The herpes viruses are responsible for a wide range of diseases in patients following transplant, resulting from direct viral effects and indirect effects, including tumor promotion. Effective treatments and prophylaxis exist for the neurotropic herpes viruses HSV-1, HSV-2, varicella zoster virus, and possibly HHV-6. Antivirals seem to be less effective at prevention of the tumor-promoting effects of Epstein-Barr virus and HHV-8. Reduction in immunosuppression is the cornerstone to treatment of many diseases associated with herpes virus infections.
The herpes viruses comprise a large group of enveloped DNA-containing viruses that characteristically cause latent infection in their respective hosts. There are 8 known herpes family viruses associated with human infection: herpes simplex virus (HSV) types 1 and 2, varicella zoster virus (VZV), Epstein-Barr virus (EBV), Cytomegalovirus (CMV), Human herpesvirus 6 (HHV-6), Human herpesvirus 7 (HHV-7), and Human herpesvirus 8 (HHV-8). Of these, CMV has received the most attention as a cause of morbidity and mortality among transplant recipients and is discussed separately in articles by Ljungman, Strasfeld, Hirsch, and Einsele in this issue. The remaining herpes viruses are also responsible for significant disease in the transplant patient population. The role of each of these viruses as a cause of disease in the transplant population is discussed in this article.
HSV-1 and HSV-2
The α-herpes viruses, HSV-1 and HSV-2, are responsible for oral and genital mucocutaneous ulcers in the general population. HSV-2 is generally considered to be sexually transmitted and primarily infects the urogenital mucosa, whereas HSV-1 predominantly affects the oral mucosa and is often transmitted through nonsexual contact. Both viruses are neurotropic and primarily infect neurons in their latent forms. Reactivation of HSV is common among transplant recipients, and is the second most common cause of viral infection after transplantation.
Most HSV-1 and HSV-2 infections occur in the setting of reactivation rather than primary infection, although primary HSV infections are well documented, particularly among younger patients. Primary infection from transplanted tissue is uncommon but has been observed in renal transplant recipients. The high percentage of cases attributed to reactivation is undoubtedly a result of a high baseline population seroprevalence of HSV-1 and HSV-2. Seroprevalence increases with age and varies by geographic, racial, socioeconomic, and ethnic characteristics among the general population. Antibodies to HSV-1 were found in 50% to 96% of people in previous seroprevalence studies. Analysis of Americans from the National Health and Nutrition Examination Survey showed the seroprevalence of HSV-1 to be 65% and HSV-2 to be 26% by age 49 years. Higher rates of seropositivity were found in women and minorities in the same survey. The greatest risk factor for reactivation of HSV following transplantation is lack of antiviral prophylaxis.
Before the introduction of acyclovir, reactivation of HSV infection was estimated to occur in up to 80% of patients receiving hematopoetic stem cell transplant. Lower, but still substantial, reactivation rates were described in solid-organ transplant recipients in the years before effective antiviral prophylaxis. The clinical manifestations of HSV infection range from limited mucocutaneous outbreaks to disseminated infections involving visceral organs and the central nervous system (CNS).
The most common manifestations of HSV are mucocutaneous outbreaks, usually involving the oral and genitourinary mucosa. These infections, which can lead to extensive mucosal involvement, typically occur in the first 30 days following transplantation if prophylaxis is not administered. Less common manifestations of HSV involving the lungs and viscera are also described. Pneumonia as a result of HSV-1 and HSV-2 is typically preceded by gingivostomatitis, however pulmonary involvement from disseminated infection and airway manipulation may also occur. The diagnosis of HSV pneumonia is complicated because viral shedding within the airways is common in immunosuppressed and critically ill adults and does not necessarily reflect true pneumonia. The use of acyclovir in critically ill patients with HSV isolated from respiratory secretions has not been shown to influence mortality, ventilator dependence, or length of hospitalization. Therefore, caution should be taken in interpreting results from viral cultures, direct fluorescent antibody staining, and nucleic acid assays without associated cytopathic evidence of infection on tissue biopsy.
Hepatitis is an uncommon manifestation of HSV that is described in several case reports and case series. When HSV presents with hepatitis there is often evidence of disseminated disease with involvement of the skin and mucous membranes. Patients may seem well initially, with elevated liver function tests as the only sign of infection. More often, patients present with nonspecific flulike symptoms of fever, malaise, and myalgias. Increasing levels of aspartate aminotransferase and alanine aminotransferase, sometimes 10 to 20 times the upper limit of normal, are often observed. Cross-sectional imaging may appear normal, but in some cases liver infiltration with microabscesses has been observed. Most cases occur within 30 days of transplant, however some cases have occurred years after transplant. Nearly all HSV hepatitis cases in the literature occurred in patients while off antiviral prophylaxis. Diagnosis is made by liver biopsy with culture and antibody staining for HSV-1 and HSV-2. Pathology typically reveals necrotic hepatitis with loss of lobular architecture. Other visceral manifestations of HSV infection in immunosuppressed hosts include esophagitis, gastritis, and colitis.
