GENERAL THERAPEUTIC PRINCIPLES OF SURGERY AND IRRADIATION
The management of pituitary tumors commences with a careful definition of the location and extent of the lesion and the endocrinologic abnormalities. The principles of therapy are based primarily on these factors and their clinical sequelae. Any direct effect of the mass (e.g., vision impairment) must be addressed, and any endocrinologic dysfunction must be corrected. Certain hormonal deficiencies, particularly those of cortisol or thyroid hormone, should be corrected immediately. Possible complications of therapy, most prominently hypopituitarism or tumor recurrence, can occur many years (up to 30 years) after therapy and must be carefully considered.
The choice of treatment modality is determined by several factors: (a) the need for immediate relief of a mass effect, (b) the need to relieve an endocrine abnormality, (c) the potential for obtaining long-term control, and (d) the character and frequency of possible associated morbidity.
Surgery and radiotherapy are the two main available tools for radical treatment of all types of pituitary adenomas. Their common technical characteristics and side effects are presented in this section. More specific medical modalities, applicable to certain types of pituitary tumors, are detailed in the later section, which deals with therapeutic options according to the type of pituitary adenoma.
SURGERY
The purpose of surgery in the management of pituitary adenomas includes, according to the circumstances, the histologic confirmation of the diagnosis; the correction of tumor-mass effect; the complete excision of a microadenoma and, if possible, of a macroadenoma; and the reduction of the tumor bulk of an invasive adenoma. Whatever the immunocytochemical type, the greater the extent to which an adenoma is small, is enclosed, and is noninvasive, the better are the results of surgical removal. In most cases, either a transsphenoidal or a subfrontal transcranial approach is used7,8 and 9 (see Chap. 23).
TRANSSPHENOIDAL TECHNIQUE
The transsphenoidal approach, via a sublabial incision, is now preferred by most pituitary neurosurgeons for the vast majority (>95%) of patients with pituitary tumors. This technique allows entry into the facial portion of the sphenoid sinus, through which access is gained to the pituitary fossa. Binocular surgical microscopy is coupled with fluoroscopic monitoring to obtain direct visualization of the surgical field. The transsphenoidal approach offers the capability of tumor destruction by resec tion, by coagulation, or by freezing. This technique is indicated for removal of a tumor that is confined to the sella turcica, removal of a tumor associated with cerebrospinal fluid (CSF) rhinorrhea or of a pituitary apoplexy, removal of a tumor with sphenoidal extension, removal of a tumor with only modest suprasellar extension, or removal of a tumor which has fluid
characteristics that allow the suprasellar part of the adenoma to flow down by gravity into the sellar cavity.
characteristics that allow the suprasellar part of the adenoma to flow down by gravity into the sellar cavity.
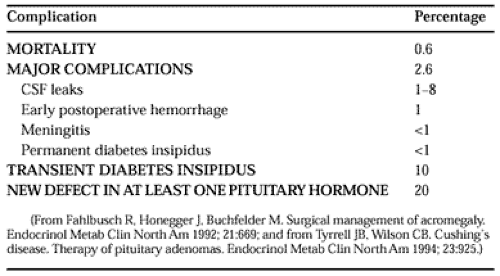
Contraindications to use of the transsphenoidal approach include the presence of dumbbell-shaped tumors with constriction at the diaphragma sellae, massive suprasellar tumors, lateral suprasellar extension of a tumor, and an incompletely pneumatized sphenoid bone. Morbidities include transient diabetes insipidus and, rarely, meningitis or persistent CSF rhinorrhea (Table 24-1). When a selective resection of an adenoma is possible, subsequent hypopituitarism is uncommon.
SUBFRONTAL APPROACH
The subfrontal approach, via craniotomy, is limited to surgery for dumbbell-shaped lesions for which removal by a transsphenoidal approach is impossible; for tumors with suprasellar extension involving the chiasm; or for tumors involving the surrounding vascular structures. The disadvantages of the subfrontal approach include a high morbidity (increased duration of hospitalization, seizures, memory loss), and increased mortality resulting from damage to vital structures. Furthermore, a substantial incidence of postoperative hypopituitarism and diabetes insipidus is seen.
COMBINED TRANSSPHENOIDAL AND SUBFRONTAL APPROACHES
When combined transsphenoidal and subfrontal approaches are used, due to the lower risk of side effects and complications with the transsphenoidal operation as compared with the subfrontal approach, transsphenoidal surgery may be used as the primary surgery, and the removal of a tumor remnant may be performed, when necessary, by a subsequent subfrontal route.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree