Cancer of the head and neck is still a significant problem worldwide. Head and neck tumors are strongly associated with a history of smoking and alcohol consumption,1 but recent evidence has shown that low socioeconomic status is a strong risk factor, comparable to tobacco and alcohol.2 While the incidence of tobacco-related tumors appears to be decreasing, oropharyngeal (OP) cancers are increasing, primarily as a result of human papilloma virus (HPV) infection, particularly HPV-16 genotype. Recent estimates show that the incidence of HPV-related OP cancers is now greater than 50% of all OP cancers, and its incidence is increasing.3
Cancer of the head and neck can occur anywhere, but the areas most commonly involved are the skin, lip, oral cavity, oropharynx (tonsil and base of tongue), and larynx.4 Overall, roughly 50% of the tumors will be located in the oral cavity. Histologically more than 90% of all head and neck malignancies are squamous cell carcinomas, which makes them amenable to chemotherapy and radiation treatment. The standard treatment for OP and laryngeal cancers is primarily radiation and chemotherapy,5 but when this modality fails, surgery is much more difficult and frequently requires complex reconstruction. In contrast, squamous cell carcinoma of the oral cavity is more commonly treated with surgery,6 followed by radiation. In very advanced cases, chemotherapy and radiation are included.
Encompassing with the changes in the preferred treatment modalities for head and neck cancer, the management of surgical defects has changed significantly over the last decades. With the advent of improved perioperative management in the 1940s to 1950s, radical ablative surgery became the mainstay for treatment of advanced tumors, which was routinely followed by radiation therapy. Unfortunately, reconstructive surgery did not advance at the same pace, and there were no reliable reconstructive options to rehabilitate these patients. Furthermore, head and neck surgeons of the time did not consider reconstruction as an important part of the surgical treatment.7 As such, extensive surgical ablations in this era were notorious for their detrimental impact in patient’s appearance and overall function. The field of reconstruction did not show significant advances until the development of the deltopectoral flap in 1965.8 This became the workhorse for head and neck reconstruction during that period. The following decade saw the introduction of pedicled myocutaneous flaps and free flaps, which revolutionized the management of head and neck cancer patients . Up to this point, the combined therapy was still considered the mainstay of treatment, but this changed in the late 1980s with the advent of organ-preservation strategies. The combination of chemotherapy and radiation therapy is still the standard treatment for laryngeal and pharyngeal cancers, limiting surgical ablation to a salvage role.9 In this setting, salvage surgery must be performed in the context of debilitated patients, radiated fields, and decreased functional status, adding yet another layer of complexity to the planning and execution of reconstructive procedures.
Restoring form and function following oncologic surgery is a complex endeavor, regardless of the location of the defect. There are, however, specific considerations in the head and neck area that make it particularly challenging and are worth describing.
Resection of facial skin, orbital contents, or underlying facial skeleton results in deformities that are by definition conspicuous, and readily apparent. These have a detrimental impact in the patient’s self-esteem and overall social functional status.
The intricate head and neck anatomy is characterized by a close relationship between bone and soft tissue, with specific functional roles. For example, maintaining the natural separation of the nasal and oral cavities is fundamental to achieve appropriate functional results. In addition to this, there is a high concentration of neurovascular structures—such as cranial nerves and the carotid arteries—that routinely get exposed during the oncologic resection, which must be adequately protected in the reconstruction.
Speech and swallowing are complex mechanisms that rely on the synchronized interaction of afferent and efferent neuromuscular pathways. Given the epidemiology of head and neck malignancies, most oncologic resections will affect sites within the upper aerodigestive tract, such as the oral cavity or oropharynx. Surgery within these areas routinely results in loss of mucosal sensitivity, motor function (from muscle resection or denervation), and postoperative pain. All of these factors confabulate to produce significant dysphagia and dysarthria in the postoperative period.
Depending on the oncologic stage, a percentage of the patients will need postoperative radiation or chemotherapy and radiation. Exposure to radiation is a well-established factor associated with worse outcomes in reconstruction as well as worst functional outcomes.10 Even more, delay in adjuvant radiation beyond 6 weeks has been associated with worse oncologic outcomes.11 In this setting, complications from the reconstruction such as postoperative fistula could have a detrimental impact in the patient’s prognosis.
While specific goals for reconstruction vary among different sites and subsites within the head and neck, the overall goals remain relatively constant and can be schematized in order of importance. The first and most critical goal is to provide adequate coverage of deep tissues, particularly in cases where bony, vascular, or nervous structures have been exposed. This principle is maintained regardless of the location of the defect, whether it is external, sinomaxillary, or within the upper aerodigestive tract. The second goal to assure that—if indicated—the patient will be ready to start adjuvant radiation therapy in a timely fashion. It is essential that all internal and external surgical wounds are healed prior to commencing the treatment, as radiating an open wound practically assures its chronicity. The reconstructive surgeon must always bear in mind that achieving this objective is in direct relationship with the anticipated oncologic outcomes. The third goal of reconstruction is to maintain and/or restore function, which is without doubt one of the most challenging aspects of the discipline. The traditional concept of “replacing like with like” is not necessarily applicable given the highly specialized nature of some tissues, such as the tongue. Functional rehabilitation of head and neck patients will invariably rely—at least to some degree—on the acquisition of compensatory and adaptative mechanisms. In this regard, the role of reconstructive surgeon is to facilitate this process by providing an adequate anatomical framework that routinely entails restoration of the continuity of bone and soft tissue. The last goal of reconstructive surgery is to maintain the appearance of these patients. Failure to achieve an acceptable cosmetic outcome will likely result in an ostracized individual, unable to reintegrate into society.12
The head and neck has an extremely rich vascular network that can be used to the advantage of the reconstructive efforts. The common carotid arteries and internal jugular veins are encased by the carotid sheath, a thick fascial plane that separates them from adjacent structures, and are further protected by the sternocleidomastoid muscle, which covers most of their trajectory in the neck. These vessels routinely get exposed during ablative neck procedures, increasing the risk for “carotid blowout,” an abrupt and usually fatal complication of neck surgery. While the great vessels are of minimal interest in terms of sources for reconstruction, adequate coverage of these structures remains one of the critical goals of the reconstructive surgeon, particularly in the setting of radiated necks. In contrast, the internal carotid artery follows a much deeper course and is protected by the mandible and masticator musculature. As such, this vessel is rarely at risk of significant bleeding following ablative surgery.
The external carotid artery and its branches—the facial artery in particular—are of great interest to the reconstructive surgeon. The facial artery is the third branch emerging from the external carotid, commencing its course in the neck, where it gives origin to several cervical branches, the submental artery being the largest of these. This vessel supplies the mental and submental skin, which can be used as a cutaneous island flap (submental flap) for reconstruction of oral cavity defects. The facial artery travels underneath the submandibular gland to emerge over the mandibular margin, where it becomes the main blood supply for the soft tissues of the lower face. At this level, the vessel provides the axial supply for the facial artery musculomucosal (FAMM) flap, which is used for reconstruction of intraoral defects. Finally, the facial artery is routinely transected during the lymphatic node dissection of the submandibular triangle, usually over the posterior belly of the digastric muscle. The large diameter of this vessel and the fact that it is routinely exposed and transected by the ablative surgeon make the facial artery the preferred recipient vessel in patients undergoing free flap reconstruction. Other branches of the external carotid artery, such as the lingual and superior thyroid, can also be used as recipient vessels for free flaps.
In addition to the carotid arteries and their branches, the thyrocervical trunk also provides vascular supply to the neck and is of reconstructive interest. The trunk arises from the subclavian arteries and is located lateral to the carotid arteries; among others it gives origin to the transverse cervical artery (TCA). This vessel crosses the carotid triangle posterolaterally to supply the trapezius muscle, which can be used as a muscle or myocutaneous flap to reconstruct posterolateral neck defects. An important branch of the TCA is the supraclavicular artery, which arises between 3 and 5 cm from its thyrocervical trunk origin.13 This vessel penetrates the fascia in the triangle formed between the clavicle, trapezius, and sternocleidomastoid muscles, and supplies the skin of the shoulder and lateral arm. The supraclavicular flap is a recently described fasciocutaneous regional flap based on this vessel. This flap is regarded as a good alternative to free tissue transfer, given its thin and pliable nature as well as its extensive list of clinical applications.14
There are many options when considering reconstruction after ablative surgery in the head and neck. They include primary closure with and without undermining the adjacent tissue, skin grafts, local flaps, regional flaps, and free flaps. The choice will depend on the location, functional or cosmetic considerations, safety considerations, and especially the experience of the surgeon. Also tissue expanders may be useful in selected cases, although this is not usual in an oncologic reconstruction setting. Since flaps are the workhorses for head and neck reconstruction, it is important to understand the differences in their types and their clinical applications. Depending on their proximity to the defect and vascular supply, flaps can be classified as follows:
Local flaps: Using adjacent tissue is common for small defects. A safe flap in the head and neck should be around 2:1 (length to base) if using a random blood supply. If a flap is fed by a known artery, the length can be longer, even 3:1. Facial skin flaps are fairly safe because of the rich blood supply. Cervical skin flaps may have more random blood supply and are less reliable.
Regional flaps: When larger flaps are rotated from an adjacent region, they should be based on known blood supply and will be covered in the specific flap choices described later in this chapter.
Free flaps: Microvascular free flaps have replaced many of the regional flaps and are the workhorses for reconstruction of extensive or complex defects. Free flaps are based on the concept of Angiosomes, defined as the anatomical vascular territory of specific artery. The tissue and its blood supply are detached from the donor site, transferred to the head and neck area, and the vascular supply is anastomosed to recipient vessels with microvascular techniques. The most common flap options for head and neck reconstruction are covered in the section on”Flap Choices” later in this chapter.
When assessing a patient who will need reconstruction after ablative or corrective surgery, there are many considerations. If a patient has had previous radiation, this is a major factor. Healing is commonly impaired after radiation, no matter how long ago the radiation was given. Closures under tension or involving the upper aerodigestive tract will frequently dehisce after surgery in previously radiated patients. Smokers have a much greater chance for cardiopulmonary as well as wound-related complications.15 Nutrition is definitely a factor in the healing process, and it is common for patients to have poor nutrition when surgery is contemplated. Another major factor is thyroid function. After radiation to the head and neck, it is common for the patient to become hypothyroid, and if not corrected prior to surgery, healing will be poor.16 Anemia is another factor that can affect normal healing and must be corrected prior to the procedure. Age does not seem to be a major factor if the patient is healthy otherwise.
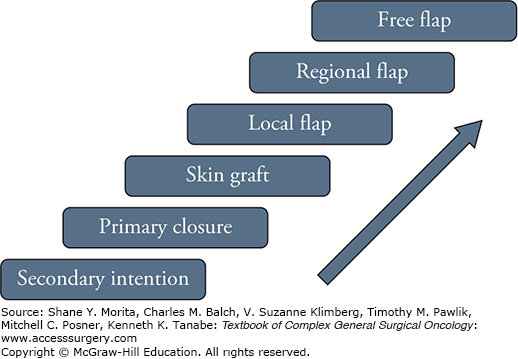
Advances in the field of reconstruction resulted in a plethora of plausible surgical alternatives for any given scenario. As a result, it might be difficult for inexperienced surgeons to decide on the best management option in each case. While there is no universally accepted management algorithm, the concept of a Reconstructive Ladder (Fig. 162-1) provides a systematic approach to the available reconstructive options. This schema organizes the surgical alternatives in an increasing order of acuity, advocating the use of the lowest acuity option that will effectively achieve the reconstructive goals. Caveats of this model include the assumption of comparable functional outcomes between techniques, and lack of consideration for important variables such as radiation therapy, or age. These limitations highlight the importance of additional considerations that must be present at the time a surgical decision is made.
The deleterious effects of radiation on the bony and soft tissues are well understood and documented, and their characterization is beyond the scope of this chapter. The possible scenarios that the reconstructive surgeon might face include prior radiation exposure and need for postoperative treatment. In patients who have been previously radiated, extreme caution must be exercised if reconstruction with local tissues is planned. The risks of flap necrosis, dehiscence, and fistula are greatly increased in this population.17 As such, it is advisable to use nonradiated tissues, such as regional or free flaps, as the first line of treatment in these patients.18 If free tissue transfer is to be performed, it is advisable to investigate if the necks were treated, as microvascular anastomosis to radiated vessels is technically more challenging and may require exploration of alternative vascular basins. In cases where radiation is expected to be given as adjuvant treatment, it is particularly important that the reconstructive process is completed ideally within 6 weeks. As such, healing by secondary intention is not advisable, and every possible effort must be made to minimize the risks for fistula and other wound-related complications. In a similar fashion, skin grafts should be avoided in this setting, given their low tolerance to radiation and tendency to present significant contracture in this setting.
This is not uncommon given the relatively high incidence of local recurrence and second primary cancers in head and neck. A detailed patient history and thorough physical examination are mandatory in this setting. This should be complemented, if possible, with a review of the previous operative reports if available. Simple reconstructions, such as primary closure or skin grafting, rarely are of significance for surgical planning in this setting. However, previous use of local, regional, or free flaps should always be taken into account. Tissues used for previous reconstructions are routinely included with the specimen, thus increasing the size and extension of the defect. As a rule of thumb, management of secondary defects requires at least the same level of complexity used initially, although it is commonly more.
The patient’s age is usually overestimated as an outcome predictor for head and neck surgery. It is well documented that it does not correlate with worse oncologic or surgical outcomes, although it is associated with increased risk of medical complications.19 The patient’s cognitive, social, and functional status are more important than his or her chronological age in the reconstructive decision-making process.
In patients undergoing any type of flap reconstruction, the characteristics of the transferred tissue and donor site morbidity profile must be taken into consideration. One of these is the presence of hair-bearing skin, which is not desirable for oral or pharyngeal reconstruction. Some flaps, such as the submental (in men) or lower extremity flaps (fibula–anterolateral thigh flap), are notorious for this characteristic. While hair does not have a significant impact on function, it is a common source of discomfort and irritation for patients. Adjuvant radiation, which is commonly given in this setting, will usually address the problem by hair follicle atrophy; laser hair removal can be used alternatively. Other flaps, such as the radial forearm, can be harvested with a minimal amount of hair-bearing skin and should be preferred for oral reconstruction.
In major head and neck reconstruction, the importance of maintaining a safe airway throughout the perioperative period cannot be stressed enough. While this may seem obvious, airway emergencies are one of the contributors for mortality in these patients. Multiple mechanisms can lead to airway compromise in these patients. Some of them are predictable, such as postoperative edema, aspiration from poor management of secretions, and airway collapse from loss of osteocartilaginous framework, while others like intraoral bleeding and spontaneous decannulation represent true emergencies. The decision of establishing a surgical airway at the time of the resection is not easy and must take into account multiple variables such as the location and extent of the defect, baseline functional status, type of reconstruction, and prior treatments. We recommend to consider a tracheotomy in cases of extensive (>50%) resections of the oral tongue, any significant OP ablation, most cases of free tissue transfer, patients with baseline aspiration (clinical or silent), and previous surgery or exposure radiation. One of the factors to keep in mind is the feasibility of oral intubation in the postoperative setting, which can be extremely challenging following reconstruction of extensive oromandibular defects.
Most local flaps are used for reconstruction of cutaneous defects, which is beyond the scope of this chapter. Regional flaps are currently reserved for the management of smaller defects, as they have been greatly replaced by free flaps. Local and regional flaps commonly used in head and neck reconstruction are described below.
This flap is based on the supratrochlear arteries and commonly used to reconstruct nasal defects or for cutaneous coverage of midline defects (refer to Fig. 161-8 in Chapter 161, “Skin Closure after Resection of Skin Malignancies, Including Melanoma”). This is a staged procedure that requires a second surgery to transect the pedicle at 4 to 6 weeks postoperatively. The donor site is usually left to heal by secondary intention, but it can also be covered with a split-thickness skin graft.
These flaps are based on the facial artery and can be superiorly or inferiorly based. These flaps are useful for reconstruction of the nose or lips and the donor site is routinely closed primarily.
This flap is based on the submental artery, which is the dominant cervical branch of the facial artery emerging immediately prior to crossing the mandible in the submandibular triangle.20 It covers a fairly large area of the submental triangle of skin, which is supplied by both submental arteries. The venous drainage must be preserved during the dissection. This flap can be used to cover defects on the lower face, the ipsilateral oral cavity, and even the palate (Fig. 162-2). When a submandibular neck dissection is performed, the blood supply can be tenuous and the potential presence of metastatic lymph nodes must be considered. The donor site for the flap can usually be closed primarily by advancing the lower neck skin.
This flap is based on the TCA and its supraclavicular branch, which provides blood supply to the skin over the shoulder and deltoid area. This flap can provide as much as 8 cm × 24 cm of thick skin for reconstruction of defects in the neck and lower face, anterior neck, or even intraoral defects. The donor site can usually be closed primarily and is inconspicuous. Preoperative use of a tissue expander can maximize the amount of available skin.