Encephalitis as a result of HSV infection is rare in the transplant population. On presentation, confusion, fever, and behavioral changes are the predominant findings. Up to one-third of patients present with seizure and one-fifth with focal neurologic findings. Cerebrospinal fluid (CSF) typically has a lymphocytic pleocytosis and increased protein level. The diagnosis of HSV encephalitis is now usually made by polymerase chain reaction (PCR) from CSF rather than brain biopsy. In the general population, on which most research on HSV encephalitis has been conducted, significant neurologic compromise is common following HSV encephalitis. The early initiation of high-dose acyclovir was shown to significantly decrease the morbidity and mortality from HSV encephalitis. In a large cohort of immunocompetent and immunosuppressed patients, long-term neurologic deficits were common despite antiviral treatment. There are insufficient data in the era of antiviral prophylaxis to know if outcomes are worse in transplant recipients.
The introduction of oral and intravenous acyclovir in the 1980s markedly decreased the incidence of serious HSV infections following transplantation. Several small randomized trials demonstrated intravenous and oral acyclovir to be safe and effective as a prophylactic regimen against HSV infections. Acyclovir appeared to abbreviate viral shedding and expedite healing from mucocutaneous outbreaks in hematopoetic stem cell transplant recipients. Since the introduction of acyclovir, related compounds such as valacyclovir and famciclovir have also been used successfully for treatment of HSV and varicella zoster infections following transplantation. Ganciclovir also has activity against HSV, and its use in the posttransplant population has been shown to significantly decrease rates of reactivation. Resistance to acyclovir and its derivatives does occur and typically reflects prolonged exposure to inadequate dosing of acyclovir at the time of viral reactivation. The highest rates of acyclovir resistance are found in allogeneic stem cell transplant recipients with estimates ranging from 1% to 14% of patients with resistant virus. Second-line treatment with foscarnet is typically used if acyclovir resistance is detected.
VZV
VZV, the α-herpes virus responsible for chickenpox and shingles, causes symptomatic infection through reactivation or primary infection in approximately 1% to 20% of solid-organ transplant recipients, with lung transplant recipients having the highest rates. The rate of VZV disease approaches more than 40% in hematopoetic stem cell transplant recipients. Reactivation of VZV is the most common route of VZV disease in adult transplant recipients, with more than 90% of adults in the United States estimated to have antibodies against VZV. In previous series, the median time frame for reactivation ranged from 9 to 23 months following solid-organ transplant. In hematopoietic cell transplant recipients most cases of VZV disease tends to occur within the first 12 months following transplantation, with up to 26% of transplant recipients developing disease following discontinuation of antiviral prophylaxis. Suggested risk factors for VZV disease in solid-organ transplant include mycophenolate use, recent treatment of rejection, induction therapy, and age greater than 50 years. All solid-organ transplant candidates should be tested before transplantation for VZV antibodies in an effort to determine the risk for primary infection. Solid-organ transplant candidates with VZV IgG negative status should undergo vaccination with the live attenuated Oka strain VZV vaccine before solid-organ transplant. The vaccine should not be given after transplant because it is a live vaccine and there are currently insufficient data to determine its safety in immunosuppressed transplant recipients. The rate of VZV disease (primary and reactivation) in allogeneic stem cell transplant recipients remains high regardless of VZV serostatus before transplant. An investigational inactivated varicella vaccine was successfully used to prevent disease in autologous hematopoetic stem cell transplant recipients; however it is currently not available.
As with HSV, the clinical manifestations of VZV disease are wide ranging, but can be severe and associated with increased mortality, especially in the early posttransplant period. Primary infection with VZV in the posttransplant setting can be severe, with disseminated infection presenting with skin, lung, and visceral organ involvement. Donor-derived VZV infections are rare, but have been reported. The most common presentation of VZV is cutaneous infection, typically with single dermatomal involvement. However, multiple dermatome involvement occurs in a sizable minority of cases. In cases of disseminated disease, typical vesicular skin lesions remain a common marker of disease. It is notable that the rash is not always vesicular in immunosuppressed hosts; consequently biopsy of the skin may be required for viral identification either by direct fluorescence or nucleic acid detection or culture. Patients may present with other symptoms of disseminated disease, including abdominal pain or hepatitis before the onset of rash. CNS involvement with VZV can present with encephalitis, myelitis, or meningoencephalitis. Unlike disseminated cutaneous infections, CNS VZV often presents without skin or other organ involvement. The diagnosis of VZV CNS infection is typically made by detection of VZV in the CSF using nucleic acid testing in conjunction with a compatible clinical presentation. CSF typically shows a lymphocyte predominant pleocytosis, moderately increased protein level and normal to low-normal glucose level. All cases of disseminated zoster should be placed in isolation once the diagnosis is suspected in an effort to prevent spread to other immunocompromised patients and susceptible health care workers.
Treatment of VZV disease is generally recommended for all transplant recipients. High-dose acyclovir or its analogues has been successfully used for the treatment of localized and disseminated VZV infections. In cases of disseminated disease and CNS infection, intravenous acyclovir (30 mg/kg/d in 3 divided doses) is preferred as initial therapy. Ganciclovir has not been studied specifically in the treatment of VZV, however it has been used successfully for treatment in several reports. Oral agents, such as valacyclovir (1 g every 8 hours), acyclovir (800 mg 5 times each day) and famciclovir (500 mg every 8 hours) are reasonable choices for localized infections. In rare cases where acyclovir resistance occurs, foscarnet can be used.
Several studies have shown acyclovir and ganciclovir to be effective as prophylaxis against VZV reactivation in the posttransplant period. Other methods of preventing primary infection in VZV-negative transplant recipients (who were not vaccinated before transplant or failed to mount a detectable VZV antibody titer) include vaccinating household and close contacts at risk for primary infection, preferably before transplant. VZV seronegative patients exposed to persons with active VZV (either chicken pox or shingles) should ideally be given postexposure prophylaxis with intravenous varicella zoster immunoglobulin (VZIG) given within the first 96 hours of exposure. Unfortunately, VZIG is no longer available in the United States. An intramuscularly dosed formulation of concentrated VZV IgG (VariZIG, Cangene Corp, Winnepeg, Canada) is available through an investigational new drug expanded access protocol from the Food and Drug Administration ( http://www.fda.gov/BiologicsBloodVaccines/SafetyAvailability/ucm176029.htm ). There are currently insufficient data to support the use of antiviral agents after VZV exposure, and it is currently not recommended by the Centers of Disease Control’s Advisory Committee on Immunization Practices.
VZV
VZV, the α-herpes virus responsible for chickenpox and shingles, causes symptomatic infection through reactivation or primary infection in approximately 1% to 20% of solid-organ transplant recipients, with lung transplant recipients having the highest rates. The rate of VZV disease approaches more than 40% in hematopoetic stem cell transplant recipients. Reactivation of VZV is the most common route of VZV disease in adult transplant recipients, with more than 90% of adults in the United States estimated to have antibodies against VZV. In previous series, the median time frame for reactivation ranged from 9 to 23 months following solid-organ transplant. In hematopoietic cell transplant recipients most cases of VZV disease tends to occur within the first 12 months following transplantation, with up to 26% of transplant recipients developing disease following discontinuation of antiviral prophylaxis. Suggested risk factors for VZV disease in solid-organ transplant include mycophenolate use, recent treatment of rejection, induction therapy, and age greater than 50 years. All solid-organ transplant candidates should be tested before transplantation for VZV antibodies in an effort to determine the risk for primary infection. Solid-organ transplant candidates with VZV IgG negative status should undergo vaccination with the live attenuated Oka strain VZV vaccine before solid-organ transplant. The vaccine should not be given after transplant because it is a live vaccine and there are currently insufficient data to determine its safety in immunosuppressed transplant recipients. The rate of VZV disease (primary and reactivation) in allogeneic stem cell transplant recipients remains high regardless of VZV serostatus before transplant. An investigational inactivated varicella vaccine was successfully used to prevent disease in autologous hematopoetic stem cell transplant recipients; however it is currently not available.
As with HSV, the clinical manifestations of VZV disease are wide ranging, but can be severe and associated with increased mortality, especially in the early posttransplant period. Primary infection with VZV in the posttransplant setting can be severe, with disseminated infection presenting with skin, lung, and visceral organ involvement. Donor-derived VZV infections are rare, but have been reported. The most common presentation of VZV is cutaneous infection, typically with single dermatomal involvement. However, multiple dermatome involvement occurs in a sizable minority of cases. In cases of disseminated disease, typical vesicular skin lesions remain a common marker of disease. It is notable that the rash is not always vesicular in immunosuppressed hosts; consequently biopsy of the skin may be required for viral identification either by direct fluorescence or nucleic acid detection or culture. Patients may present with other symptoms of disseminated disease, including abdominal pain or hepatitis before the onset of rash. CNS involvement with VZV can present with encephalitis, myelitis, or meningoencephalitis. Unlike disseminated cutaneous infections, CNS VZV often presents without skin or other organ involvement. The diagnosis of VZV CNS infection is typically made by detection of VZV in the CSF using nucleic acid testing in conjunction with a compatible clinical presentation. CSF typically shows a lymphocyte predominant pleocytosis, moderately increased protein level and normal to low-normal glucose level. All cases of disseminated zoster should be placed in isolation once the diagnosis is suspected in an effort to prevent spread to other immunocompromised patients and susceptible health care workers.
Treatment of VZV disease is generally recommended for all transplant recipients. High-dose acyclovir or its analogues has been successfully used for the treatment of localized and disseminated VZV infections. In cases of disseminated disease and CNS infection, intravenous acyclovir (30 mg/kg/d in 3 divided doses) is preferred as initial therapy. Ganciclovir has not been studied specifically in the treatment of VZV, however it has been used successfully for treatment in several reports. Oral agents, such as valacyclovir (1 g every 8 hours), acyclovir (800 mg 5 times each day) and famciclovir (500 mg every 8 hours) are reasonable choices for localized infections. In rare cases where acyclovir resistance occurs, foscarnet can be used.
Several studies have shown acyclovir and ganciclovir to be effective as prophylaxis against VZV reactivation in the posttransplant period. Other methods of preventing primary infection in VZV-negative transplant recipients (who were not vaccinated before transplant or failed to mount a detectable VZV antibody titer) include vaccinating household and close contacts at risk for primary infection, preferably before transplant. VZV seronegative patients exposed to persons with active VZV (either chicken pox or shingles) should ideally be given postexposure prophylaxis with intravenous varicella zoster immunoglobulin (VZIG) given within the first 96 hours of exposure. Unfortunately, VZIG is no longer available in the United States. An intramuscularly dosed formulation of concentrated VZV IgG (VariZIG, Cangene Corp, Winnepeg, Canada) is available through an investigational new drug expanded access protocol from the Food and Drug Administration ( http://www.fda.gov/BiologicsBloodVaccines/SafetyAvailability/ucm176029.htm ). There are currently insufficient data to support the use of antiviral agents after VZV exposure, and it is currently not recommended by the Centers of Disease Control’s Advisory Committee on Immunization Practices.
EBV
EBV is a gammaherpes virus responsible for several clinical entities. In the general population, EBV is the causative agent of infectious mononucleosis, Burkitt lymphoma, and nasopharyngeal carcinoma. The role of EBV as a cause of posttransplant lymphoproliferative disorder (PTLD) is now well established, accounting for 90% of cases of PTLD. Other rare disorders attributed to EBV in the posttransplant period include smooth muscle tumors and the hemophagocytic syndrome. EBV is ubiquitous, with up to 90% seropositivity observed in the general community. Infection in early childhood is common and often without significant symptoms. The clinical entity of mononucleosis, characterized by pharyngitis, lymphadenopathy, and fatigue, is typically seen with primary infection in young immunocompetent adults. Rarely, neurologic manifestations of EBV infection, including encephalitis and optic neuritis, occur. Like other herpes viruses, EBV is a chronic infection, with latent virus infecting B cells in the blood and lymphoid tissues. The virus is typically transmitted to naive individuals through saliva and respiratory secretions. Transmissions to naive transplant recipients through blood transfusion and organ transplant are also described.
The clinical entity known as PTLD comprises a spectrum of disease characterized by the abnormal proliferation of lymphocytic cells, often with an invasive component, in patients following transplantation. The clinical manifestations of PTLD vary considerably. In some instances patients are asymptomatic and disease is only suggested by incidental imaging findings. Other cases may present with a mononucleosis-like syndrome, organ dysfunction secondary to tissue infiltration or septic-appearing febrile illness. Tissue infiltration from PTLD may present as extranodal masses, which can involve various organs, including the lungs, liver, spleen, bowels, and CNS. In some instances, allografts are the primary site of PTLD, with resulting organ dysfunction mimicking rejection. PTLD may present as an infiltrative process rather than a focal mass, mimicking such entities as pneumonia, lymphocele, and colitis.
Numerous risk factors for the development of PTLD are described. Host EBV seronegative status has been shown to increase the risk of developing PTLD up to 76-fold, making the issue particularly troublesome for pediatric patients. These patients, at risk for primary EBV infection, are most likely to present with disease within only a few months of transplant. Other risk factors in solid-organ transplant recipients, reflect a state of actual or potentially augmented immune suppression and include CMV disease, CMV donor/recipient mismatch, and intensity of pharmacologically mediated immune suppression. Risk factors for PTLD in hematopoetic stem cell recipients include unrelated donor HLA mismatch, use of antithymocyte globulin, T-cell depletion, and use of anti-CD3 monoclonal antibodies for graft-versus-host disease prophylaxis.
The initial diagnosis of PTLD is best made with tissue, ideally from an excisional biopsy specimen. High serum levels of EBV DNA may be seen in PTLD, especially in younger recipients, and may precede clinical disease. Currently, the incongruity in EBV DNA testing methods between centers and the need for tissue for pathologic grading, argue against the use of EBV viral load testing as replacement for histologic diagnosis, although it is estimated that up to 90% of PTLD is EBV-associated. The Society of Hematopathology classification schema for PTLD divides lesions into 3 general categories: lymphoid hyperplasia (early lesions), polymorphic PTLD, and lymphomatous (monomorphic) PTLD. Lymphoid hyperplasia, sometimes referred to as early PTLD, is subcharacterized into posttransplant infectious mononucleosis and reactive plasmacytic hyperplasia. A notable characteristic in both of these groups is the presence of polyclonal cell populations. Polymorphic PTLD is characterized by more aggressive lesions that escape the normal lymphatic system boundaries and infiltrate underlying tissue. Although these lesions behave similarly to malignant lymphoma, the cell population involved remains heterogeneous in appearance, although they are all typically monoclonal at the molecular level. The term monomorphic PTLD is used to describe lymphomas in the posttransplant setting. Many are associated with EBV, although some are not. These lesions are generally categorized according to the Revised European American Lymphoma system with the suffix PTLD to note the correlation with transplant status.
Treatment varies considerably depending on which variation of PTLD is diagnosed. A cornerstone of therapy is decreasing the level of immunosuppression whenever possible. In 1 series of solid-organ transplant recipients treated for PTLD, 63% of patients treated by reducing immunosuppression alone had complete disease remission. Risk factors for failing treatment with reduction of immunosuppression included a high baseline lactate dehydrogenase level, multiorgan involvement, presence of B symptoms, and organ dysfunction from disease. The data for antiviral medications in the treatment of PTLD through suppression of EBV are limited. Although early reports suggested acyclovir and ganciclovir, which have some in vitro activity against EBV, might have a potential role in PTLD treatment there is no compelling clinical data to support their use. Treatment with immunomodulatory agents such as anti-CD-20 (rituximab), interleukin 6 (IL-6) and interferon-α is described. Infusions of cytotoxic EBV-specific T cells have also been used as a therapeutic and prophylactic treatment in solid-organ and hematopoetic stem cell transplant recipients. As a treatment, results have been mixed and no controlled trials have been published on the subject. The use of cytotoxic EBV-specific T cells as a prophylactic measure in individuals with high levels of circulating EBV DNA were also reported to be beneficial, but data are limited to small uncontrolled series. In some cases treatment with chemotherapeutic agents used in nontransplant-associated lymphomas are also used, often in conjunction with rituximab. Other strategies include resection of localized tumors, radiotherapy, and treatment of other infections, such as CMV, that may act to suppress the immune system further. In cases where reduction of immunosuppression has resulted in graft loss, retransplantation can be successful.
The use of antivirals gained some support as a prophylactic measure against EBV based on the results of some uncontrolled studies. A randomized controlled trial exploring the use of ganciclovir and acyclovir as a prophylactic strategy for EBV and CMV did not show any decrease in PTLD, however. The use of quantitative EBV viral load monitoring has been advocated as another method to prevent the development of PTLD in high-risk individuals. In this approach regular quantitative EBV viral loads are obtained and immunosuppression is decreased when viral loads reach a predetermined threshold.
HHV-6 and HHV-7
HHV-6, the causative agent of the common childhood disease roseola infantum (exanthem sabitum), has received attention in the past several years as an opportunistic infection in the posttransplant population. The virus, first described in 1986, is a member of the β-herpes virus family, and establishes latency in CD4+ T lymphocytes. Genetic sequencing has demonstrated 2 variants, A and B. The B variant has been linked to most disease in children and in the transplant population. It is estimated that greater than 90% of children are seropositive for HHV-6 by 1 year of age. Therefore, most cases of HHV-6 viremia are believed to be caused by viral reactivation, although primary infection following transplantation has been described.
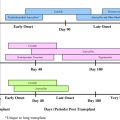
Reactivation of HHV-6 is common in the immediate period following hematopoetic stem cell transplant, when immunosuppression is highest. A prospective study by Zerr and colleagues detected HHV-6 viremia in 52 of 110 (47%) patients evaluated during the first 100 days after transplant. Numerous indirect effects have been suggested related to HHV-6 viremia in the hematopoetic stem cell transplant population. These include delayed engraftment, higher rates of graft-versus-host disease, cytomegalovirus disease, and all-cause mortality. Estimates of HHV-6 viremia following solid-organ transplant range from 24% to 66%, although this is likely reduced in patients receiving ganciclovir for CMV prophylaxis. Reported indirect effects associated with HHV-6 viremia include higher frequencies of allograft rejection, severe CMV disease, and invasive fungal infections. Despite these associations, no causal link has been definitively established between HHV-6 reactivation and indirect effects. A recent prospective cohort study that included 298 solid-organ transplant recipients found no connection between severity or duration of CMV disease and HHV-6 coinfection.
Several case series and reports have linked HHV-6 with encephalitis in solid-organ and hematopoetic stem cell transplant recipients. Most of the cases reported in the literature occurred 30 to 90 days after transplant. Manifestations of neurologic disease include generalized confusion, amnesia, insomnia, seizures (often subclinical), and coma. Magnetic resonance imaging imaging of the brain often reveals involvement of the basal ganglia. The detection of HHV-6 in CSF through PCR or culture, in conjunction with compatible neuroradiology and clinical manifestations, is highly suggestive of HHV-6 encephalitis. Nonetheless, other causes of encephalitis should be ruled out as HHV-6 has been detected in the CSF of asymptomatic patients and the symptoms of HHV-6 encephalitis may be strikingly similar to those of immunosuppression leukoencephalopathy. Other manifestations of HHV-6 disease reported in the literature include gastroenteritis, pneumonitis, hepatitis, and myelosuppression.
No prospective clinical trials have evaluated the use of antiviral medications in the treatment of HHV-6 associated disease. In vitro data suggest that HHV-6 is inhibited by ganciclovir, foscarnet, and cidofovir. Most clinical experience has been with the treatment of HHV-6 encephalitis. Most reported cases used ganciclovir, foscarnet, or a combination of both with varying success. Despite their in vitro activity against HHV-6, neither intravenous ganciclovir nor valganciclovir affected HHV-6 viral loads in a multicenter prospective clinical trial of CMV disease treatment.
The β-herpes virus, HHV-7, is closely related to HHV-6 but its role in clinically relevant disease remains unclear. In children, HHV-7 has been associated with rare cases of exanthem subitum, febrile seizures, and encephalitis. A few cases of encephalitis and myelitis have been attributed to HHV-7 among hematopoetic stem cell transplant recipients. In comparison with HHV-6, however, little data exist supporting organ-specific infections with HHV-7 in transplant recipients. Like HHV-6, HHV-7 has been proposed to act as an immunomodulatory virus, potentially lowering the barrier to other opportunistic infections, including CMV. A recent prospective multicenter cohort examined the effect of HHV-7 viremia in patients with diagnosed CMV disease and found no correlation with duration of CMV disease or CMV disease outcomes.
HHV-8
HHV-8 also known as Kaposi sarcoma–associated herpes virus, is responsible for the malignant entities of Kaposi sarcoma (KS) and primary effusion lymphoma (PEL), as well as some forms of multicentric Castleman disease (MCD). HHV-8 belongs to the γ-herpes virus family along with EBV and infects CD-19 positive B cells in its latent form. Unlike the other herpes viruses discussed earlier, the seroprevalence to HHV-8 is highly variable, depending on geography and behavioral risk factors. Of 13,984 Americans sampled in the National Health and Nutrition Survey, 1.5% were found to be seropositive for HHV-8. The highest rate of HHV-8 seropositivity in the United States was found in men who have sex with men, with a prevalence rate estimated to be 8.2%. Worldwide prevalence varies dramatically, with some areas of sub-Saharan Africa estimated to have 30% to 50% seropositivity.
Transmission of HHV-8 is believed to occur through sexual activity and possibly through saliva. In endemic regions both means of transmission probably occur. Elsewhere, such as in North America, sexual activity is believed to be the primary mode of transmission. Transmission of HHV-8 has also been documented through solid-organ and hematopoetic stem cell transplantation.
Manifestations of HHV-8 disease in transplant recipients are variable. In the Middle East, where seroprevalence for HHV-8 reaches 25%, KS is the most common malignancy following renal transplant. The incidence is lower in North America. Prior series describing KS following solid-organ transplant reported onset of disease ranging from 2 to 23 months after transplant. Lesions may present as focal nodules on the skin, within organs (including allografts), or as disseminated disease with lymph node, bone marrow, and splenic infiltration. The diagnosis of KS is made by pathologic examination of affected tissues.
As with EBV-associated PTLD, reduction in immunosuppression is the first-line therapy for KS and is often curative. Some investigators have suggested that using sirolimus instead of other calcineurin inhibitors may provide additional treatment effect by inhibition of vascular endothelial cell growth factor. Chemotherapy and radiation may also be necessary in cases where reduction of immunosuppression is ineffective or not possible. Antiviral medications have not been shown to be useful in the treatment of KS.
Other rare manifestations of HHV-8 reported in transplant recipients include MCD and PEL. MCD is an aggressive lymphoproliferative disorder characterized by fever, diffuse lymphadenopathy, wasting, and hepatosplenomegally. HHV-8 is not always found in MCD, but is common, with virus detected in 75% of MCD lesions in 1 series. The diagnosis of MCD is made by tissue biopsy. Other causes of diffuse lymphadenopathy, such as disseminated mycobacterial and fungal infections, should be ruled out. The reported outcomes of MCD in transplant recipients are poor, with rapidly fatal disease or allograft failure in several reports. Treatments with immunomodulatory agents, chemotherapy, and antivirals have all been used with variable results.
PEL, also known as body cavity lymphoma, typically presents with a refractory exudative effusion in 1 of several potential spaces within the body. Lymphomatous cells fill the affected cavity, with tumor foci often studding the serous membranes. The most frequent location is the pleural space, however pericardial, peritoneal, and intracranial cases are also reported. Diagnosis is made by pathologic evaluation of effusion cells. HHV-8 PCR of the effusion may also be helpful in making a diagnosis. Other causes of exudative effusions should be ruled out, including infectious entities such as tuberculosis and empyema. Treatment experience of transplant-associated PEL is limited. Reduction in immunosuppression may be useful, as with KS and MCD. Antivirals have not been shown to offer much benefit and chemotherapy remains the treatment of choice in most cases.
Summary
The herpes viruses are responsible for a wide range of diseases in patients following transplant. The development of effective antiviral prophylaxis against HSV and VZV has substantially reduced the morbidity and mortality associated with these infections. Nonetheless, primary disease and reactivation of HSV and VZV can cause significant harm if not treated promptly. The role of EBV as a major cause of PTLD continues to pose a significant challenge. Current therapies focus on reduction of immunosuppression, chemotherapy, and rituximab therapy. There are few data to support antiviral therapy for EBV-associated PTLD, however ganciclovir may have a prophylactic effect, either by indirect or direct means. HHV-6 and -7 may have several indirect effects on transplant patients, including increased risk of infections and rejection episodes. These effects may be related to the viruses’ effect on immune cell function. The evidence for HHV-6 as a cause of posttransplant encephalitis is growing. Treatment with ganciclovir and/or foscarnet may be beneficial. The role of HHV-8 in posttransplant KS is well established. Reduction in immune suppression is the mainstay of therapy; in some cases alteration of immunosuppression to include sirolimus may be effective. Other manifestations of HHV-8 infection, including PEL and MCD may require chemotherapy in conjunction with reduction in immunosuppression. Antivirals have not been shown to be beneficial in the treatment of KS or PEL.
Dr Shiley has no financial disclosures.
Dr Blumberg receives financial support from Roche Pharmaceuticals for research support and consulting services. She also receives research support from Viropharma as a site investigator in a multicenter trial.
A version of this article was previously published in the Infectious Disease Clinics of North America , 24:2.
EBV
EBV is a gammaherpes virus responsible for several clinical entities. In the general population, EBV is the causative agent of infectious mononucleosis, Burkitt lymphoma, and nasopharyngeal carcinoma. The role of EBV as a cause of posttransplant lymphoproliferative disorder (PTLD) is now well established, accounting for 90% of cases of PTLD. Other rare disorders attributed to EBV in the posttransplant period include smooth muscle tumors and the hemophagocytic syndrome. EBV is ubiquitous, with up to 90% seropositivity observed in the general community. Infection in early childhood is common and often without significant symptoms. The clinical entity of mononucleosis, characterized by pharyngitis, lymphadenopathy, and fatigue, is typically seen with primary infection in young immunocompetent adults. Rarely, neurologic manifestations of EBV infection, including encephalitis and optic neuritis, occur. Like other herpes viruses, EBV is a chronic infection, with latent virus infecting B cells in the blood and lymphoid tissues. The virus is typically transmitted to naive individuals through saliva and respiratory secretions. Transmissions to naive transplant recipients through blood transfusion and organ transplant are also described.
The clinical entity known as PTLD comprises a spectrum of disease characterized by the abnormal proliferation of lymphocytic cells, often with an invasive component, in patients following transplantation. The clinical manifestations of PTLD vary considerably. In some instances patients are asymptomatic and disease is only suggested by incidental imaging findings. Other cases may present with a mononucleosis-like syndrome, organ dysfunction secondary to tissue infiltration or septic-appearing febrile illness. Tissue infiltration from PTLD may present as extranodal masses, which can involve various organs, including the lungs, liver, spleen, bowels, and CNS. In some instances, allografts are the primary site of PTLD, with resulting organ dysfunction mimicking rejection. PTLD may present as an infiltrative process rather than a focal mass, mimicking such entities as pneumonia, lymphocele, and colitis.
Numerous risk factors for the development of PTLD are described. Host EBV seronegative status has been shown to increase the risk of developing PTLD up to 76-fold, making the issue particularly troublesome for pediatric patients. These patients, at risk for primary EBV infection, are most likely to present with disease within only a few months of transplant. Other risk factors in solid-organ transplant recipients, reflect a state of actual or potentially augmented immune suppression and include CMV disease, CMV donor/recipient mismatch, and intensity of pharmacologically mediated immune suppression. Risk factors for PTLD in hematopoetic stem cell recipients include unrelated donor HLA mismatch, use of antithymocyte globulin, T-cell depletion, and use of anti-CD3 monoclonal antibodies for graft-versus-host disease prophylaxis.
The initial diagnosis of PTLD is best made with tissue, ideally from an excisional biopsy specimen. High serum levels of EBV DNA may be seen in PTLD, especially in younger recipients, and may precede clinical disease. Currently, the incongruity in EBV DNA testing methods between centers and the need for tissue for pathologic grading, argue against the use of EBV viral load testing as replacement for histologic diagnosis, although it is estimated that up to 90% of PTLD is EBV-associated. The Society of Hematopathology classification schema for PTLD divides lesions into 3 general categories: lymphoid hyperplasia (early lesions), polymorphic PTLD, and lymphomatous (monomorphic) PTLD. Lymphoid hyperplasia, sometimes referred to as early PTLD, is subcharacterized into posttransplant infectious mononucleosis and reactive plasmacytic hyperplasia. A notable characteristic in both of these groups is the presence of polyclonal cell populations. Polymorphic PTLD is characterized by more aggressive lesions that escape the normal lymphatic system boundaries and infiltrate underlying tissue. Although these lesions behave similarly to malignant lymphoma, the cell population involved remains heterogeneous in appearance, although they are all typically monoclonal at the molecular level. The term monomorphic PTLD is used to describe lymphomas in the posttransplant setting. Many are associated with EBV, although some are not. These lesions are generally categorized according to the Revised European American Lymphoma system with the suffix PTLD to note the correlation with transplant status.
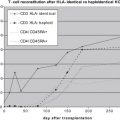
Treatment varies considerably depending on which variation of PTLD is diagnosed. A cornerstone of therapy is decreasing the level of immunosuppression whenever possible. In 1 series of solid-organ transplant recipients treated for PTLD, 63% of patients treated by reducing immunosuppression alone had complete disease remission. Risk factors for failing treatment with reduction of immunosuppression included a high baseline lactate dehydrogenase level, multiorgan involvement, presence of B symptoms, and organ dysfunction from disease. The data for antiviral medications in the treatment of PTLD through suppression of EBV are limited. Although early reports suggested acyclovir and ganciclovir, which have some in vitro activity against EBV, might have a potential role in PTLD treatment there is no compelling clinical data to support their use. Treatment with immunomodulatory agents such as anti-CD-20 (rituximab), interleukin 6 (IL-6) and interferon-α is described. Infusions of cytotoxic EBV-specific T cells have also been used as a therapeutic and prophylactic treatment in solid-organ and hematopoetic stem cell transplant recipients. As a treatment, results have been mixed and no controlled trials have been published on the subject. The use of cytotoxic EBV-specific T cells as a prophylactic measure in individuals with high levels of circulating EBV DNA were also reported to be beneficial, but data are limited to small uncontrolled series. In some cases treatment with chemotherapeutic agents used in nontransplant-associated lymphomas are also used, often in conjunction with rituximab. Other strategies include resection of localized tumors, radiotherapy, and treatment of other infections, such as CMV, that may act to suppress the immune system further. In cases where reduction of immunosuppression has resulted in graft loss, retransplantation can be successful.
The use of antivirals gained some support as a prophylactic measure against EBV based on the results of some uncontrolled studies. A randomized controlled trial exploring the use of ganciclovir and acyclovir as a prophylactic strategy for EBV and CMV did not show any decrease in PTLD, however. The use of quantitative EBV viral load monitoring has been advocated as another method to prevent the development of PTLD in high-risk individuals. In this approach regular quantitative EBV viral loads are obtained and immunosuppression is decreased when viral loads reach a predetermined threshold.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree