cutaneous infection, typically with single dermatomal involvement. However, multiple dermatome involvement occurs in a sizable minority of cases. In cases of disseminated disease, typical vesicular skin lesions remain a common marker of disease. It is notable that the rash is not always vesicular in immunosuppressed hosts; consequently biopsy of the skin may be required for viral identification either by direct fluorescence or nucleic acid detection or culture. Patients may present with other symptoms of disseminated disease, including abdominal pain or hepatitis before the onset of rash. CNS involvement with VZV can present with encephalitis, myelitis, or meningoencephalitis. Unlike disseminated cutaneous infections, CNS VZV often presents without skin or other organ involvement. The diagnosis of VZV CNS infection is typically made by detection of VZV in the CSF using nucleic acid testing in conjunction with a compatible clinical presentation. CSF typically shows a lymphocyte predominant pleocytosis, moderately increased protein level and normal to low-normal glucose level. All cases of disseminated zoster should be placed in isolation once the diagnosis is suspected in an effort to prevent spread to other immunocompromised patients and susceptible health care workers.
Treatment of VZV disease is generally recommended for all transplant recipients. High-dose acyclovir or its analogues has been successfully used for the treatment of localized and disseminated VZV infections. In cases of disseminated disease and CNS infection, intravenous acyclovir (30 mg/kg/d in 3 divided doses) is preferred as initial therapy. Ganciclovir has not been studied specifically in the treatment of VZV, however it has been used successfully for treatment in several reports. Oral agents, such as valacyclovir (1 g every 8 hours), acyclovir (800 mg 5 times each day) and famciclovir (500 mg every 8 hours) are reasonable choices for localized infections. In rare cases where acyclovir resistance occurs, foscarnet can be used.
Several studies have shown acyclovir and ganciclovir to be effective as prophylaxis against VZV reactivation in the posttransplant period. Other methods of preventing primary infection in VZV-negative transplant recipients (who were not vaccinated before transplant or failed to mount a detectable VZV antibody titer) include vaccinating household and close contacts at risk for primary infection, preferably before transplant. VZV seronegative patients exposed to persons with active VZV (either chicken pox or shingles) should ideally be given postexposure prophylaxis with intravenous varicella zoster immunoglobulin (VZIG) given within the first 96 hours of exposure. Unfortunately, VZIG is no longer available in the United States. An intramuscularly dosed formulation of concentrated VZV IgG (VariZIG, Cangene Corp, Winnepeg, Canada) is available through an investigational new drug expanded access protocol from the Food and Drug Administration ( http://www.fda.gov/BiologicsBloodVaccines/SafetyAvailability/ucm176029.htm ). There are currently insufficient data to support the use of antiviral agents after VZV exposure, and it is currently not recommended by the Centers of Disease Control’s Advisory Committee on Immunization Practices.
EBV
EBV is a gammaherpes virus responsible for several clinical entities. In the general population, EBV is the causative agent of infectious mononucleosis, Burkitt lymphoma, and nasopharyngeal carcinoma. The role of EBV as a cause of posttransplant lymphoproliferative disorder (PTLD) is now well established, accounting for 90% of cases of PTLD. Other rare disorders attributed to EBV in the posttransplant period include smooth muscle tumors and the hemophagocytic syndrome. EBV is ubiquitous, with up to 90% seropositivity observed in the general community. Infection in early childhood is common and often without significant symptoms. The clinical entity of mononucleosis, characterized by pharyngitis, lymphadenopathy, and fatigue, is typically seen with primary infection in young immunocompetent adults. Rarely, neurologic manifestations of EBV infection, including encephalitis and optic neuritis, occur. Like other herpes viruses, EBV is a chronic infection, with latent virus infecting B cells in the blood and lymphoid tissues. The virus is typically transmitted to naive individuals through saliva and respiratory secretions. Transmissions to naive transplant recipients through blood transfusion and organ transplant are also described.
The clinical entity known as PTLD comprises a spectrum of disease characterized by the abnormal proliferation of lymphocytic cells, often with an invasive component, in patients following transplantation. The clinical manifestations of PTLD vary considerably. In some instances patients are asymptomatic and disease is only suggested by incidental imaging findings. Other cases may present with a mononucleosis-like syndrome, organ dysfunction secondary to tissue infiltration or septic-appearing febrile illness. Tissue infiltration from PTLD may present as extranodal masses, which can involve various organs, including the lungs, liver, spleen, bowels, and CNS. In some instances, allografts are the primary site of PTLD, with resulting organ dysfunction mimicking rejection. PTLD may present as an infiltrative process rather than a focal mass, mimicking such entities as pneumonia, lymphocele, and colitis.
Numerous risk factors for the development of PTLD are described. Host EBV seronegative status has been shown to increase the risk of developing PTLD up to 76-fold, making the issue particularly troublesome for pediatric patients. These patients, at risk for primary EBV infection, are most likely to present with disease within only a few months of transplant. Other risk factors in solid-organ transplant recipients, reflect a state of actual or potentially augmented immune suppression and include CMV disease, CMV donor/recipient mismatch, and intensity of pharmacologically mediated immune suppression. Risk factors for PTLD in hematopoetic stem cell recipients include unrelated donor HLA mismatch, use of antithymocyte globulin, T-cell depletion, and use of anti-CD3 monoclonal antibodies for graft-versus-host disease prophylaxis.
The initial diagnosis of PTLD is best made with tissue, ideally from an excisional biopsy specimen. High serum levels of EBV DNA may be seen in PTLD, especially in younger recipients, and may precede clinical disease. Currently, the incongruity in EBV DNA testing methods between centers and the need for tissue for pathologic grading, argue against the use of EBV viral load testing as replacement for histologic diagnosis, although it is estimated that up to 90% of PTLD is EBV-associated. The Society of Hematopathology classification schema for PTLD divides lesions into 3 general categories: lymphoid hyperplasia (early lesions), polymorphic PTLD, and lymphomatous (monomorphic) PTLD. Lymphoid hyperplasia, sometimes referred to as early PTLD, is subcharacterized into posttransplant infectious mononucleosis and reactive plasmacytic hyperplasia. A notable characteristic in both of these groups is the presence of polyclonal cell populations. Polymorphic PTLD is characterized by more aggressive lesions that escape the normal lymphatic system boundaries and infiltrate underlying tissue. Although these lesions behave similarly to malignant lymphoma, the cell population involved remains heterogeneous in appearance, although they are all typically monoclonal at the molecular level. The term monomorphic PTLD is used to describe lymphomas in the posttransplant setting. Many are associated with EBV, although some are not. These lesions are generally categorized according to the Revised European American Lymphoma system with the suffix PTLD to note the correlation with transplant status.
Treatment varies considerably depending on which variation of PTLD is diagnosed. A cornerstone of therapy is decreasing the level of immunosuppression whenever possible. In 1 series of solid-organ transplant recipients treated for PTLD, 63% of patients treated by reducing immunosuppression alone had complete disease remission. Risk factors for failing treatment with reduction of immunosuppression included a high baseline lactate dehydrogenase level, multiorgan involvement, presence of B symptoms, and organ dysfunction from disease. The data for antiviral medications in the treatment of PTLD through suppression of EBV are limited. Although early reports suggested acyclovir and ganciclovir, which have some in vitro activity against EBV, might have a potential role in PTLD treatment there is no compelling clinical data to support their use. Treatment with immunomodulatory agents such as anti-CD-20 (rituximab), interleukin 6 (IL-6) and interferon-α is described. Infusions of cytotoxic EBV-specific T cells have also been used as a therapeutic and prophylactic treatment in solid-organ and hematopoetic stem cell transplant recipients. As a treatment, results have been mixed and no controlled trials have been published on the subject. The use of cytotoxic EBV-specific T cells as a prophylactic measure in individuals with high levels of circulating EBV DNA were also reported to be beneficial, but data are limited to small uncontrolled series. In some cases treatment with chemotherapeutic agents used in nontransplant-associated lymphomas are also used, often in conjunction with rituximab. Other strategies include resection of localized tumors, radiotherapy, and treatment of other infections, such as CMV, that may act to suppress the immune system further. In cases where reduction of immunosuppression has resulted in graft loss, retransplantation can be successful.
The use of antivirals gained some support as a prophylactic measure against EBV based on the results of some uncontrolled studies. A randomized controlled trial exploring the use of ganciclovir and acyclovir as a prophylactic strategy for EBV and CMV did not show any decrease in PTLD, however. The use of quantitative EBV viral load monitoring has been advocated as another method to prevent the development of PTLD in high-risk individuals. In this approach regular quantitative EBV viral loads are obtained and immunosuppression is decreased when viral loads reach a predetermined threshold.
HHV-6 and HHV-7
HHV-6, the causative agent of the common childhood disease roseola infantum (exanthem sabitum), has received attention in the past several years as an opportunistic infection in the posttransplant population. The virus, first described in 1986, is a member of the β-herpes virus family, and establishes latency in CD4+ T lymphocytes. Genetic sequencing has demonstrated 2 variants, A and B. The B variant has been linked to most disease in children and in the transplant population. It is estimated that greater than 90% of children are seropositive for HHV-6 by 1 year of age. Therefore, most cases of HHV-6 viremia are believed to be caused by viral reactivation, although primary infection following transplantation has been described.
Reactivation of HHV-6 is common in the immediate period following hematopoetic stem cell transplant, when immunosuppression is highest. A prospective study by Zerr and colleagues detected HHV-6 viremia in 52 of 110 (47%) patients evaluated during the first 100 days after transplant. Numerous indirect effects have been suggested related to HHV-6 viremia in the hematopoetic stem cell transplant population. These include delayed engraftment, higher rates of graft-versus-host disease, cytomegalovirus disease, and all-cause mortality. Estimates of HHV-6 viremia following solid-organ transplant range from 24% to 66%, although this is likely reduced in patients receiving ganciclovir for CMV prophylaxis. Reported indirect effects associated with HHV-6 viremia include higher frequencies of allograft rejection, severe CMV disease, and invasive fungal infections. Despite these associations, no causal link has been definitively established between HHV-6 reactivation and indirect effects. A recent prospective cohort study that included 298 solid-organ transplant recipients found no connection between severity or duration of CMV disease and HHV-6 coinfection.
Several case series and reports have linked HHV-6 with encephalitis in solid-organ and hematopoetic stem cell transplant recipients. Most of the cases reported in the literature occurred 30 to 90 days after transplant. Manifestations of neurologic disease include generalized confusion, amnesia, insomnia, seizures (often subclinical), and coma. Magnetic resonance imaging imaging of the brain often reveals involvement of the basal ganglia. The detection of HHV-6 in CSF through PCR or culture, in conjunction with compatible neuroradiology and clinical manifestations, is highly suggestive of HHV-6 encephalitis. Nonetheless, other causes of encephalitis should be ruled out as HHV-6 has been detected in the CSF of asymptomatic patients and the symptoms of HHV-6 encephalitis may be strikingly similar to those of immunosuppression leukoencephalopathy. Other manifestations of HHV-6 disease reported in the literature include gastroenteritis, pneumonitis, hepatitis, and myelosuppression.
No prospective clinical trials have evaluated the use of antiviral medications in the treatment of HHV-6 associated disease. In vitro data suggest that HHV-6 is inhibited by ganciclovir, foscarnet, and cidofovir. Most clinical experience has been with the treatment of HHV-6 encephalitis. Most reported cases used ganciclovir, foscarnet, or a combination of both with varying success. Despite their in vitro activity against HHV-6, neither intravenous ganciclovir nor valganciclovir affected HHV-6 viral loads in a multicenter prospective clinical trial of CMV disease treatment.
The β-herpes virus, HHV-7, is closely related to HHV-6 but its role in clinically relevant disease remains unclear. In children, HHV-7 has been associated with rare cases of exanthem subitum, febrile seizures, and encephalitis. A few cases of encephalitis and myelitis have been attributed to HHV-7 among hematopoetic stem cell transplant recipients. In comparison with HHV-6, however, little data exist supporting organ-specific infections with HHV-7 in transplant recipients. Like HHV-6, HHV-7 has been proposed to act as an immunomodulatory virus, potentially lowering the barrier to other opportunistic infections, including CMV. A recent prospective multicenter cohort examined the effect of HHV-7 viremia in patients with diagnosed CMV disease and found no correlation with duration of CMV disease or CMV disease outcomes.
HHV-8
HHV-8 also known as Kaposi sarcoma–associated herpes virus, is responsible for the malignant entities of Kaposi sarcoma (KS) and primary effusion lymphoma (PEL), as well as some forms of multicentric Castleman disease (MCD). HHV-8 belongs to the γ-herpes virus family along with EBV and infects CD-19 positive B cells in its latent form. Unlike the other herpes viruses discussed earlier, the seroprevalence to HHV-8 is highly variable, depending on geography and behavioral risk factors. Of 13,984 Americans sampled in the National Health and Nutrition Survey, 1.5% were found to be seropositive for HHV-8. The highest rate of HHV-8 seropositivity in the United States was found in men who have sex with men, with a prevalence rate estimated to be 8.2%. Worldwide prevalence varies dramatically, with some areas of sub-Saharan Africa estimated to have 30% to 50% seropositivity.
Transmission of HHV-8 is believed to occur through sexual activity and possibly through saliva. In endemic regions both means of transmission probably occur. Elsewhere, such as in North America, sexual activity is believed to be the primary mode of transmission. Transmission of HHV-8 has also been documented through solid-organ and hematopoetic stem cell transplantation.
Manifestations of HHV-8 disease in transplant recipients are variable. In the Middle East, where seroprevalence for HHV-8 reaches 25%, KS is the most common malignancy following renal transplant. The incidence is lower in North America. Prior series describing KS following solid-organ transplant reported onset of disease ranging from 2 to 23 months after transplant. Lesions may present as focal nodules on the skin, within organs (including allografts), or as disseminated disease with lymph node, bone marrow, and splenic infiltration. The diagnosis of KS is made by pathologic examination of affected tissues.
As with EBV-associated PTLD, reduction in immunosuppression is the first-line therapy for KS and is often curative. Some investigators have suggested that using sirolimus instead of other calcineurin inhibitors may provide additional treatment effect by inhibition of vascular endothelial cell growth factor. Chemotherapy and radiation may also be necessary in cases where reduction of immunosuppression is ineffective or not possible. Antiviral medications have not been shown to be useful in the treatment of KS.
Other rare manifestations of HHV-8 reported in transplant recipients include MCD and PEL. MCD is an aggressive lymphoproliferative disorder characterized by fever, diffuse lymphadenopathy, wasting, and hepatosplenomegally. HHV-8 is not always found in MCD, but is common, with virus detected in 75% of MCD lesions in 1 series. The diagnosis of MCD is made by tissue biopsy. Other causes of diffuse lymphadenopathy, such as disseminated mycobacterial and fungal infections, should be ruled out. The reported outcomes of MCD in transplant recipients are poor, with rapidly fatal disease or allograft failure in several reports. Treatments with immunomodulatory agents, chemotherapy, and antivirals have all been used with variable results.
PEL, also known as body cavity lymphoma, typically presents with a refractory exudative effusion in 1 of several potential spaces within the body. Lymphomatous cells fill the affected cavity, with tumor foci often studding the serous membranes. The most frequent location is the pleural space, however pericardial, peritoneal, and intracranial cases are also reported. Diagnosis is made by pathologic evaluation of effusion cells. HHV-8 PCR of the effusion may also be helpful in making a diagnosis. Other causes of exudative effusions should be ruled out, including infectious entities such as tuberculosis and empyema. Treatment experience of transplant-associated PEL is limited. Reduction in immunosuppression may be useful, as with KS and MCD. Antivirals have not been shown to offer much benefit and chemotherapy remains the treatment of choice in most cases.
Summary
The herpes viruses are responsible for a wide range of diseases in patients following transplant. The development of effective antiviral prophylaxis against HSV and VZV has substantially reduced the morbidity and mortality associated with these infections. Nonetheless, primary disease and reactivation of HSV and VZV can cause significant harm if not treated promptly. The role of EBV as a major cause of PTLD continues to pose a significant challenge. Current therapies focus on reduction of immunosuppression, chemotherapy, and rituximab therapy. There are few data to support antiviral therapy for EBV-associated PTLD, however ganciclovir may have a prophylactic effect, either by indirect or direct means. HHV-6 and -7 may have several indirect effects on transplant patients, including increased risk of infections and rejection episodes. These effects may be related to the viruses’ effect on immune cell function. The evidence for HHV-6 as a cause of posttransplant encephalitis is growing. Treatment with ganciclovir and/or foscarnet may be beneficial. The role of HHV-8 in posttransplant KS is well established. Reduction in immune suppression is the mainstay of therapy; in some cases alteration of immunosuppression to include sirolimus may be effective. Other manifestations of HHV-8 infection, including PEL and MCD may require chemotherapy in conjunction with reduction in immunosuppression. Antivirals have not been shown to be beneficial in the treatment of KS or PEL.
Dr Shiley has no financial disclosures.
Dr Blumberg receives financial support from Roche Pharmaceuticals for research support and consulting services. She also receives research support from Viropharma as a site investigator in a multicenter trial.
A version of this article was previously published in the Infectious Disease Clinics of North America , 24:2.
References
- 1. Balfour H.H., Chace B.A., Stapleton J.T., et al: A randomized, placebo-controlled trial of oral acyclovir for the prevention of cytomegalovirus disease in recipients of renal allografts. N Engl J Med 1989; 320: pp. 1381-1387
- 2. Snydman D.R.: Epidemiology of infections after solid-organ transplantation. Clin Infect Dis 2001; 33: pp. S5-S8
- 3. Montoya J., Giraldo L., Efron B., et al: Infectious complications among 620 consecutive heart transplant patients at Stanford University Medical Center. Clin Infect Dis 2001; 33: pp. 629-640
- 4. Singh N., Dummer J.S., Kusne S., et al: Infections with cytomegalovirus and other herpesviruses in 121 liver transplant recipients: transmission by donated organ and the effect of OKT3 antibodies. J Infect Dis 1988; 158: pp. 124-131
- 5. Dummer J.S., Armstrong J., Somers J., et al: Transmission of infection with herpes simplex virus by renal transplantation. J Infect Dis 1987; 155: pp. 202-206
- 6. Koneru B., Tzakis A.G., DePuydt L.E., et al: Transmission of fatal herpes simplex infection through renal transplantation. Transplantation 1988; 45: pp. 653-656
- 7. Malkin J.: Epidemiology of genital herpes simplex virus infection in developed countries. Herpes 2004; 11: pp. 24
- 8. Malkin J., Morand P., and Malvy D.: Seroprevalence of HSV-1 and HSV-2 in the general French population. Sex Transm Dis 2002; 78: pp. 201-203
- 9. Vyse A., Gay N., and Slomka M.: The burden of infection with HSV-1 and HSV-2 in England and Wales: implications for the changing epidemiology of genital herpes. Sex Transm Dis 2000; 76: pp. 183-187
- 10. Xu F., Sternberg M.R., Kottiri B.J., et al: Trends in herpes simplex virus type 1 and type 2 seroprevalence in the United States. JAMA 2006; 296: pp. 964-973
- 11. Gane E., Saliba F., Valdecasas G.J., et al: Randomised trial of efficacy and safety of oral ganciclovir in the prevention of cytomegalovirus disease in liver-transplant recipients. The Oral Ganciclovir International Transplantation Study Group. Lancet 1997; 350: pp. 1729-1733
- 12. Lowance D., Neumayer H.H., Legendre C.M., et al: Valacyclovir for the prevention of cytomegalovirus disease after renal transplantation. International Valacyclovir Cytomegalovirus Prophylaxis Transplantation Study Group. N Engl J Med 1999; 340: pp. 1462-1470
- 13. Meyers J.D., Flournoy N., and Thomas E.D.: Infection with herpes simplex virus and cell-mediated immunity after marrow transplant. J Infect Dis 1980; 142: pp. 338-346
- 14. Meyers J.D., Wade J.C., Mitchell C.D., et al: Multicenter collaborative trial of intravenous acyclovir for treatment of mucocutaneous herpes simplex virus infection in the immunocompromised host. Am J Med 1982; 73: pp. 229-235
- 15. Saral R., Burns W.H., Laskin O.L., et al: Acyclovir prophylaxis of herpes-simplex-virus infections. N Engl J Med 1981; 305: pp. 63-67
- 16. Seale L., Jones C.J., Kathpalia S., et al: Prevention of herpesvirus infections in renal allograft recipients by low-dose oral acyclovir. JAMA 1985; 254: pp. 3435-3438
- 17. Kusne S., Schwartz M., Breinig M.K., et al: Herpes simplex virus hepatitis after solid organ transplantation in adults. J Infect Dis 1991; 163: pp. 1001-1007
- 18. Pettersson E., Hovi T., Ahonen J., et al: Prophylactic oral acyclovir after renal transplantation. Transplantation 1985; 39: pp. 279-281
- 19. Naraqi S., Jackson G.G., Jonasson O., et al: Prospective study of prevalence, incidence, and source of herpesvirus infections in patients with renal allografts. J Infect Dis 1977; 136: pp. 531-540
- 20. Corey L.: Herpes simplex virus. In Mandell G., Bennett J., and Dolin R. (eds): , 6th edition. Philadelphia (PA): Elsevier, 2005. pp. 1762-1780
- 21. Hann I.M., Prentice H.G., Blacklock H.A., et al: Acyclovir prophylaxis against herpes virus infections in severely immunocompromised patients: randomised double blind trial. Br Med J (Clin Res Ed) 1983; 287: pp. 384-388
- 22. Buss D.H., and Scharyj M.: Herpesvirus infection of the esophagus and other visceral organs in adults. Incidence and clinical significance. Am J Med 1979; 66: pp. 457-462
- 23. Cunha B.A., Eisenstein L.E., Dillard T., et al: Herpes simplex virus (HSV) pneumonia in a heart transplant: diagnosis and therapy. Heart Lung 2007; 36: pp. 72-78
- 24. Herout V., Vortel V., and Vondrackova A.: Herpes simplex involvement of the lower respiratory tract. Am J Clin Pathol 1966; 46: pp. 411-419
- 25. Morgan H.R., and Finland M.: Isolation of herpes virus from a case of atypical pneumonia and erythema multiforme exudativum with studies of four additional cases. Am J Med Sci 1949; 217: pp. 92-95
- 26. Nash G.: Necrotizing tracheobronchitis and bronchopneumonia consistent with herpetic infection. Hum Pathol 1972; 3: pp. 283-291
- 27. Nash G., and Foley F.D.: Herpetic infection of the middle and lower respiratory tract. Am J Clin Pathol 1970; 54: pp. 857-863
- 28. Ramsey P.G., Fife K.H., Hackman R.C., et al: Herpes simplex virus pneumonia: clinical, virologic, and pathologic features in 20 patients. Ann Intern Med 1982; 97: pp. 813-820
- 29. Bruynseels P., Jorens P.G., Demey H.E., et al: Herpes simplex virus in the respiratory tract of critical care patients: a prospective study. Lancet 2003; 362: pp. 1536-1541
- 30. Camps K., Jorens P.G., Demey H.E., et al: Clinical significance of herpes simplex virus in the lower respiratory tract of critically ill patients. Eur J Clin Microbiol Infect Dis 2002; 21: pp. 758-759
- 31. Klainer A.S., Oud L., Randazzo J., et al: Herpes simplex virus involvement of the lower respiratory tract following surgery. Chest 1994; 106: pp. 8S-14S
- 32. Liebau P., Kuse E., Winkler M., et al: Management of herpes simplex virus type 1 pneumonia following liver transplantation. Infection 1996; 24: pp. 130-135
- 33. Tuxen D.V., Wilson J.W., and Cade J.F.: Prevention of lower respiratory herpes simplex virus infection with acyclovir in patients with the adult respiratory distress syndrome. Am Rev Respir Dis 1987; 136: pp. 402-405
- 34. Schuller D., Spessert C., Fraser V.J., et al: Herpes simplex virus from respiratory tract secretions: epidemiology, clinical characteristics, and outcome in immunocompromised and nonimmunocompromised hosts. Am J Med 1993; 94: pp. 29-33
- 35. Campsen J., Hendrickson R., Bak T., et al: Herpes simplex in a liver transplant recipient. Liver Transpl 2006; 12: pp. 1171-1173
- 36. Basse G., Mengelle C., Kamar N., et al: Disseminated herpes simplex type-2 (HSV-2) infection after solid-organ transplantation. Infection 2008; 36: pp. 62-64
- 37. Duckro A.N., Sha B.E., Jakate S., et al: Herpes simplex virus hepatitis: expanding the spectrum of disease. Transpl Infect Dis 2006; 8: pp. 171-176
- 38. Kaufman B., Gandhi S.A., Louie E., et al: Herpes simplex virus hepatitis: case report and review. Clin Infect Dis 1997; 24: pp. 334-338
- 39. Taylor R.J., Saul S.H., Dowling J.N., et al: Primary disseminated herpes simplex infection with fulminant hepatitis following renal transplantation. Arch Intern Med 1981; 141: pp. 1519-1521
- 40. Bissig K.D., Zimmermann A., Bernasch D., et al: Herpes simplex virus hepatitis 4 years after liver transplantation. J Gastroenterol 2003; 38: pp. 1005-1008
- 41. Adler M., Goldman M., Liesnard C., et al: Diffuse herpes simplex virus colitis in a kidney transplant recipient successfully treated with acyclovir. Transplantation 1987; 43: pp. 919-921
- 42. Delis S., Kato T., Ruiz P., et al: Herpes simplex colitis in a child with combined liver and small bowel transplant. Pediatr Transplant 2001; 5: pp. 374-377
- 43. el-Serag H.B., Zwas F.R., Cirillo N.W., et al: Fulminant herpes colitis in a patient with Crohn’s disease. J Clin Gastroenterol 1996; 22: pp. 220-223
- 44. Fishbein P.G., Tuthill R., Kressel H., et al: Herpes simplex esophagitis: a cause of upper-gastrointestinal bleeding. Dig Dis Sci 1979; 24: pp. 540-544
- 45. Howiler W., and Goldberg H.I.: Gastroesophageal involvement in herpes simplex. Gastroenterology 1976; 70: pp. 775-778
- 46. Mosimann F., Cuenoud P.F., Steinhauslin F., et al: Herpes simplex esophagitis after renal transplantation. Transpl Int 1994; 7: pp. 79-82
- 47. Naik H.R., and Chandrasekar P.H.: Herpes simplex virus (HSV) colitis in a bone marrow transplant recipient. Bone Marrow Transplant 1996; 17: pp. 285-286
- 48. Watts S.J., Alexander L.C., Fawcett K., et al: Herpes simplex esophagitis in a renal transplant patient treated with cyclosporine A: a case report. Am J Gastroenterol 1986; 81: pp. 185-188
- 49. Gomez E., Melon S., Aguado S., et al: Herpes simplex virus encephalitis in a renal transplant patient: diagnosis by polymerase chain reaction detection of HSV DNA. Am J Kidney Dis 1997; 30: pp. 423-427
- 50. Raschilas F., Wolff M., Delatour F., et al: Outcome of and prognostic factors for herpes simplex encephalitis in adult patients: results of a multicenter study. Clin Infect Dis 2002; 35: pp. 254-260
- 51. Lakeman F.D., and Whitley R.J.: Diagnosis of herpes simplex encephalitis: application of polymerase chain reaction to cerebrospinal fluid from brain-biopsied patients and correlation with disease. National Institute of Allergy and Infectious Diseases Collaborative Antiviral Study Group. J Infect Dis 1995; 171: pp. 857-863
- 52. Whitley R.J., Alford C.A., Hirsch M.S., et al: Vidarabine versus acyclovir therapy in herpes simplex encephalitis. N Engl J Med 1986; 314: pp. 144-149
- 53. Shepp D.H., Dandliker P.S., Flournoy N., et al: Once-daily intravenous acyclovir for prophylaxis of herpes simplex virus reactivation after marrow transplantation. J Antimicrob Chemother 1985; 16: pp. 389-395
- 54. Chen Y., Scieux C., Garrait V., et al: Resistant herpes simplex virus type 1 infection: an emerging concern after allogeneic stem cell transplantation. Clin Infect Dis 2000; 31: pp. 927-935
- 55. Erard V., Wald A., Corey L., et al: Use of long-term suppressive acyclovir after hematopoietic stem-cell transplantation: impact on herpes simplex virus (HSV) disease and drug-resistant HSV disease. J Infect Dis 2007; 196: pp. 266-270
- 56. Morfin F., and Thouvenot D.: Herpes simplex virus resistance to antiviral drugs. J Clin Virol 2003; 26: pp. 29-37
- 57. Nugier F., Colin J.N., Aymard M., et al: Occurrence and characterization of acyclovir-resistant herpes simplex virus isolates: report on a two-year sensitivity screening survey. J Med Virol 1992; 36: pp. 1-12
- 58. Herpes simplex virus (HSV)-1 and -2, and varicella zoster virus (VZV). Am J Transplant 2004; 4: pp. 69-71
- 59. Alcaide M.L., Abbo L., Pano J.R., et al: Herpes zoster infection after liver transplantation in patients receiving induction therapy with alemtuzumab. Clin Transplant 2008; 22: pp. 502-507
- 60. Arness T., Pedersen R., Dierkhising R., et al: Varicella zoster virus-associated disease in adult kidney transplant recipients: incidence and risk-factor analysis. Transpl Infect Dis 2008; 10: pp. 260-268
- 61. Manuel O., Kumar D., Singer L.G., et al: Incidence and clinical characteristics of herpes zoster after lung transplantation. J Heart Lung Transplant 2008; 27: pp. 11-16
- 62. Locksley R.M., Flournoy N., Sullivan K.M., et al: Infection with varicella-zoster virus after marrow transplantation. J Infect Dis 1985; 152: pp. 1172-1181
- 63. Boeckh M., Kim H.W., Flowers M.E., et al: Long-term acyclovir for prevention of varicella zoster virus disease after allogeneic hematopoietic cell transplantation–a randomized double-blind placebo-controlled study. Blood 2006; 107: pp. 1800-1805
- 64. Han C.S., Miller W., Haake R., et al: Varicella zoster infection after bone marrow transplantation: incidence, risk factors and complications. Bone Marrow Transplant 1994; 13: pp. 277-283
- 65. Leung T.F., Chik K.W., Li C.K., et al: Incidence, risk factors and outcome of varicella-zoster virus infection in children after haematopoietic stem cell transplantation. Bone Marrow Transplant 2000; 25: pp. 167-172
- 66. Koc Y., Miller K.B., Schenkein D.P., et al: Varicella zoster virus infections following allogeneic bone marrow transplantation: frequency, risk factors, and clinical outcome. Biol Blood Marrow Transplant 2000; 6: pp. 44-49
- 67. Gnann J.: Herpes simplex and varicella zoster virus infection after hemopoietic stem cell or solid organ transplantation. Philadelphia: Lippincott, Williams and Wilkins, 2003.
- 68. Fuks L., Shitrit D., Fox B.D., et al: Herpes zoster after lung transplantation: incidence, timing, and outcome. Ann Thorac Surg 2009; 87: pp. 423-426
- 69. Gourishankar S., McDermid J.C., Jhangri G.S., et al: Herpes zoster infection following solid organ transplantation: incidence, risk factors and outcomes in the current immunosuppressive era. Am J Transplant 2004; 4: pp. 108-115
- 70. Herrero J.I., Quiroga J., Sangro B., et al: Herpes zoster after liver transplantation: incidence, risk factors, and complications. Liver Transpl 2004; 10: pp. 1140-1143
- 71. Lauzurica R., Bayes B., Frias C., et al: Disseminated varicella infection in adult renal allograft recipients: role of mycophenolate mofetil. Transplant Proc 2003; 35: pp. 1758-1759
- 72. Weinberg A., Horslen S.P., Kaufman S.S., et al: Safety and immunogenicity of varicella-zoster virus vaccine in pediatric liver and intestine transplant recipients. Am J Transplant 2006; 6: pp. 565-568
- 73. Khan S., Erlichman J., and Rand E.B.: Live virus immunization after orthotopic liver transplantation. Pediatr Transplant 2006; 10: pp. 78-82
- 74. Kraft J.N., and Shaw J.C.: Varicella infection caused by Oka strain vaccine in a heart transplant recipient. Arch Dermatol 2006; 142: pp. 943-945
- 75. Levitsky J., Te H.S., Faust T.W., et al: Varicella infection following varicella vaccination in a liver transplant recipient. Am J Transplant 2002; 2: pp. 880-882
- 76. Sauerbrei A., Prager J., Hengst U., et al: Varicella vaccination in children after bone marrow transplantation. Bone Marrow Transplant 1997; 20: pp. 381-383
- 77. Merck : Varivax varicella virus vaccine live. http://www.merck.com/product/usa/pi_circulars/v/varivax/varivax_pi.pdf
- 78. Hata A., Asanuma H., Rinki M., et al: Use of an inactivated varicella vaccine in recipients of hematopoietic-cell transplants. N Engl J Med 2002; 347: pp. 26-34
- 79. Feldhoff C.M., Balfour H.H., Simmons R.L., et al: Varicella in children with renal transplants. J Pediatr 1981; 98: pp. 25-31
- 80. McGregor R.S., Zitelli B.J., Urbach A.H., et al: Varicella in pediatric orthotopic liver transplant recipients. Pediatrics 1989; 83: pp. 256-261
- 81. Parnham A.P., Flexman J.P., Saker B.M., et al: Primary varicella in adult renal transplant recipients: a report of three cases plus a review of the literature. Clin Transplant 1995; 9: pp. 115-118
- 82. Fall A.J., Aitchison J.D., Krause A., et al: Donor organ transmission of varicella zoster due to cardiac transplantation. Transplantation 2000; 70: pp. 211-213
- 83. Hyland J.M., and Butterworth J.: Severe acute visceral pain from varicella zoster virus. Anesth Analg 2003; 97: pp. 1117-1118
- 84. Koskiniemi M., Piiparinen H., Rantalaiho T., et al: Acute central nervous system complications in varicella zoster virus infections. J Clin Virol 2002; 25: pp. 293-301
- 85. Aberle S.W., and Puchhammer-Stockl E.: Diagnosis of herpesvirus infections of the central nervous system. J Clin Virol 2002; 25: pp. S79-S85
- 86. Puchhammer-Stockl E., Popow-Kraupp T., Heinz F.X., et al: Detection of varicella-zoster virus DNA by polymerase chain reaction in the cerebrospinal fluid of patients suffering from neurological complications associated with chicken pox or herpes zoster. J Clin Microbiol 1991; 29: pp. 1513-1516
- 87. Glaser C.A., Honarmand S., Anderson L.J., et al: Beyond viruses: clinical profiles and etiologies associated with encephalitis. Clin Infect Dis 2006; 43: pp. 1565-1577
- 88. Gilden D.: Varicella zoster virus and central nervous system syndromes. Herpes 2004; 11: pp. 89A-94A
- 89. Tyring S., Belanger R., Bezwoda W., et al: A randomized, double-blind trial of famciclovir versus acyclovir for the treatment of localized dermatomal herpes zoster in immunocompromised patients. Cancer Invest 2001; 19: pp. 13-22
- 90. American Academy of Pediatrics : Varicella zoster virus. Elk Grove (IL): American Academy of Pediatrics, 2000.
- 91. Marin M., Guris D., Chaves S.S., et al: Prevention of varicella: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2007; 56: pp. 1-40
- 92. A new product (VariZIG™) for postexposure prophylaxis of varicella available under an investigational new drug application expanded access protocol. MMWR Morb Mortal Wkly Rep 2006; 55: pp. 209-210
- 93. Epstein-Barr virus and lymphoproliferative disorders after transplantation. Am J Transplant 2004; 4: pp. 59-65
- 94. Nalesnik M.A.: The diverse pathology of post-transplant lymphoproliferative disorders: the importance of a standardized approach. Transpl Infect Dis 2001; 3: pp. 88-96
- 95. Preiksaitis J.K.: New developments in the diagnosis and management of posttransplantation lymphoproliferative disorders in solid organ transplant recipients. Clin Infect Dis 2004; 39: pp. 1016-1023
- 96. Karras A., Thervet E., and Legendre C.: Hemophagocytic syndrome in renal transplant recipients: report of 17 cases and review of literature. Transplantation 2004; 77: pp. 238-243
- 97. Lee E.S., Locker J., Nalesnik M., et al: The association of Epstein-Barr virus with smooth-muscle tumors occurring after organ transplantation. N Engl J Med 1995; 332: pp. 19-25
- 98. Jenkins F.J., Rowe D.T., and Rinaldo C.R.: Herpesvirus infections in organ transplant recipients. Clin Diagn Lab Immunol 2003; 10: pp. 1-7
- 99. Johannsen E., Schooley R., and Kaye K.: Epstein-Barr virus (infectious mononucleosis). In Mandell G., Bennett J., and Dolin R. (eds): . Philadelphia (PA): Elsevier, 2005. pp. 1801-1820
- 100. Baskin H.J., and Hedlund G.: Neuroimaging of herpesvirus infections in children. Pediatr Radiol 2007; 37: pp. 949-963
- 101. Alfieri C., Tanner J., Carpentier L., et al: Epstein-Barr virus transmission from a blood donor to an organ transplant recipient with recovery of the same virus strain from the recipient’s blood and oropharynx. Blood 1996; 87: pp. 812-817
- 102. Haque T., Thomas J.A., Falk K.I., et al: Transmission of donor Epstein-Barr virus (EBV) in transplanted organs causes lymphoproliferative disease in EBV-seronegative recipients. J Gen Virol 1996; 77: pp. 1169-1172
- 103. Frizzera G., Hanto D.W., Gajl-Peczalska K.J., et al: Polymorphic diffuse B-cell hyperplasias and lymphomas in renal transplant recipients. Cancer Res 1981; 41: pp. 4262-4279
- 104. Hanto D.W., Gajl-Peczalska K.J., Frizzera G., et al: Epstein-Barr virus (EBV) induced polyclonal and monoclonal B-cell lymphoproliferative diseases occurring after renal transplantation. Clinical, pathologic, and virologic findings and implications for therapy. Ann Surg 1983; 198: pp. 356-369
- 105. Yousem S.A., Randhawa P., Locker J., et al: Posttransplant lymphoproliferative disorders in heart-lung transplant recipients: primary presentation in the allograft. Hum Pathol 1989; 20: pp. 361-369
- 106. Diaz-Guzman E., Farver C., Kanne J.P., et al: A 65-year-old man with odynophagia and a lung mass. Chest 2009; 135: pp. 876-879
- 107. Khan M.S., Ahmed S., Challacombe B., et al: Post-transplant lymphoproliferative disorder (PTLD) presenting as painful lymphocele 12 years after a cadaveric renal transplant. Int Urol Nephrol 2008; 40: pp. 547-550
- 108. Lee W.K., Lau E.W., Duddalwar V.A., et al: Abdominal manifestations of extranodal lymphoma: spectrum of imaging findings. AJR Am J Roentgenol 2008; 191: pp. 198-206
- 109. Kunitomi A., Arima N., and Ishikawa T.: Epstein-Barr virus-associated post-transplant lymphoproliferative disorders presented as interstitial pneumonia; successful recovery with rituximab. Haematologica 2007; 92: pp. e49-e52
- 110. Ellis D., Jaffe R., Green M., et al: Epstein-Barr virus-related disorders in children undergoing renal transplantation with tacrolimus-based immunosuppression. Transplantation 1999; 68: pp. 997-1003
- 111. Ho M., Miller G., Atchison R.W., et al: Epstein-Barr virus infections and DNA hybridization studies in posttransplantation lymphoma and lymphoproliferative lesions: the role of primary infection. J Infect Dis 1985; 152: pp. 876-886
- 112. Swinnen L.J., Costanzo-Nordin M.R., Fisher S.G., et al: Increased incidence of lymphoproliferative disorder after immunosuppression with the monoclonal antibody OKT3 in cardiac-transplant recipients. N Engl J Med 1990; 323: pp. 1723-1728
- 113. Walker R.C., Marshall W.F., Strickler J.G., et al: Pretransplantation assessment of the risk of lymphoproliferative disorder. Clin Infect Dis 1995; 20: pp. 1346-1353
- 114. Keay S., Oldach D., Wiland A., et al: Posttransplantation lymphoproliferative disorder associated with OKT3 and decreased antiviral prophylaxis in pancreas transplant recipients. Clin Infect Dis 1998; 26: pp. 596-600
- 115. Cox K.L., Lawrence-Miyasaki L.S., Garcia-Kennedy R., et al: An increased incidence of Epstein-Barr virus infection and lymphoproliferative disorder in young children on FK506 after liver transplantation. Transplantation 1995; 59: pp. 524-529
- 116. Manez R., Breinig M.C., Linden P., et al: Posttransplant lymphoproliferative disease in primary Epstein-Barr virus infection after liver transplantation: the role of cytomegalovirus disease. J Infect Dis 1997; 176: pp. 1462-1467
- 117. Weinstock D.M., Ambrossi G.G., Brennan C., et al: Preemptive diagnosis and treatment of Epstein-Barr virus-associated post transplant lymphoproliferative disorder after hematopoietic stem cell transplant: an approach in development. Bone Marrow Transplant 2006; 37: pp. 539-546
- 118. Preiksaitis J.K., and Keay S.: Diagnosis and management of posttransplant lymphoproliferative disorder in solid-organ transplant recipients. Clin Infect Dis 2001; 33: pp. S38-S46
- 119. Tsai D.E., Douglas L., Andreadis C., et al: EBV PCR in the diagnosis and monitoring of posttransplant lymphoproliferative disorder: results of a two-arm prospective trial. Am J Transplant 2008; 8: pp. 1016-1024
- 120. Wheless S.A., Gulley M.L., Raab-Traub N., et al: Post-transplantation lymphoproliferative disease: Epstein-Barr virus DNA levels, HLA-A3, and survival. Am J Respir Crit Care Med 2008; 178: pp. 1060-1065
- 121. Harris N.L.: Posttransplant lymphoproliferative disorders (PTLD). In Jaffe E., Harris N., and Stein H. (eds): Pathology and genetics: tumours of haematopoietic and lymphoid tissues. WHO classification of tumours. Lyon (France): IARC Press, 2001.
- 122. Harris N.L., Ferry J.A., and Swerdlow S.H.: Posttransplant lymphoproliferative disorders: summary of Society for Hematopathology Workshop. Semin Diagn Pathol 1997; 14: pp. 8-14
- 123. Starzl T.E., Nalesnik M.A., Porter K.A., et al: Reversibility of lymphomas and lymphoproliferative lesions developing under cyclosporin-steroid therapy. Lancet 1984; 1: pp. 583-587
- 124. Tsai D.E., Hardy C.L., Tomaszewski J.E., et al: Reduction in immunosuppression as initial therapy for posttransplant lymphoproliferative disorder: analysis of prognostic variables and long-term follow-up of 42 adult patients. Transplantation 2001; 71: pp. 1076-1088
- 125. Hanto D.W., Frizzera G., Gajl-Peczalska K.J., et al: Epstein-Barr virus-induced B-cell lymphoma after renal transplantation: acyclovir therapy and transition from polyclonal to monoclonal B-cell proliferation. N Engl J Med 1982; 306: pp. 913-918
- 126. Andersson J., Skoldenberg B., Ernberg I., et al: Acyclovir treatment in primary Epstein-Barr virus infection. A double-blind placebo-controlled study. Scand J Infect Dis Suppl 1985; 47: pp. 107-115
- 127. Paya C.V., Fung J.J., Nalesnik M.A., et al: Epstein-Barr virus-induced posttransplant lymphoproliferative disorders. ASTS/ASTP EBV-PTLD Task Force and The Mayo Clinic Organized International Consensus Development Meeting. Transplantation 1999; 68: pp. 1517-1525
- 128. Yao Q.Y., Ogan P., Rowe M., et al: Epstein-Barr virus-infected B cells persist in the circulation of acyclovir-treated virus carriers. Int J Cancer 1989; 43: pp. 67-71
- 129. Choquet S., Leblond V., Herbrecht R., et al: Efficacy and safety of rituximab in B-cell post-transplantation lymphoproliferative disorders: results of a prospective multicenter phase 2 study. Blood 2006; 107: pp. 3053-3057
- 130. Norin S., Kimby E., Ericzon B.G., et al: Posttransplant lymphoma–a single-center experience of 500 liver transplantations. Med Oncol 2004; 21: pp. 273-284
- 131. Trappe R.U., Choquet S., Reinke P., et al: Salvage therapy for relapsed posttransplant lymphoproliferative disorders (PTLD) with a second progression of PTLD after upfront chemotherapy: the role of single-agent rituximab. Transplantation 2007; 84: pp. 1708-1712
- 132. Oertel S.H., Verschuuren E., Reinke P., et al: Effect of anti-CD 20 antibody rituximab in patients with post-transplant lymphoproliferative disorder (PTLD). Am J Transplant 2005; 5: pp. 2901-2906
- 133. Rooney C.M., Smith C.A., Ng C.Y.C., et al: Infusion of cytotoxic T cells for the prevention and treatment of Epstein-Barr virus-induced lymphoma in allogeneic transplant recipients. Blood 1998; 92: pp. 1549-1555
- 134. Gustafsson A., Levitsky V., Zou J.-Z., et al: Epstein-Barr virus (EBV) load in bone marrow transplant recipients at risk to develop posttransplant lymphoproliferative disease: prophylactic infusion of EBV-specific cytotoxic T cells. Blood 2000; 95: pp. 807-814
- 135. Savoldo B., Goss J.A., Hammer M.M., et al: Treatment of solid organ transplant recipients with autologous Epstein Barr virus-specific cytotoxic T lymphocytes (CTLs). Blood 2006; 108: pp. 2942-2949
- 136. Haque T., Taylor C., Wilkie G.M., et al: Complete regression of posttransplant lymphoproliferative disease using partially HLA-matched Epstein Barr virus-specific cytotoxic T cells. Transplantation 2001; 72: pp. 1399-1402
- 137. Haque T., Wilkie G.M., Jones M.M., et al: Allogeneic cytotoxic T-cell therapy for EBV-positive posttransplantation lymphoproliferative disease: results of a phase 2 multicenter clinical trial. Blood 2007; 110: pp. 1123-1131
- 138. Haque T., Wilkie G.M., Taylor C., et al: Treatment of Epstein-Barr-virus-positive post-transplantation lymphoproliferative disease with partly HLA-matched allogeneic cytotoxic T cells. Lancet 2002; 360: pp. 436-442
- 139. Comoli P., Labirio M., Basso S., et al: Infusion of autologous Epstein-Barr virus (EBV)-specific cytotoxic T cells for prevention of EBV-related lymphoproliferative disorder in solid organ transplant recipients with evidence of active virus replication. Blood 2002; 99: pp. 2592-2598
- 140. Khanna R., Bell S., Sherritt M., et al: Activation and adoptive transfer of Epstein–Barr virus-specific cytotoxic T cells in solid organ transplant patients with posttransplant lymphoproliferative disease. Proc Natl Acad Sci U S A 1999; 96: pp. 10391-10396
- 141. Choquet S., Trappe R., Leblond V., et al: CHOP-21 for the treatment of post-transplant lymphoproliferative disorders (PTLD) following solid organ transplantation. Haematologica 2007; 92: pp. 273-274
- 142. Elstrom R.L., Andreadis C., Aqui N.A., et al: Treatment of PTLD with rituximab or chemotherapy. Am J Transplant 2006; 6: pp. 569-576
- 143. Garrett T.J., Chadburn A., Barr M.L., et al: Posttransplantation lymphoproliferative disorders treated with cyclophosphamide-doxorubicin-vincristine-prednisone chemotherapy. Cancer 1993; 72: pp. 2782-2785
- 144. Mamzer-Bruneel M.F., Lome C., Morelon E., et al: Durable remission after aggressive chemotherapy for very late post-kidney transplant lymphoproliferation: a report of 16 cases observed in a single center. J Clin Oncol 2000; 18: pp. 3622-3632
- 145. Everly M.J., Bloom R.D., Tsai D.E., et al: Posttransplant lymphoproliferative disorder. Ann Pharmacother 2007; 41: pp. 1850-1858
- 146. Karras A., Thervet E., Le Meur Y., et al: Successful renal retransplantation after post-transplant lymphoproliferative disease. Am J Transplant 2004; 4: pp. 1904-1909
- 147. Darenkov I.A., Marcarelli M.A., Basadonna G.P., et al: Reduced incidence of Epstein-Barr virus-associated posttransplant lymphoproliferative disorder using preemptive antiviral therapy. Transplantation 1997; 64: pp. 848-852
- 148. Davis C.L., Harrison K.L., McVicar J.P., et al: Antiviral prophylaxis and the Epstein Barr virus-related post-transplant lymphoproliferative disorder. Clin Transplant 1995; 9: pp. 53-59
- 149. Funch D.P., Walker A.M., Schneider G., et al: Ganciclovir and acyclovir reduce the risk of post-transplant lymphoproliferative disorder in renal transplant recipients. Am J Transplant 2005; 5: pp. 2894-2900
- 150. Green M., Kaufmann M., Wilson J., et al: Comparison of intravenous ganciclovir followed by oral acyclovir with intravenous ganciclovir alone for prevention of cytomegalovirus and Epstein-Barr virus disease after liver transplantation in children. Clin Infect Dis 1997; 25: pp. 1344-1349
- 151. Bakker N.A., Verschuuren E.A., Erasmus M.E., et al: Epstein-Barr virus-DNA load monitoring late after lung transplantation: a surrogate marker of the degree of immunosuppression and a safe guide to reduce immunosuppression. Transplantation 2007; 83: pp. 433-438
- 152. Salahuddin S.Z., Ablashi D.V., Markham P.D., et al: Isolation of a new virus, HBLV, in patients with lymphoproliferative disorders. Science 1986; 234: pp. 596-601
- 153. Gentile G.: Post-transplant HHV-6 diseases. Herpes 2000; 7: pp. 24-27
- 154. Leach C.T., Sumaya C.V., and Brown N.A.: Human herpesvirus-6: clinical implications of a recently discovered, ubiquitous agent. J Pediatr 1992; 121: pp. 173-181
- 155. Brown N.A., Sumaya C.V., Liu C.R., et al: Fall in human herpesvirus 6 seropositivity with age. Lancet 1988; 2: pp. 396
- 156. Lau Y.L., Peiris M., Chan G.C., et al: Primary human herpes virus 6 infection transmitted from donor to recipient through bone marrow infusion. Bone Marrow Transplant 1998; 21: pp. 1063-1066
- 157. Cervera C., Marcos M.A., Linares L., et al: A prospective survey of human herpesvirus-6 primary infection in solid organ transplant recipients. Transplantation 2006; 82: pp. 979-982
- 158. Zerr D.M., Corey L., Kim H.W., et al: Clinical outcomes of human herpesvirus 6 reactivation after hematopoietic stem cell transplantation. Clin Infect Dis 2005; 40: pp. 932-940
- 159. de Pagter P.J., Schuurman R., Meijer E., et al: Human herpesvirus type 6 reactivation after haematopoietic stem cell transplantation. J Clin Virol 2008; 43: pp. 361-366
- 160. de Pagter P.J., Schuurman R., Visscher H., et al: Human herpes virus 6 plasma DNA positivity after hematopoietic stem cell transplantation in children: an important risk factor for clinical outcome. Biol Blood Marrow Transplant 2008; 14: pp. 831-839
- 161. Wang L.R., Dong L.J., Zhang M.J., et al: The impact of human herpesvirus 6B reactivation on early complications following allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 2006; 12: pp. 1031-1037
- 162. Yamane A., Mori T., Suzuki S., et al: Risk factors for developing human herpesvirus 6 (HHV-6) reactivation after allogeneic hematopoietic stem cell transplantation and its association with central nervous system disorders. Biol Blood Marrow Transplant 2007; 13: pp. 100-106
- 163. DesJardin J.A., Gibbons L., Cho E., et al: Human herpesvirus 6 reactivation is associated with cytomegalovirus infection and syndromes in kidney transplant recipients at risk for primary cytomegalovirus infection. J Infect Dis 1998; 178: pp. 1783-1786
- 164. Dockrell D.H., Prada J., Jones M.F., et al: Seroconversion to human herpesvirus 6 following liver transplantation is a marker of cytomegalovirus disease. J Infect Dis 1997; 176: pp. 1135-1140
- 165. Lehto J.T., Halme M., Tukiainen P., et al: Human herpesvirus-6 and -7 after lung and heart-lung transplantation. J Heart Lung Transplant 2007; 26: pp. 41-47
- 166. Ratnamohan V.M., Chapman J., Howse H., et al: Cytomegalovirus and human herpesvirus 6 both cause viral disease after renal transplantation. Transplantation 1998; 66: pp. 877-882
- 167. Yoshikawa T., Suga S., Asano Y., et al: A prospective study of human herpesvirus-6 infection in renal transplantation. Transplantation 1992; 54: pp. 879-883
- 168. Humar A., Malkan G., Moussa G., et al: Human herpesvirus-6 is associated with cytomegalovirus reactivation in liver transplant recipients. J Infect Dis 2000; 181: pp. 1450-1453
- 169. Herbein G., Strasswimmer J., Altieri M., et al: Longitudinal study of human herpesvirus 6 infection in organ transplant recipients. Clin Infect Dis 1996; 22: pp. 171-173
- 170. Razonable R.R., and Paya C.V.: The impact of human herpesvirus-6 and -7 infection on the outcome of liver transplantation. Liver Transpl 2002; 8: pp. 651-658
- 171. Humar A., Asberg A., Kumar D., et al: An assessment of herpesvirus co-infections in patients with CMV disease: correlation with clinical and virologic outcomes. Am J Transplant 2009; 9: pp. 374-381
- 172. Singh N., and Paterson D.L.: Encephalitis caused by human herpesvirus-6 in transplant recipients: relevance of a novel neurotropic virus. Transplantation 2000; 69: pp. 2474-2479
- 173. Bollen A.E., Wartan A.N., Krikke A.P., et al: Amnestic syndrome after lung transplantation by human herpes virus-6 encephalitis. J Neurol 2001; 248: pp. 619-620
- 174. Mookerjee B.P., and Vogelsang G.: Human herpes virus-6 encephalitis after bone marrow transplantation: successful treatment with ganciclovir. Bone Marrow Transplant 1997; 20: pp. 905-906
- 175. Mori T., Mihara A., Yamazaki R., et al: Myelitis associated with human herpes virus 6 (HHV-6) after allogeneic cord blood transplantation. Scand J Infect Dis 2007; 39: pp. 276-278
- 176. Seeley W.W., Marty F.M., Holmes T.M., et al: Post-transplant acute limbic encephalitis: clinical features and relationship to HHV6. Neurology 2007; 69: pp. 156-165
- 177. Vu T., Carrum G., Hutton G., et al: Human herpesvirus-6 encephalitis following allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant 2007; 39: pp. 705-709
- 178. Fotheringham J., Akhyani N., Vortmeyer A., et al: Detection of active human herpesvirus-6 infection in the brain: correlation with polymerase chain reaction detection in cerebrospinal fluid. J Infect Dis 2007; 195: pp. 450-454
- 179. Luppi M., Barozzi P., Maiorana A., et al: Human herpesvirus 6 infection in normal human brain tissue. J Infect Dis 1994; 169: pp. 943-944
- 180. Caserta M.T., McDermott M., Dewhurst S., et al: Human herpesvirus 6 (HHV6) DNA persistence and reactivation in healthy children. J Pediatr 2004; 145: pp. 478-484
- 181. Singh N., Carrigan D.R., Gayowski T., et al: Variant B human herpesvirus-6 associated febrile dermatosis with thrombocytopenia and encephalopathy in a liver transplant recipient. Transplantation 1995; 60: pp. 1355-1357
- 182. Revest M., Camus C., D’Halluin P.N., et al: Fatal human herpes virus 6 primary infection after liver transplantation. Transplantation 2007; 83: pp. 1404-1405
- 183. Randhawa P.S., Jenkins F.J., Nalesnik M.A., et al: Herpesvirus 6 variant A infection after heart transplantation with giant cell transformation in bile ductular and gastroduodenal epithelium. Am J Surg Pathol 1997; 21: pp. 847-853
- 184. Burns W.H., and Sandford G.R.: Susceptibility of human herpesvirus 6 to antivirals in vitro. J Infect Dis 1990; 162: pp. 634-637
- 185. Agut H., Aubin J.T., and Huraux J.M.: Homogeneous susceptibility of distinct human herpesvirus 6 strains to antivirals in vitro. J Infect Dis 1991; 163: pp. 1382-1383
- 186. Reymen D., Naesens L., Balzarini J., et al: Antiviral activity of selected acyclic nucleoside analogues against human herpesvirus 6. Antiviral Res 1995; 28: pp. 343-357
- 187. Ward K.N.: Human herpesviruses-6 and -7 infections. Curr Opin Infect Dis 2005; 18: pp. 247-252
- 188. Ward K.N., White R.P., Mackinnon S., et al: Human herpesvirus-7 infection of the CNS with acute myelitis in an adult bone marrow recipient. Bone Marrow Transplant 2002; 30: pp. 983-985
- 189. Yoshikawa T., Yoshida J., Hamaguchi M., et al: Human herpesvirus 7-associated meningitis and optic neuritis in a patient after allogeneic stem cell transplantation. J Med Virol 2003; 70: pp. 440-443
- 190. Kidd I.M., Clark D.A., Sabin C.A., et al: Prospective study of human betaherpesviruses after renal transplantation: association of human herpesvirus 7 and cytomegalovirus co-infection with cytomegalovirus disease and increased rejection. Transplantation 2000; 69: pp. 2400-2404
- 191. Osman H.K., Peiris J.S., Taylor C.E., et al: “Cytomegalovirus disease” in renal allograft recipients: is human herpesvirus 7 a co-factor for disease progression? J Med Virol 1996; 48: pp. 295-301
- 192. Tong C.Y., Bakran A., Williams H., et al: Association of human herpesvirus 7 with cytomegalovirus disease in renal transplant recipients. Transplantation 2000; 70: pp. 213-216
- 193. Moore P.S., and Chang Y.: Detection of herpesvirus-like DNA sequences in Kaposi’s sarcoma in patients with and without HIV infection. N Engl J Med 1995; 332: pp. 1181-1185
- 194. Cesarman E., Chang Y., Moore P.S., et al: Kaposi’s sarcoma-associated herpesvirus-like DNA sequences in AIDS-related body-cavity-based lymphomas. N Engl J Med 1995; 332: pp. 1186-1191
- 195. Antman K., and Chang Y.: Kaposi’s sarcoma. N Engl J Med 2000; 342: pp. 1027-1038
- 196. Moore P.S.: The emergence of Kaposi’s sarcoma-associated herpesvirus (human herpesvirus 8). N Engl J Med 2000; 343: pp. 1411-1413
- 197. Melbye M., Cook P.M., Hjalgrim H., et al: Risk factors for Kaposi’s-sarcoma-associated herpesvirus (KSHV/HHV-8) seropositivity in a cohort of homosexual men, 1981–1996. Int J Cancer 1998; 77: pp. 543-548
- 198. Ahmadpoor P., Ilkhanizadeh B., Sharifzadeh P., et al: Seroprevalence of human herpes virus-8 in renal transplant recipients: a single center study from Iran. Transplant Proc 2007; 39: pp. 1000-1002
- 199. Butler L.M., Dorsey G., Hladik W., et al: Kaposi sarcoma-associated herpesvirus (KSHV) seroprevalence in population-based samples of African children: evidence for at least 2 patterns of KSHV transmission. J Infect Dis 2009; 200: pp. 430-438
- 200. Fu B., Sun F., Li B., et al: Seroprevalence of Kaposi’s sarcoma-associated herpesvirus and risk factors in Xinjiang, China. J Med Virol 2009; 81: pp. 1422-1431
- 201. Engels E.A., Atkinson J.O., Graubard B.I., et al: Risk factors for human herpesvirus 8 infection among adults in the United States and evidence for sexual transmission. J Infect Dis 2007; 196: pp. 199-207
- 202. Human herpesvirus-8 (HHV-8, KSHV). Am J Transplant 2004; 4: pp. 67-69
- 203. Dudderidge T.J., Khalifa M., Jeffery R., et al: Donor-derived human herpes virus 8-related Kaposi’s sarcoma in renal allograft ureter. Transpl Infect Dis 2008; 10: pp. 221-226
- 204. Luppi M., Barozzi P., Schulz T.F., et al: Bone marrow failure associated with human herpesvirus 8 infection after transplantation. N Engl J Med 2000; 343: pp. 1378-1385
- 205. Parravicini C., Olsen S.J., Capra M., et al: Risk of Kaposi’s sarcoma-associated herpes virus transmission from donor allografts among Italian posttransplant Kaposi’s sarcoma patients. Blood 1997; 90: pp. 2826-2829
- 206. Bergallo M., Costa C., Margio S., et al: Human herpes virus 8 infection in kidney transplant patients from an area of northwestern Italy (Piemonte region). Nephrol Dial Transplant 2007; 22: pp. 1757-1761
- 207. Boeckle E., Boesmueller C., Wiesmayr S., et al: Kaposi sarcoma in solid organ transplant recipients: a single center report. Transplant Proc 2005; 37: pp. 1905-1909
- 208. Verucchi G., Calza L., Trevisani F., et al: Human herpesvirus-8-related Kaposi’s sarcoma after liver transplantation successfully treated with cidofovir and liposomal daunorubicin. Transpl Infect Dis 2005; 7: pp. 34-37
- 209. Stallone G., Schena A., Infante B., et al: Sirolimus for Kaposi’s sarcoma in renal-transplant recipients. N Engl J Med 2005; 352: pp. 1317-1323
- 210. Lebbe C., Euvrard S., Barrou B., et al: Sirolimus conversion for patients with posttransplant Kaposi’s sarcoma. Am J Transplant 2006; 6: pp. 2164-2168
- 211. Robles R., Lugo D., Gee L., et al: Effect of antiviral drugs used to treat cytomegalovirus end-organ disease on subsequent course of previously diagnosed Kaposi’s sarcoma in patients with AIDS. J Acquir Immune Defic Syndr Hum Retrovirol 1999; 20: pp. 34-38
- 212. Little R.F., Merced-Galindez F., Staskus K., et al: A pilot study of cidofovir in patients with Kaposi sarcoma. J Infect Dis 2003; 187: pp. 149-153
- 213. Jones D., Ballestas M.E., Kaye K.M., et al: Primary-effusion lymphoma and Kaposi’s sarcoma in a cardiac-transplant recipient. N Engl J Med 1998; 339: pp. 444-449
- 214. Al Otaibi T., Al Sagheir A., Ludwin D., et al: Post renal transplant Castleman’s disease resolved after graft nephrectomy: a case report. Transplant Proc 2007; 39: pp. 1276-1277
- 215. Cagirgan S., Cirit M., Ok E., et al: Castleman’s disease in a renal allograft recipient. Nephron 1997; 76: pp. 352-353
- 216. Dotti G., Fiocchi R., Motta T., et al: Primary effusion lymphoma after heart transplantation: a new entity associated with human herpesvirus-8. Leukemia 1999; 13: pp. 664-670
- 217. Melo N.C., Sales M.M., Santana A.N., et al: Pleural primary effusion lymphoma in a renal transplant recipient. Am J Transplant 2008; 8: pp. 906-907
- 218. Stebbing J., Pantanowitz L., Dayyani F., et al: HIV-associated multicentric Castleman’s disease. Am J Hematol 2008; 83: pp. 498-503
- 219. Soulier J., Grollet L., Oksenhendler E., et al: Kaposi’s sarcoma-associated herpesvirus-like DNA sequences in multicentric Castleman’s disease. Blood 1995; 86: pp. 1276-1280
- 220. Mandel C., Silberstein M., and Hennessy O.: Case report: fatal pulmonary Kaposi’s sarcoma and Castleman’s disease in a renal transplant recipient. Br J Radiol 1993; 66: pp. 264-265
- 221. Theate I., Michaux L., Squifflet J.P., et al: Human herpesvirus 8 and Epstein-Barr virus-related monotypic large B-cell lymphoproliferative disorder coexisting with mixed variant of Castleman’s disease in a lymph node of a renal transplant recipient. Clin Transplant 2003; 17: pp. 451-454
- 222. Casper C.: Defining a role for antiviral drugs in the treatment of persons with HHV-8 infection. Herpes 2006; 13: pp. 42-47
- 223. Gaidano G., and Carbone A.: Primary effusion lymphoma: a liquid phase lymphoma of fluid-filled body cavities. Adv Cancer Res 2001; 80: pp. 115-146
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree