Severe combined immunodeficiency (SCID) is fatal in infancy unless corrected with allogeneic bone marrow transplants (BMT), preferably from a family-related genotypically HLA-identical donor (RID) or phenotypically HLA-matched family donor (PMD). For the majority of SCID patients, such donors are not available; Therefore, parents who are HLA-haploidentical donors (HID) or HLA-matched unrelated donors (MUD) have been used. MUD BMT are associated with increased frequency of acute graft versus host disease, which can be controlled by high doses of steroids. HID BMT are associated with increased frequency of short- and long-term graft failure, need for repeated transplants, fatal pneumonitis, impaired immune reconstitution, and long-term complications, contributing to lower survival. In conclusion, the excellent long-term survival, immune reconstitution, and normal quality of life after MUD BMT suggests that in the absence of RID or PMD, MUD BMT should be offered for patients suffering from SCID.
Severe combined immunodeficiency (SCID) is a heterogeneous group of inherited diseases characterized by significantly impaired T-cell immunity that leads to death in infancy. The diagnosis of SCID relies on distinct clinical manifestations and laboratory features, and ideally is confirmed by the identification of mutations in genes known to be critical for T lineage development and function. Complete cure can be attained in the majority of patients suffering from SCID by using allogeneic bone marrow transplantation (BMT). The best outcome is achieved by family-related genotypically HLA-identical donors (RID). Among populations with high consanguinity marriage, RID account for the majority of transplants for SCID ; however, in most European and North American populations, RID are found for only 15% to 25% of the patients. BMT using phenotypically HLA-matched family-related donors (PMD) have resulted in a relatively high success rate ; however, PMD are not frequently found. The lack of RID or PMD for more than 75% of SCID patients led many groups to search for alternative sources, such as parents who are often HLA-haploidentical donors (HID) or HLA-matched unrelated donors (MUD).
The first attempt to treat SCID with unmodified MUD transplant was performed in 1973. A patient diagnosed with SCID, whose similarly affected sister died previously after receiving a transplant from her HLA-haploidentical parent, underwent BMT from a partially MUD found among 800 normal individuals registered in Denmark. The patient achieved durable engraftment with complete hematopoietic and immunologic reconstitution, but suffered from skin and oral mucosa chronic graft versus host disease (GvHD).
Difficulties finding HLA-matched unrelated donors and the lack of adequate means to control GvHD, together with the increased availability of T-cell depleted HID BMT in the early 1980s resulted in limited use of MUD BMT for SCID. However, it soon became apparent that with some exceptions, the success rate of HID BMT consistently hovered around 50% at best, regardless of the T-cell depletion method (D. Kohn, Los Angeles, California, personal communication, 2006; L. Notarangelo, Brescia, Italy, personal communication, 2006).
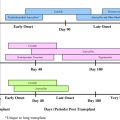
During the late 1980s, several events including the disappointment from HID BMT for SCID, the surge in the number of bone marrow donor registries ( Fig. 1 ), and the development of efficient medications to control GvHD, such as cyclosporine A (CsA), prompted Dr Roifman to systematically explore the systematic use of MUD BMT for SCID in their center. Therefore, in 1987, Dr Roifman created a protocol for MUD BMT in SCID. The protocol included strict patient isolation in private HEPA-filtered rooms from diagnosis until discharge, intensive pretransplant antimicrobial management with intravenous immunoglobulins (to maintain IgG≥6 g/L), Pneumocystis jiroveci pneumonia prophylaxis, close Herpes virus group surveillance, and nutritional support. Pretransplant conditioning consisted of oral or intravenous busulfan in 16 doses over 4 days (total amount ranging from 16 to 20 mg/kg), in accordance with busulfan blood levels, followed by a 4-day course of cyclophosphamide. Patients received 3 to 5 × 10 8 nucleated cells per kilogram body weight from bone marrow that was unmodified except for volume reduction and plasma removal in blood group mismatch. The amount of nucleated bone marrow harvested from the adult donors was often greater than that required for the infant SCID, therefore excess bone marrow was frozen as backup for graft failure. Patients also received aggressive GvHD prophylaxis and treatment, detailed later in this article, as well as granulocyte-macrophage colony stimulating factor or granulocyte colony stimulating factor from the day of transplant (or day +5 in some cases). This protocol led to improved engraftment and patient survival, which was summarized in 2000 by Dalal and colleagues. Among the first 15 patients with SCID and CID in the authors’ center who underwent BMT from HLA-matched or 1 non-DR antigen mismatched unrelated donors, survival was 73.3% with a mean follow-up of 47.4 months (range 18–101 months). All patients had leukocytes engraftment, which were demonstrated to be 100% donor by restriction length fragment polymorphism. Deaths were directly attributed to GvHD disease in 2 patients, while the third patient died of Streptococcus viridans sepsis and bone marrow aplasia 1 year after transplant, presumably also due to GvHD.
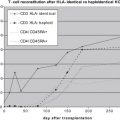
Other centers using MUD BMT for SCID also achieved excellent engraftment, with survival ranging from 71.5% to 83.3%. These reports suffered from drawbacks such as the small number of patients in each study, which represented only single centers and lacked long-term evaluation of immune reconstitution. Therefore, in 2004 the authors initiated a study comparing the outcome of 94 patients with SCID who received BMT from 1990 until 2004 at the Hospital for Sick Children, Toronto, Canada and Brescia, Italy. Of importance, this study contained the largest group of patients with SCID to have undergone MUD BMT. The study also provided a unique opportunity for direct and detailed comparison of 40 patients transplanted using HLA-mismatched related donors (MMRD), mostly HID, with 41 patients transplanted with MUD. The clinical presentation, age of diagnosis, molecular diagnosis, and gender, as well as maintenance prior to and after BMT were similar in both centers and among both transplant groups ( Table 1 ). Of note is that among 9 patients initially considered as clinically unstable, 4 could be stabilized and only a few required “rush” BMT. The latter emphasizes that while the diagnosis and initial treatment of SCID is a medical emergency, once patients have been stabilized, the BMT itself should be performed with the best available donor.
| MUD (N = 41) | MMRD (N = 40) | P | |
|---|---|---|---|
| Males/females | 28/13 | 29/11 | 0.78 |
| Diagnosis before 3 mo of age | 11 | 14 | 0.43 |
| Diagnosis between 3 and 12 mo of age | 27 | 25 | 0.75 |
| Diagnosis after 12 mo of age | 3 | 1 | 0.32 |
| Failure to thrive | 13 | 8 | 0.17 |
| Lung disease | 14 | 19 | 0.16 |
| Diarrhea | 5 | 9 | 0.17 |
| Rash | 6 | 8 | 0.36 |
| Candida | 6 | 7 | 0.48 |
| Unstable clinical condition | 4 | 5 | 0.48 |
| No clinical abnormalities | 8 | 6 | 0.40 |
| T−B+NK− immune phenotype | 14 | 16 | 0.29 |
| T−B−NK+ immune phenotype | 12 | 15 | 0.20 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree