Granulomatous Infection
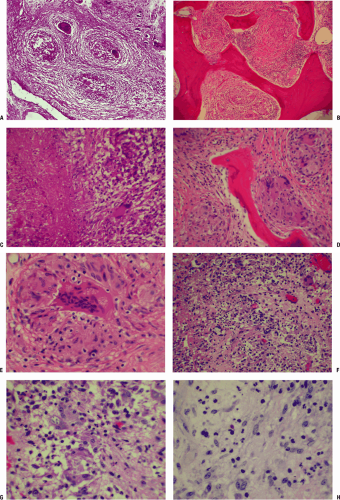
Granuloma is defined as a microscopic-sized aggregation of histiocytes and hypertrophied fibroblasts termed epithelioid cells, centrally located and rimmed by a chronic inflammatory infiltrate of lymphocytes and plasma cells (Fig. 27.2-1). The entire focus can be surrounded by a ring of fibrosis. Multinucleated giant cells, with a characteristic positioning of the nuclei at the periphery of the cell (foreign body or Langhans giant cells), are frequently present (Table 27.2-1). Over time the granuloma may be replaced by scarring and even calcification. In tuberculosis, the central area may undergo caseous (cheese-like) necrosis.
Conditions associated with granulomatous histology (see Fig. 27.2-1) include:
Infection by mycobacteria, fungi, or parasites
Foreign materials
Eosinophilic granuloma
Sarcoidosis
The response in bone is indolent, with slowly enlarging lytic defects in bone with smooth walls accommodating confluent, usually caseating granulomas.
Eosinophilic granuloma (Langerhans cell histiocytosis or Langerhans cell granulomatosis) only infrequently has clear-cut granulomatous histology (see Table 27.2-1). This disorder can progress with rapid local osteolysis (unique among granulomatous bone processes, which are usually indolent).
Mycobacterial Osteomyelitis
Tuberculosis (TB) will be discussed in detail as the prototype disorder in this section.
Pathophysiology
General
Tubercle bacillus induces an acute inflammatory response on entry into host tissue that usually controls the infection, walling it off to form a primary complex; if infecting dose overwhelms the response, the infection persists and spreads; during the early stages, bacilli may move into the circulation and metastasize to central nervous system, bones, or liver.
PMNs, on ingesting the bacilli, may necrose and become engulfed by macrophages and mononuclear cells.
Macrophages adopt epithelioid morphology on accepting the lipids of the bacilli, or may aggregate to form Langhans giant cells, whose task is to digest and remove the bacilli; these cells may also be overcome by the bacillus, also necrosing and inducing further phagocytic activity. Necrosis of epithelioid and Langhans cells becomes confluent (caseating).
After 1 week, lymphocytes form a ring around the periphery of the lesion, forming a 1- to 2-mm nodule known as the tubercle.
During the second week caseation starts to occur, induced by the protein fraction of the tubercle bacilli.
Over time, the PMN response is replaced by chronic inflammatory round cell infiltration accompanied by a fibroblastic proliferation that is variable in degree around the tubercle (chronic inflammatory focus).
This immune response usually will control the infection, in essence walling it off, where it can lie dormant for a lifetime, potentially becoming active as old age and impaired immune response occur.
Musculoskeletal lesions form by metastasis from 3 months to 3 years after the primary infection.
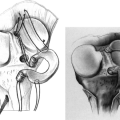
Spine
Children: Spine involvement begins in the vertebral body, usually anteriorly, then extends to adjacent disc and vertebral body.
Adults: Onset is beneath the periosteum under the anterior longitudinal ligament and may spread up and down the spine, bypassing some vertebrae to lodge at more than one level; disc space narrowing, vertebral body destruction, collapse with kyphosis, and eventual fusion may occur after 1 to 2 years.
Extraspinal
Unlike bacteria, TB does not produce proteolytic enzymes that aggressively destroy cartilage, affording more time to make the diagnosis before the joint is destroyed in tuberculous arthritis.
Bacillus lodges in synovium and proliferates, opposed by the immune process in sequence as outlined above.
The inflamed synovium enlarges to fill all recesses
of the joint, spreading over the cartilage from the periphery as a pannus, mechanically eliminating nutrition of the cartilage from the surface.
Table 27.2-1 Langhans Versus Langerhans Cells
Langhans Cells
Langerhans Cells
Appearance
Giant cells with nuclei distributed around the periphery
Histiocytes with typical coffee-bean cleaved nuclei (NOT giant cells)
Associated conditions
Tuberculosis, foreign body granulomas
Langerhans cell histiocytosis or Langerhans cell granulomatosis or eosinophilic granuloma (older terminology)
Central joint space is preserved for months.
Cold abscess
A marked exudative reaction consists of serum, PMNs, caseous material, bone debris, and tubercle bacilli.
This collection migrates under the influence of gravity and may present along the spine and pelvis, in the groins, or about involved joints.
It may present through the skin as a sinus or ulcer, which may then become secondarily infected, obscuring the diagnostic picture.
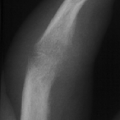
Regional osteopenia
The inflammatory process induces an active hyperemia with osteoclastic deletion of bone, resulting in marked regional osteopenia.
Kissing sequestrate
The inflammatory synovial mass invades weakened subchondral bone from the periphery.
Rarely, sequestration of the opposing joint surfaces can occur as a result of this bone destruction, leading to the radiographic picture of “kissing sequestrate.”
Etiology
Causative organisms include Mycobacterium tuberculosis (TB), Mycobacterium leprae, and environmental mycobacteria.
Organisms grow on enriched medium slowly so that colonies appear at 2 to 4 weeks.
Acid-fast stain may reveal classic “red snappers.”
Epidemiology
One third of global population is infected with TB; most frequent cause of death and disability worldwide.
U.S. statistics
10 million are infected; 90% of new activated cases come from this pool.
In non-Hispanic whites, median age at diagnosis is 61; among minority groups it is 39.
Americans >65 represent 6.5% of population but account for 26% of reported cases.
20% of new cases of TB have extrapulmonary disease.
33% of patients with TB and HIV have extrapulmonary disease.
1% to 3% of patients with TB develop musculoskeletal manifestations.
Diagnosis
Clinical Presentation
Classic: Patient becomes insidiously ill and develops chronic local musculoskeletal pain, fever, and weight loss.
Initial presentation may include:
Cold abscess: juxta-articular or paraspinal soft tissue mass without inflammation
Spinal involvement: may be truncal rigidity, muscle spasm, and neurological signs and deficit; spinal deformity (gibbus) is a late finding
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree