The morphology of gray zone lymphoma (GZL) is variable with tumor cells spanning the spectrum of diffuse large B-cell lymphoma (DLBCL) and classical Hodgkin lymphoma. The immunophenotype is frequently discordant. Clinically, the initial case descriptions of GZL were primarily with mediastinal presentation; however, a nonmediastinal (systemic) clinical subtype is now recognized. Patients with GZL have high relapse rates. Recommended treatment of GZL is with a DLBCL-directed regimen with consideration for consolidative radiotherapy for bulk disease. Continued biologic examination of this entity is needed and there should be exploration toward integration of novel targeted therapeutic agents into the treatment paradigm of GZL.
Key points
- •
The WHO recognizes a distinct category of B-cell lymphoma, unclassifiable, with features intermediate between diffuse large B-cell lymphoma (DLBCL) and classical Hodgkin lymphoma (cHL), also known as gray zone lymphoma (GZL).
- •
The immunophenotype of GZL is frequently discordant with tumor cells morphologically resembling DLBCL, but immunophenotypically being more consistent with cHL, and vice versa.
- •
Clinically, the initial case descriptions of GZL were primarily with mediastinal presentation; however, a nonmediastinal (systemic) clinical subtype is now fully recognized.
- •
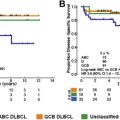
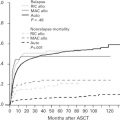
Regardless of clinical presentation, patients with GZL have relatively high relapse rates, especially compared with primary mediastinal DLBCL and cHL.
- •
Off of a clinical trial, we advocate treating GZL with a DLBCL-directed regimen (eg, R-CHOP or DA-EPOCH-R) with consideration for consolidative radiotherapy for bulk disease.
Introduction
Gray zone lymphoma (GZL) is a rare neoplasm initially described in 2005 based on the recognition of an aggressive subset of primary mediastinal B-cell lymphoma (PMBCL) with poor prognosis. GZL was officially first recognized in the World Health Organization classification as a distinct entity in 2008 as a B-cell lymphoma, unclassifiable, with features intermediate between diffuse large B-cell lymphoma (DLBCL) and classical Hodgkin lymphoma (cHL). Since this time, there has been more insight into the pathologic diagnosis, biology, and clinical outcomes for patients with GZL. Although initially clinically described as primarily involving the mediastinum, further analyses have elucidated primary mediastinal and nonmediastinal (systemic) clinical disease presentations. Notably, this article does not include discussion of the gray zone entity of lymphoma with features of intermediate DLBCL and Burkitt lymphoma.
GZL with mediastinal presentation (MGZL) is similar in presentation to cHL in part as it typically occurs in young adults in the third and fourth decade. Conversely, patients with GZL without mediastinal presentation (NMGZL) are typically older and more often present with advanced-stage disease. Furthermore, unlike cHL and PMBCL, both MGZL and NMGZL have a more aggressive clinical course with comparatively inferior outcomes. Given its newer recognition and relative paucity of associated clinical data, continued description of this unique disease entity is warranted. The following is a detailed review of the current literature and descriptions of the diagnosis, biology, prognosis, and treatment of GZL.
Introduction
Gray zone lymphoma (GZL) is a rare neoplasm initially described in 2005 based on the recognition of an aggressive subset of primary mediastinal B-cell lymphoma (PMBCL) with poor prognosis. GZL was officially first recognized in the World Health Organization classification as a distinct entity in 2008 as a B-cell lymphoma, unclassifiable, with features intermediate between diffuse large B-cell lymphoma (DLBCL) and classical Hodgkin lymphoma (cHL). Since this time, there has been more insight into the pathologic diagnosis, biology, and clinical outcomes for patients with GZL. Although initially clinically described as primarily involving the mediastinum, further analyses have elucidated primary mediastinal and nonmediastinal (systemic) clinical disease presentations. Notably, this article does not include discussion of the gray zone entity of lymphoma with features of intermediate DLBCL and Burkitt lymphoma.
GZL with mediastinal presentation (MGZL) is similar in presentation to cHL in part as it typically occurs in young adults in the third and fourth decade. Conversely, patients with GZL without mediastinal presentation (NMGZL) are typically older and more often present with advanced-stage disease. Furthermore, unlike cHL and PMBCL, both MGZL and NMGZL have a more aggressive clinical course with comparatively inferior outcomes. Given its newer recognition and relative paucity of associated clinical data, continued description of this unique disease entity is warranted. The following is a detailed review of the current literature and descriptions of the diagnosis, biology, prognosis, and treatment of GZL.
Case study
A 26-year-old Middle Eastern man was seen for second opinion of a new diagnosis of stage IIBXE cHL. On initial presentation, he experienced several weeks of nonproductive cough and drenching night sweats. A chest radiograph showed left upper lobe consolidation and he was started on antibiotics for a presumed pneumonia. His symptoms did not abate. Computerized tomography of the chest indicated multiple soft tissue masses that filled the upper mediastinum including an 11 cm × 14 cm anterior mediastinal mass with hilar adenopathy. Bronchoscopy at outside hospital with left anterior mediastinoscopy was performed. Based on morphology and positivity for CD15 and CD30, an initial diagnosis of nodular sclerosis Hodgkin lymphoma was made. The laboratory data were notable for a mild anemia, with hemoglobin 12 g/dL and hematocrit of 36% without further abnormalities. There was no evidence of bone marrow involvement on staging biopsy.
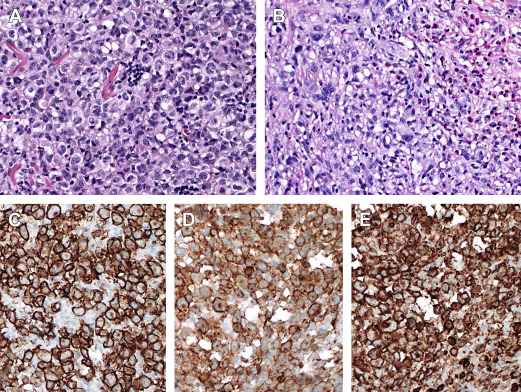
Additional pathologic review conducted at our institution and the National Institutes of Health (NIH) noted unusual morphology and immunophenotype. In addition to areas of cHL, the tumor exhibited extensive syncytial sheets of large cells, Reed-Sternberg cells, and variants. The neoplastic cells showed strong positivity for CD20 and CD15 with strong to variable positivity for CD30 ( Fig. 1 ). The final diagnosis was B-cell lymphoma, unclassifiable, with features intermediate between DLBCL and cHL (ie, GZL). The patient was treated with cyclophosphamide, doxorubicin, oncovin, and prednisone and rituximab (CHOP-R) for six cycles. The patient had a Deauville score of 3 after two cycles and was Deauville score 2 at end of chemotherapy; he subsequently received mediastinal involved-node radiation therapy (3000 cGy). The patient currently remains disease-free 34 months following initial diagnosis.
Biology
GZL is known to arise from an altered B cell. In GZL, the putative cell of origin is thymic B cell, which is also a common precursor for cHL and PMBCL. This common precursor hypothesis explains why cHL, PMBCL, or GZL may relapse as the other related entity and why they are found as synchronous neoplasms. The notion of a common cell of origin is supported by data examining gene expression signatures of GZL, PMBCL, and cHL being similar as were numerous genetic abnormalities, such as gains in chromosome 9p and 2p. However, because GZL may differentiate in either direction (eg, Reed-Sternberg cell/variant or DLBCL), epigenetic changes as opposed to genetic aberrations may more strongly influence the final morphology and immunophenotype.
Eberle and colleagues performed a DNA methylation analyses of 30 cases including cHL, PMBCL, and GZL. They demonstrated a close relationship between the three diseases but with unique signatures that distinguished GZL from HL and PMBCL. These included lack of de novo hypomethylation in cHL, hypomethylation of HOXA5 in GZL, and hypermethylation of EPHA7 and DAPK1 in PMBCL. In addition, the nuclear factor-κB pathway was highly enriched and was important to the pathogenesis of all three disease entities. Notably, most of the aforementioned biologic studies have been conducted among patients with MGZL; it is not known if NMGZL has similar or distinct biology.
Diagnosis
The diagnosis of GZL should be made by expert pathologic evaluation of the involved tissue preferably obtained by an excisional or incisional biopsy. GZL is highly variable with each tumor displaying a unique set of features. A spectrum of morphologies known with cHL and DLBCL can occur and divergent morphologic areas are seen within the same tumor necessitating extensive sampling for the correct diagnosis. The neoplastic cells are usually large with centroblastic or immunoblastic appearance, high degree of pleomorphism, and can include bona fide Reed-Sternberg cells and variants. Mummified cells can be present. In cases resembling PMBCL the neoplastic cells occur in sheets. In cases resembling cHL the neoplastic cells are sparse and occur on mixed inflammatory background with small lymphocytes, histiocytes, and eosinophils. These cases can exhibit significant degree of fibrosis and distinction from true cHL is difficult. Necrosis can be present and be extensive. Neutrophilic infiltrates, however, are not a usual feature.
Similar to morphologic findings, the immunophenotype of GZL is variable and has transitional features between cHL and DLBCL ( Table 1 ). Tumors resembling cHL can show prominent CD20, weaker/absent CD30, and absent CD15, whereas tumors resembling DLBCL may be strongly positive for CD30 and CD15 with negative CD20 and CD79a. Because the B-cell program is preserved, B-cell transcription factors, such as PAX5, OCT2, and BOB1, are positive in neoplastic cells. In comparison with a cohort of 51 patients with PMBCL, patients with MGZL were more often male, expressed CD15, and had lower expression of CD20.
| Feature | PMLBCL | DLBCL | cHL | GZL |
|---|---|---|---|---|
| Morphology | ||||
| RS cells and variants | Rare | Rare | Yes | Yes in areas |
| HL background | No | No | Yes | Yes in areas |
| Sheets of large cells | Yes | Yes | Syncytial variant | Yes in areas |
| Fibrous bands | No | No | Yes | Uncommon |
| “Alveolar” fibrosis | Yes | No | No | Sometimes |
| Necrosis | Yes | Yes | Common | Common |
| Neutrophilic infiltrates | No | No | Yes | No |
| Immunophenotype | ||||
| CD20 | + | + | −/+ | −/+ or + |
| CD30 | + weak, variable | −/+ | + | + or +/− |
| CD15 | −/+ | − | +/− | +/− |
| CD79a | + | + | −/+ | −/+ or + |
| PAX5 | + | + | + (weak) | −/+ or + |
| Bcl6 | +/− | +/− | +/− (weak) | +/− variable |
| OCT2 | + | + | −/+ | +/− or + |
| MUM1/IRF4 | +/− | + ABC type | + | + |
| CD45 | + | + | − | +/− or + |
| EBV (EBER) | − | −/+ | −/+ | −/+ |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree