24125
Hematopoietic Cell Transplantation for Older Patients
Sergio Giralt
INTRODUCTION
In 1974, Thomas et al. published their seminal paper of the use of high-dose chemoradiotherapy followed by the infusion of related human leucocyte antigen (HLA) compatible bone marrow in 100 patients with refractory acute leukemia (1). This paper demonstrated that high-dose chemoradiotherapy followed by an HLA-identical bone marrow transplant could result in long-term disease control in a fraction of patients with refractory acute leukemia.
Initially it was felt that most of the curative potential of this strategy was derived from the steep dose–response curve of alkylating agents and radiotherapy and tumor cell response in human tumors. Doubling the dose of alkylating agents increases tumor cell kill by a log or more, and increasing the dose of alkylating agents by 5- to 10-fold overcomes the resistance of tumor cells against lower doses. Thus, over the next 20 years, high-dose chemoradiotherapy followed by either autologous or allogeneic hematopoietic cell transplant (HCT) was extensively explored in a variety of hematologic and nonhematologic malignancies (2).
However, due to the toxic side effects of high-dose chemoradiotherapy and the intensive supportive care required during the period of intense myelosuppression after the conditioning regimen, allogeneic and autologous HCT was initially limited to younger patients with few if any comorbidities (1,2).
In 1997, the first reports of reduced-intensity conditioning (RIC) regimens appeared in the literature, with subsequent reports demonstrating that RIC regimens can be delivered to older patients or patients with comorbidities and achieve acceptable toxicities and outcomes (3–5). With the advent of RIC regimens and with improvements in supportive care, the average age of an HCT recipient for both autologous or allogeneic has increased significantly, as depicted in Figure 25.1, and is now considered standard of care for most patients over the age of 65; many transplant centers no longer have an age limit for the procedure (6). In this chapter, we summarize the rationale for exploring HCT in older patients, current indications and results, and future directions.
242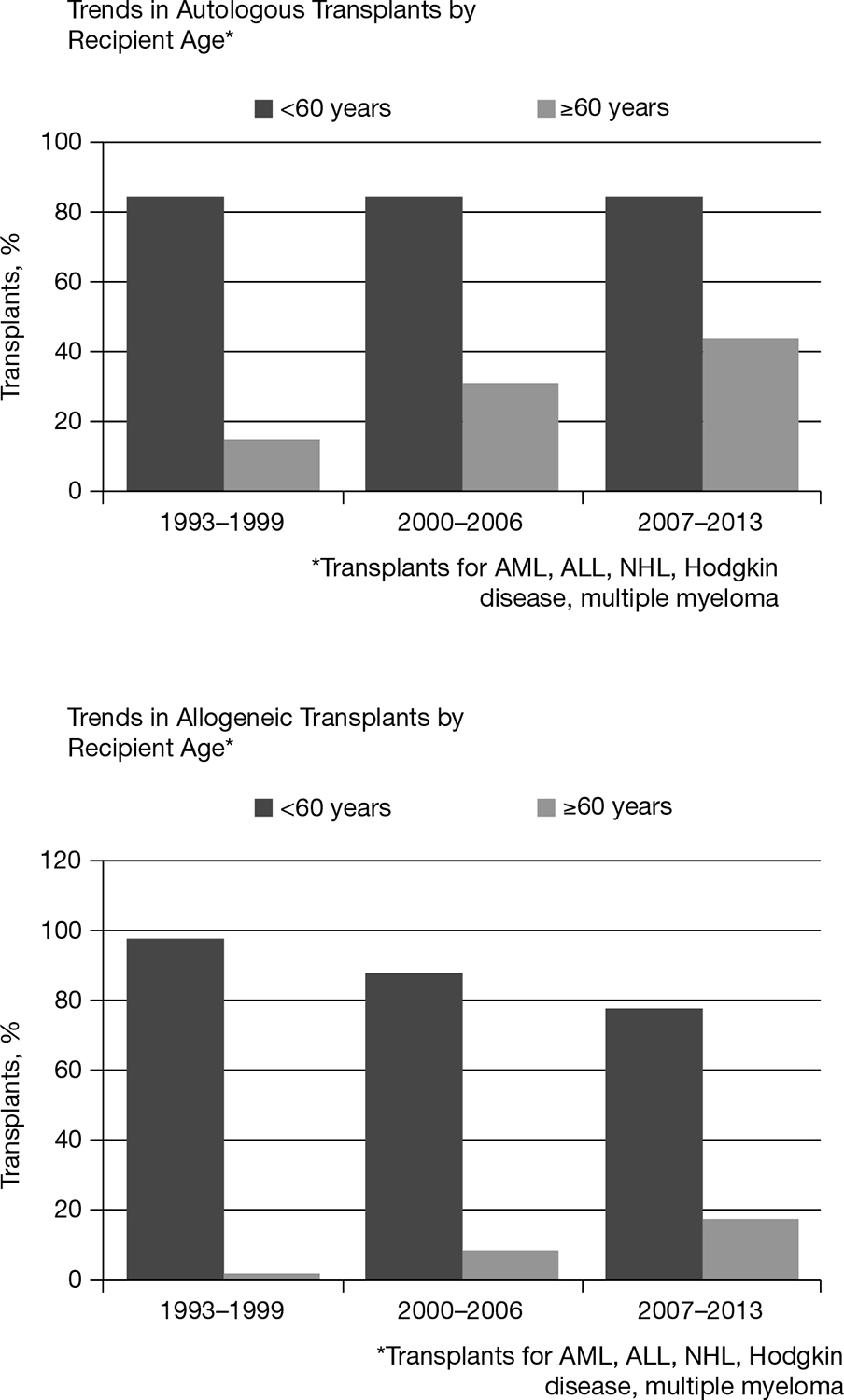
FIGURE 25.1 Trends in age of HCT recipients as reported to the Center for International Blood and Marrow Research.
ALL, acute lymphoblastic leukemia; AML, acute myeloid leukemia; NHL, non-hodgkin lymphoma; HCT, hematopoietic cell transplantation.
243RATIONALE FOR EXPLORING HCT IN OLDER PATIENTS
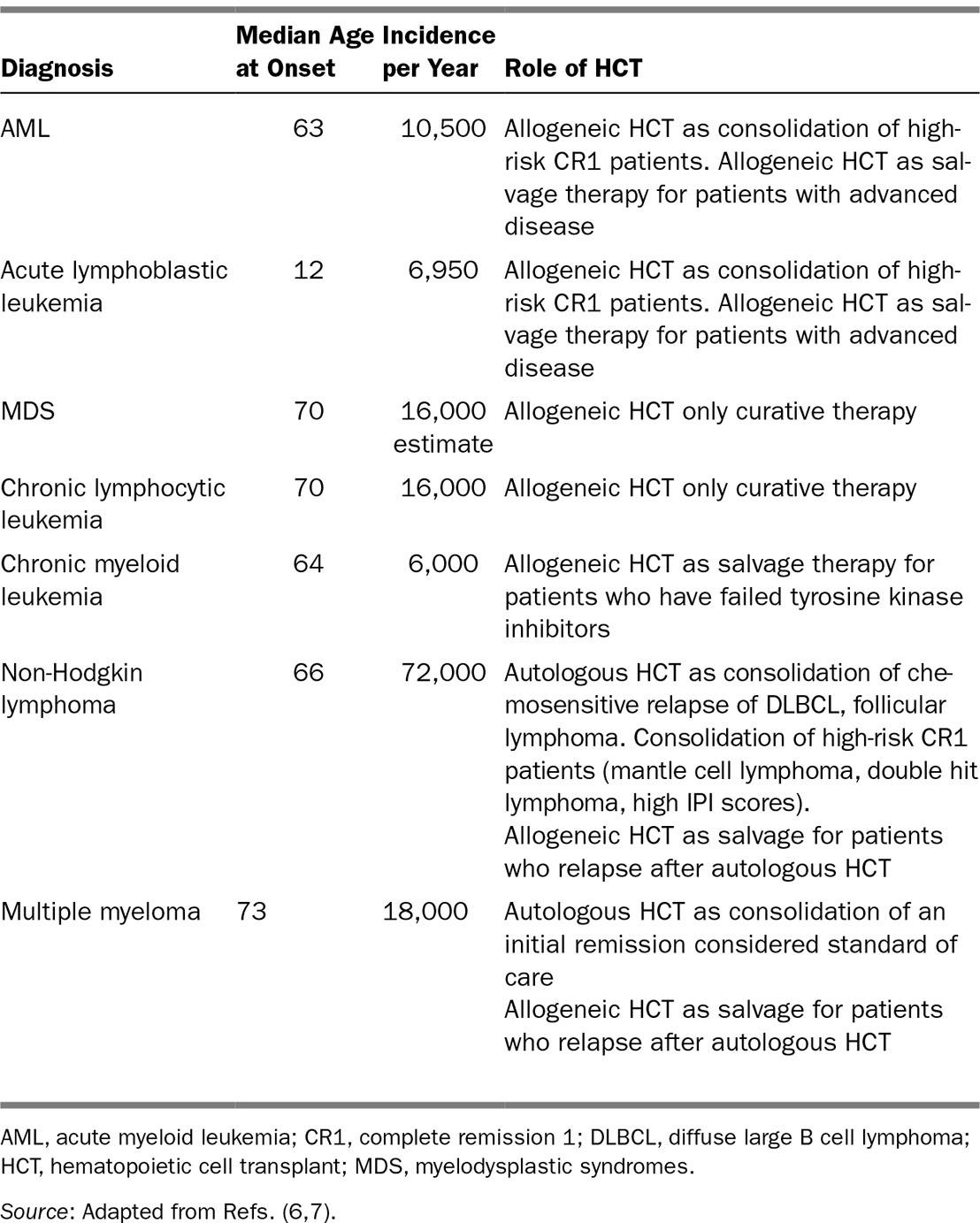
Table 25.1 summarizes the incidence and prevalence of the most common blood cancers in the United States today, as well as the median age of onset and the role of HCT in the treatment of the disease. For many blood cancers, HCT represents the only curative approach or the approach with the best chance of long-term disease control. Nevertheless, most of the patients who can benefit from this procedure are either older or medically debilitated.
TABLE 25.1 Most Common Hematologic Malignancies With Median Age of Onset, Incidence, Prevalence, and Role of Hematopoietic Cell Transplantation
244BASICS OF HEMATOPOIETIC CELL TRANSPLANTATION (8)
Hematopoietic cell transplantation is a complex procedure. The patient receives a combination of chemical and physical agents to eliminate a malignant disorder or a poorly functioning bone marrow, supported by reinfusion of hematopoietic stem cells (HSCs) from the patient or a third party (related or unrelated). As with solid organ transplantation, HCT candidates should meet a set of organ function and psychosocial criteria that may vary from transplant center to transplant center, but are aimed at determining the risk-benefit ratio of HCT versus other treatment approaches. Figure 25.2 depicts the different components and phases of the HCT procedure.
Depending on the source of stem cells, HCT can be categorized as either autologous (HSCs are obtained from patient) or allogeneic (HSCs are obtained from a third party). HSCs can be obtained from the marrow cavity or can be mobilized in large quantities into the peripheral blood using medications such as filgrastim or plerixafor and collected through apheresis techniques.
The conditioning regimen is the combination of agents given to eliminate malignant cells exploiting the dose response phenomena that most cancer cells exhibit and in the setting of HCT suppress the host immune system to allow engraftment of donor cells. Conditioning regimen intensity has been classified according to their myelosuppressive effects into myeloablative, reduced intensity, and nonmyeloablative.
Myeloablative conditioning regimens were long considered necessary for engraftment of allografts, but their considerable extramedullary toxicity typically limited their use to patients under the age of 60 years who had a good performance status and no comorbidities. RIC regimens use lower doses of busulfan, melphalan, cyclophosphamide, or Total Body Irradiation (TBI) (typically 2 Gy) often in combination with fludarabine are the ones most commonly used in older patients and in patients with comorbidities. These regimens rely more heavily on immunologic (GVL) effects to induce tumor regression and contain lower doses of drugs with cytoreductive activity. Graft-versus-host disease (GVHD) and infections remain the major causes of nonrelapse mortality (NRM).
Successful HCT requires that the patient tolerate the side effects of the conditioning regimen, so that the HSCs proliferate and mature adequately; the patient must also tolerate the treatment and prevention of infectious complications that can occur during the severely immuno compromised state of such patients during the first months after HCT. The HCT procedure can be divided into five phases:
Phase 1: Chemotherapy phase
Phase 2: Cytopenic phase
Phase 3: Early recovery phase
Phase 4: Early convalescence phase
Phase 5: Late convalescence
HCT is associated with a variety of complications that are summarized in Table 25.2.
245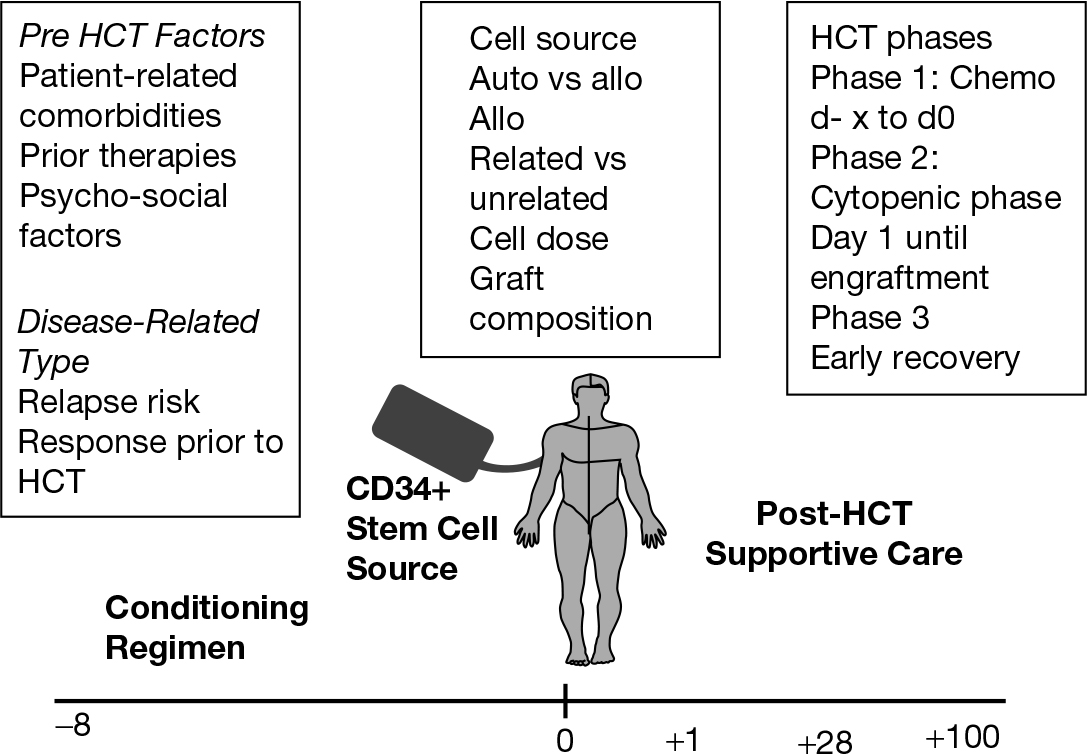
FIGURE 25.2 Components of the hematopoietic cell transplantation (HCT) procedure.
CURRENT STATUS OF HEMATOPOIETIC CELL TRANSPLANTATION IN OLDER PATIENTS
Reflecting the age distribution of different blood cancers in North America, the most common indications for HCT in patients over the age of 60 are myeloma for autografting and acute myeloid leukemia (AML) for allografting (7,9) (Table 25.3). Nevertheless, only a minority of older patients are actually undergoing HCT for a variety of hematologic malignancies that could clinically benefit them (7).
The magnitude of underutilization of HCT is probably most dramatic in myeloma, a malignant disorder of plasma cells in which randomized trials have demonstrated a significant benefit for high-dose therapy, mortality rates are extremely low, and advancing age does not significantly affect outcome (10). Costa et al. utilizing Surveillance, Epidemiology, and End Results (SEER) data and CIBMTR data demonstrated that patients over the age of 65 had less than a 25% likelihood of receiving an autologous HCT; likewise, African Americans have a 50% less likelihood of undergoing the procedure (10). Physician referral bias probably plays a role in this disparity as to who receives an allograft, as shown by the results of a survey conducted by Pidala et al., and most likely also plays a role in referrals for autografting (11,12).
The factors that influence utilization of HCT among medically fit older patients with hematologic malignancies are not well understood. El-Jawahari et al. reported on 127 patients with advanced myelodysplastic syndromes (MDSs) and examined the effects of age, gender, cytogenetics, International Prognostic Scoring System (IPSS) category, performance status, distance from HCT center, and baseline patient-reported quality of life (QOL) on the likelihood of receiving an allogeneic HCT with RIC conditioning. A total of 44 patients (35%) had undergone RIC HCT. In multivariable analyses, younger age and higher IPSS (intermediate-2/high) predicted a higher likelihood of receiving a RIC HCT (13).
246TABLE 25.2 Post–Hematopoietic Cell Transplantation Complications
Complication | Incidence | Implications for Older Patient |
Myelosuppression | Universal with exception of truly nonablative regimens | Prolonged myelosuppression increases risks of life-threatening infections; thus, strategies that may accelerate neutrophil recovery in older patients could be beneficial |
Mucositis | 50%–70% in ablative regimens 30%–50% in RIC regimens <10% in truly nonablative regimens | Severe mucositis may require opioid analgesia for pain control, which is less well-tolerated in older patients. Risk of aspiration from severe mucositis may be more frequent in older patients. One of the major benefits of RIC is reduction in the risk of severe mucositis. |
Infections | >50% of patients will have some infectious complication. Most common is neutropenic fever, gram positive sepsis, or CMV reactivation in the context of allogeneic HCT | For older patients, the ability to recover from infectious complications may be affected by prior comorbid states and ability to tolerate anti-infective therapies such as foscarnet or amphotericin B. |
Gastrointestinal toxicities | Loss of appetite almost universal Severe nausea and emesis rare with current antiemetic regimens Severe diarrhea uncommon with RIC regimens (seen more frequently with melphalan) | As with other toxicities, gastrointestinal toxicities can be more common and more severe in older patients. Essential to maintain good hydration and adequate electrolyte replacements; nutritional intervention may have to be considered earlier |
Pulmonary toxicities | Pneumonitis Diffuse alveolar hemorrhage Idiopathic pneumonia syndrome occurs in 5%–10% of patients | Patients with pre-HCT pulmonary comorbidities are at higher risk for pulmonary toxicities |
Hepatic toxicities | SOS/VOD rare with RIC, but can still occur in high-risk patients | Similar risk factors as with younger patients |
Cardiac toxicities | Arrythmias Congestive heart failure | Atrial fibrillation common occurrence after high-dose melphalan |
GVHD | Rash Diarrhea Hyperbilirubinemia Severe immunodeficiency | High-dose steroids poorly tolerated in older patients. Age a predictor of poor outcome in patients with grade 2–4 GVHD |
247Graft failure | Rare | Rare but more common with older donors |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