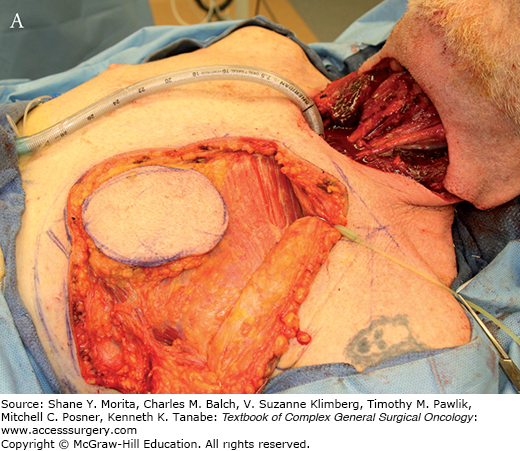
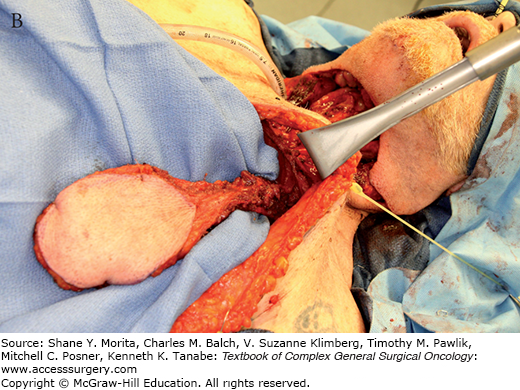
Among the regional flaps, this is the most popular option and is still widely used. While initially described for reconstruction of thoracic defects, its use for head and neck reconstruction was advocated by Ariyan21 in 1979.21 The pectoralis major muscle is supplied by the pectoral branch of the thoracoacromial artery, and partly by the lateral thoracic artery and by perforators from the internal mammary (see Fig. 159-19 in Chapter 159, “Principles of Skin Grafting and Flaps”). The primary vascular supply, the pectoral branch, comes just underneath the mid clavicle and goes inferiorly on the underside of the muscle. It is important to visualize the vessel while harvesting the flap, as the pedicle can be inadvertently transected as the dissection proceeds cephalad. It can be harvested as a myofascial or myocutaneous flap depending upon the specific reconstructive needs, and the donor site can usually be closed primarily (Fig. 162-3). This can be a bulky flap, especially in females, and is limited primarily to the neck area due to its arc of rotation. Because of its size, it is common to use a skin graft to cover part of the muscle in the neck. The cutaneous paddle portion of the flap must be planned carefully and should be over the muscle and protected from a shearing effect during harvesting. With a total loss rate of just 1% to 3%,22 this flap is characterized by its reliability and robust blood supply.
FIGURE 162-3:
A. Harvesting of a pectoralis major myocutaneous flap. The skin island is carefully preserved over the muscle. B. The flap is dissected and attached by its vascular pedicle, the pectoral branch of the thoracoacromial artery. Note the subcutaneous tunnel communicating with the neck. C. The flap is used for reconstruction of an anterior cutaneous defect.

This flap was described by Bakamjian8 in 1965 and was the workhorse for head and neck reconstruction until the late 1970s. The flap encompasses a segment of full-thickness skin and fascia over the pectoralis major muscle, but can include the skin over the deltoid (see Fig. 159-11 in Chapter 159, “Principles of Skin Grafting and Flaps”). It has a robust blood supply from the first through the fourth intercostal perforators of the internal mammary artery. Any extension beyond the deltopectoral groove has random blood supply and should not be used for any critical part of the reconstruction. The flap is primarily used to close cutaneous defects of the anterior neck and for salvage reconstruction after flap failures. The donor site can frequently be closed primarily, but a skin graft is necessary in rare cases.
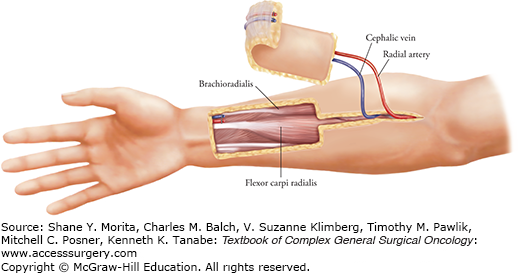
The radial forearm free flap, also known as the Chinese flap, was described by Yang et al23 in 1978 and is currently the most common free flap used for head and neck reconstruction. This flap is based on the radial artery, which supplies the skin on the volar aspect of the forearm and is located between the brachioradialis and flexor carpi radialis muscles (Fig. 162-4). The skin of the distal forearm is thin, pliable, and predominantly hairless, making it an excellent alternative for reconstruction of oral cavity and pharyngeal defects. Other advantages of this flap include its long pedicle, constant anatomy, and high tolerance to radiation. An Allen’s test should be performed in all patients preoperatively to rule out the presence of an incomplete palmar arch, an absolute contraindication to the procedure.
The palmaris longus muscle is a vestigial structure found in approximately 85% of the population. Its tendon lies superficially in the volar aspect of the forearm, and it can be easily included in the flap design as a vascularized sling, routinely used for reconstruction of total lower lip defects.24 Another modification is the osteocutaneous radial forearm flap, where a 6- to 12-cm segment of partial-thickness radial bone is harvested with the flap. In these cases, blood supply to the bone is assured through radial artery perforators reaching periosteum. While only up to 50% of the diameter of the radius can be harvested with this technique, the bone stock is usually enough for reconstruction of maxillary and mandibular defects, provided that osseointegrated implants are not being considered.25
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree