Chapter 58 Heparin-Induced Thrombocytopenia
Table 58-1 Risk Factors for Heparin-Induced Thrombocytopenia
| Heparin type: | Unfractionated > low-molecular-weight heparin > fondaparinux |
| Patient type: | Postoperative (major > minor surgery) > medical > obstetric/pediatric |
| Dose*: | Prophylactic dose > therapeutic dose > flushes |
| Duration: | 11-14 days† > 5-10 days > 4 days or fewer |
| Sex: | Female > male |
*Importance of heparin dose is uncertain because of confounding effect of patient type (e.g., postoperative patients tend to receive prophylactic-dose heparin whereas medical patients [e.g., with venous thromboembolism] are more likely to receive therapeutic-dose heparin); nevertheless, reported frequencies of heparin-induced thrombocytopenia (HIT) are relatively high in patients given postoperative prophylactic-dose heparin.
†Heparin exposure beyond 14 days does not usually increase the risk of HIT beyond that of an 11- to 14-day exposure.
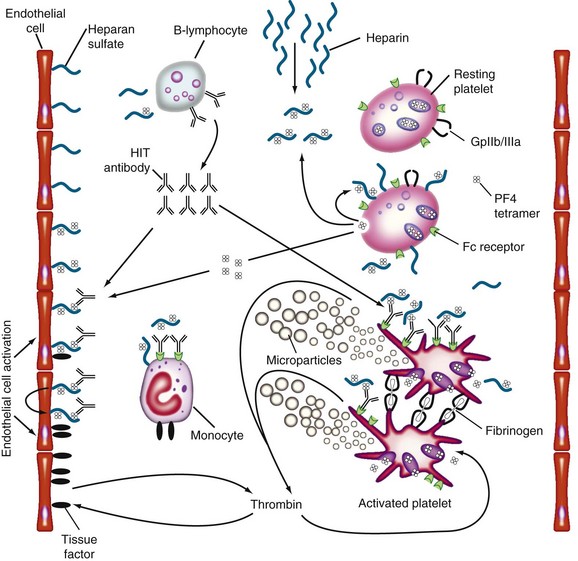
Figure 58-1 PATHOGENESIS OF HEPARIN-INDUCED THROMBOCYTOPENIA (HIT).
(Reprinted with permission from Greinacher A, Warkentin TE: Treatment of heparin-induced thrombocytopenia: An overview. In Warkentin TE, Greinacher A, editors: Heparin-induced thrombocytopenia, ed 4, New York, 2007, Informa Healthcare USA, p 287.)
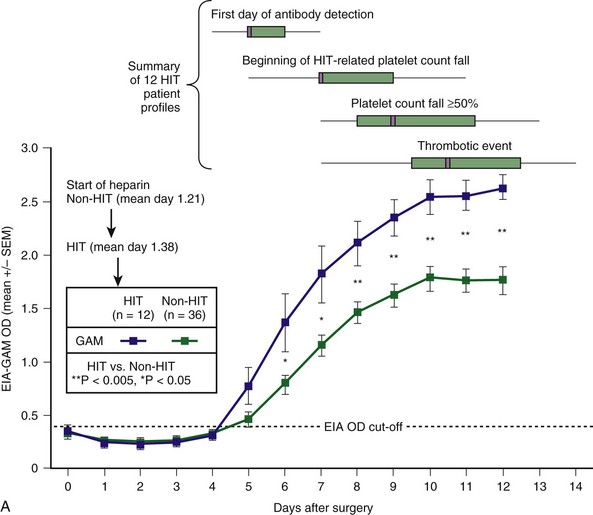
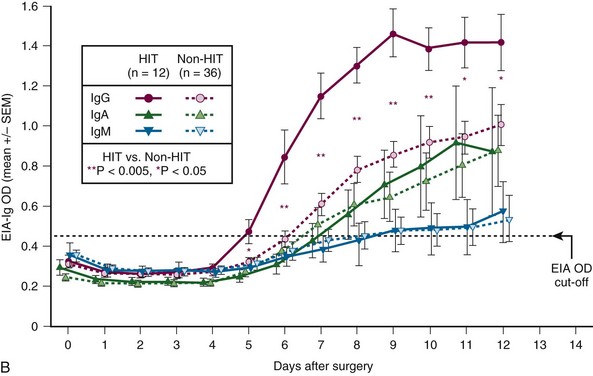
Figure 58-2 CHARACTERISTIC TIMELINE OF HEPARIN-INDUCED THROMBOCYTOPENIA (HIT).
(From Warkentin TE, Sheppard JI, Moore JC, et al: Studies of the immune response in heparin-induced thrombocytopenia. Blood 113:4693, 2009.)
Diagnostic Considerations in the Patient With Limb Ischemia and Thrombocytopenia
• Heparin-induced thrombocytopenia (HIT). Occlusion of large lower-limb arteries by platelet-rich “white clots” is characteristic of HIT. The major clue is an otherwise unexplained platelet count fall that begins 5 or more days after initiation of heparin. Urgent thromboembolectomy may be limb sparing. Sensitive assays for HIT antibodies give strongly positive results. See subsequent entry for warfarin.
• Adenocarcinoma-associated disseminated intravascular coagulation (DIC). Severe venous or arterial thrombosis can develop in patients with metastatic adenocarcinoma who have DIC. This often occurs within hours after stopping heparin. A clinical clue is an otherwise unexplained rise in platelet count that occurs with initial or repeated heparin therapy. See next entry for warfarin.
• Warfarin-induced phlegmasia cerulea dolens/venous limb gangrene. Coumarin anticoagulants, such as warfarin, can lead to venous ischemia (phlegmasia cerulea dolens) or venous limb gangrene in patients with DIC caused by HIT or adenocarcinoma. Limb loss can occur even though the limb pulses are palpable.
• Sepsis-associated microvascular thrombosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 , and seropositive non-HIT controls by
, and seropositive non-HIT controls by  . On each day beginning on postoperative day 6, there is a significant difference in the mean of the OD levels between the patients with HIT and the seropositive non-HIT controls (P < .05 by nonpaired t test). At the top of the figure, summary data for 12 HIT patient profiles are shown for four key events (first day of antibody detection, beginning of HIT-related platelet count fall, platelet count fall ≥50%, and thrombotic event), summarized as median (small purple squares within rectangles), interquartile range (rectangles), and range (ends of thin black lines). B, Mean (±SEM) OD values of anti-PF4/heparin antibodies detected using an in-house immunoassay (EIA-Ig) that detects antibodies of the individual immunoglobulin classes, IgG (red circles), IgA (green triangles), and IgM (blue inverted triangles) for HIT (solid symbols) and non-HIT (open symbols). On each postoperative day beginning on day 5, there is a significant difference in the mean of the OD units for the IgG immunoassay between the patients with HIT and the seropositive non-HIT controls (**P < .005 for days 6 to 10; *P < .05 for days 5, 11, and 12).
. On each day beginning on postoperative day 6, there is a significant difference in the mean of the OD levels between the patients with HIT and the seropositive non-HIT controls (P < .05 by nonpaired t test). At the top of the figure, summary data for 12 HIT patient profiles are shown for four key events (first day of antibody detection, beginning of HIT-related platelet count fall, platelet count fall ≥50%, and thrombotic event), summarized as median (small purple squares within rectangles), interquartile range (rectangles), and range (ends of thin black lines). B, Mean (±SEM) OD values of anti-PF4/heparin antibodies detected using an in-house immunoassay (EIA-Ig) that detects antibodies of the individual immunoglobulin classes, IgG (red circles), IgA (green triangles), and IgM (blue inverted triangles) for HIT (solid symbols) and non-HIT (open symbols). On each postoperative day beginning on day 5, there is a significant difference in the mean of the OD units for the IgG immunoassay between the patients with HIT and the seropositive non-HIT controls (**P < .005 for days 6 to 10; *P < .05 for days 5, 11, and 12).