Summary of Key Points
- •
Epidemiology of lung cancer is still changing: in the last 10 years lung cancer became the first cause of cancer-related deaths in both men and women in many countries, while having previously been a rare disease in females.
- •
Smoking is the first cause of lung cancer also among women: no conclusive data are present in the literature about female smokers and their susceptibility to develop lung cancer, compared with their male counterparts.
- •
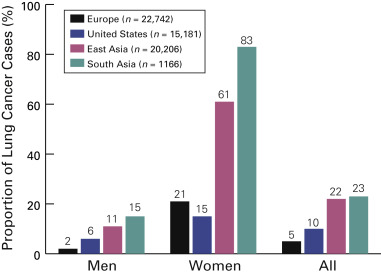
The risk of lung cancer is 2.5 times more common in female lifetime nonsmokers compared with male nonsmokers with different geographic distribution: in Asia the proportion of female lung cancer patients who are never-smokers ranges from 61% to 83%.
- •
Several publications describe a more favorable prognosis of lung cancer in women than in men, and this is regardless of a longer life expectancy or the influence of other factors.
- •
Population studies and preclinical studies suggest that steroid hormone pathways, as well as progesterone receptors, are involved in the biology of lung cancer: these pathways are consequently promising targets for lung cancer therapy.
- •
From a molecular biology point of view, lung cancer in women should be considered a specific entity, and this fact must be taken into account in diagnosis and therapeutic approaches.
For several decades, lung cancer has been considered a neoplastic disease affecting mainly men; however, during the past 40 years, the incidence of the disease has increased exponentially among women. From 1990 through 1995, in many Western countries, the incidence of lung cancer among men has gradually declined as a result of antitobacco campaigns, which, in turn, led to a progressive reduction in incidence rates for men and women, with a projection of equal incidences by 2020.
The mortality rate for lung cancer among women shows a clear inverse trend compared with most other cancers. Whereas deaths from gastric and uterine cancer have plummeted in the past four decades and deaths from breast cancer have steadily declined since a peak in 1990, deaths from lung cancer have continued an upward trajectory, reflecting the consequences of tobacco smoking among women. Overall, lung cancer causes death for more women than the combination of the three most common cancers among women (breast, colorectal, and ovarian cancer).
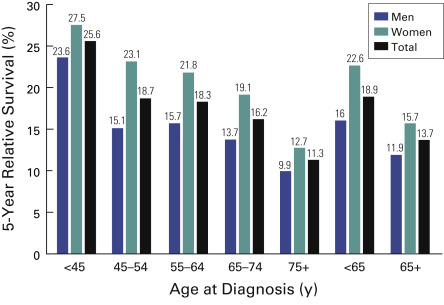
Whether women are more or less susceptible than men to the carcinogenic effects of cigarette smoking is controversial. Compared with men, women are less likely to have a smoking history and are more likely to be younger at the time of diagnosis and to have a better survival at any stage ( Fig. 5.1 ). Adenocarcinoma of the lung is the most common histologic subtype among women.
Epidemiology
Worldwide, lung cancer accounts for the most cancer diagnoses (1,600,000 new cases; 12.4% of total new cancer cases) and is the leading cause of cancer-related deaths in both men and women (1,378,000 deaths; 17.6% of total cancer deaths). The estimated number of lung cancer cases worldwide has increased by 51% since 1985 (a 44% increase in men and a 76% increase in women).
The World Health Organization (WHO) estimates that worldwide lung cancer deaths will continue to increase, largely as a consequence of an increase in global tobacco use, primarily in Asia. Despite efforts to curb tobacco smoking, there are approximately 1.1 billion smokers around the world, and if the current trends continue, that number will increase to 1.9 billion by 2025.
United States
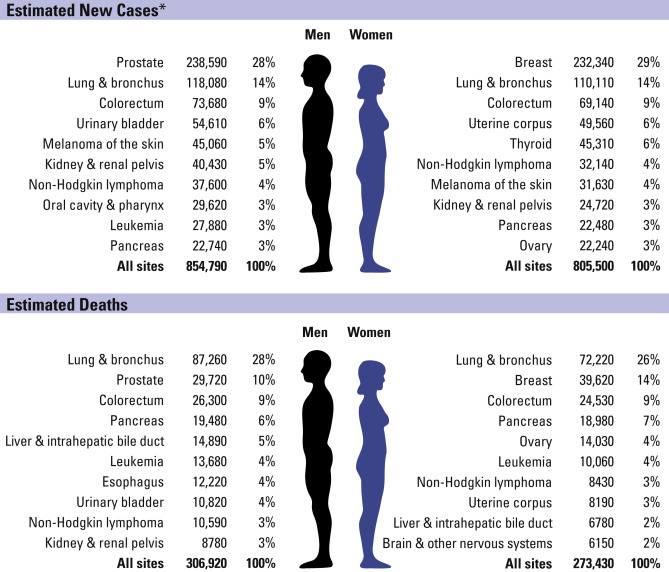
In the United States, it is estimated that 118,080 men and 110,110 women were diagnosed with lung cancer in 2013, and 87,260 men and 72,220 women died of the disease. The age-adjusted death rate for the period from 2006 to 2010 was 63.5/100,000 and 39.2/100,000 for men and women per year, respectively.
The most common cancers expected to occur in men in 2013 included prostate, lung and bronchus, and colorectal, which account for about 50% of all newly diagnosed cancers (prostate cancer alone accounted for 28%, or 238,590 of all new cases). In women, the three most commonly diagnosed types of cancer in 2013 were breast, lung and bronchus, and colorectal, accounting for 52% of estimated cancer cases (breast cancer alone accounted for 29%, or 232,340 of all new cases). These cancers continue to be the most common causes of cancer death ( Fig. 5.2 ). In 2013, lung cancer was expected to account for 26% of all cancer-related deaths among women and 28% of all cancer-related deaths among men. Of the 2,437,163 deaths recorded in the United States in 2009, 567,628 were caused by cancer. Lung cancer is the leading cause of death among men aged 40 years and older and is the leading cause of cancer-related deaths among women aged 60 years and older.
The Hispanic/Latino population is the largest and fastest growing major demographic group in the United States, accounting for 16.3% (50.5 million/310 million) of the US population in 2010. In 2012, an estimated 112,800 new cases of cancer were diagnosed and 33,200 cancer-related deaths occurred among Hispanic individuals. The incidence and mortality rates for all cancers combined and for the four most common cancers (breast, prostate, lung and bronchus, and colorectal) are lower for the Hispanic population than for the non-Hispanic white population, but the incidence and mortality rates are higher for cancers of the stomach, liver, uterine cervix, and gallbladder. These differences in rates reflect greater exposure to cancer-related infectious agents, lower rates of screening for cervical cancer, differences in lifestyle and dietary patterns, and possibly genetic factors.
The considerable efforts in implementing tobacco-control strategies in the United States since the 1950s and the subsequent favorable changes in smoking behaviors in 1975 to 2000 have averted more than 240,000 lung cancer-related deaths in women. However, it is estimated that 20.6% of all American adults 18 years and older continue to smoke, a percentage that has changed slightly since approximately 1997. Smoking prevalence in the United States has decreased from a high of 53% for men and 32% for women in 1964 to rates of 21.6% for men and 16.5% for women in 2011.
Large geographic differences in public policies against tobacco use and socioeconomic factors affect the distribution of lung cancer mortality rates across states. California has been a leader in introducing public policies designed to reduce cigarette smoking. It was the first state to establish a comprehensive state-wide tobacco-control program in 1988 through increased excise taxes on cigarettes, and as early as the mid-1970s it had local government ordinances for smoke-free work places. As a result, progress in reducing smoking prevalence and mortality associated with smoking-related diseases, including lung cancer, has been much greater in California than in the rest of the United States. Jemal et al. evaluated state-specific lung cancer mortality rates among white women to assess regional differences in lung cancer trends. The decrease in age-specific lung cancer mortality rates among white women continued in younger age groups and birth cohorts in California, but the decline was slower or even reversed among women younger than 50 years of age and for women born after the 1950s in the remaining 22 states analyzed, especially in the South and Midwest.
Europe
Worldwide, the estimated incidence of lung cancer among women is 516,000, of which 100,000 are diagnosed in the United States and 70,000 in Europe. There are still differences when incidence rates from European cancer registries are compared with rates in the United States, suggesting that the lung cancer epidemic among women in Europe may not yet have reached the US rate from the 1990s (>25 lung cancers/100,000 women). Nevertheless, in the European Union (EU), the lung cancer mortality rate for women increased by 50% between the mid-1960s and the early 2000s and steady upward trends have been seen even in the youngest age groups in some southern European countries such as France and Spain up to the early 2000s.
In the EU, lung cancer mortality rates for women increased during the past decade, from 11.3/100,000 to 12.7/100,000 (2.3% per year) for all ages (a further increase is predicted to reach 14/100,000 women in 2015) and from 18.6/100,000 to 21.5/100,000 (3.0% per year) for middle-age women ( Fig. 5.3 ).
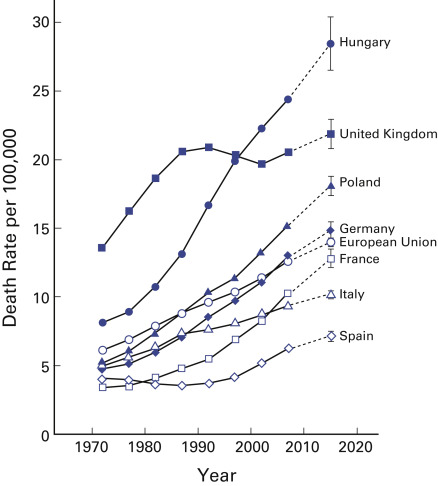
Despite the reduction in breast cancer mortality, this disease is still the leading cause of cancer-related deaths among women across the EU, as well as specifically in France, Germany, Italy, and Spain. Lung cancer is the leading cause of cancer-related deaths in several countries in Northern and Eastern Europe, including Denmark, Hungary, the Netherlands, Poland, Sweden, and the United Kingdom. The projected cancer mortality rate has increased among women in several European countries. In Serbia, colorectal cancer in men and lung cancer in women are estimated to have the most significant increase over time (2010 to 2014): 0.42/100,000 ( p = 0.036) and 0.626/100,000 ( p < 0.001) per year, respectively. From 1996 to 2001, the National Health Service Breast Screening Programme in the United Kingdom recruited 1.3 million women into the Million Women Study. The women signed consent forms and completed a questionnaire about lifestyle, medical history, and sociodemographic factors and were resurveyed by mail about 3 years and 8 years later. Twenty-three of the 30 most common causes of death occurred more frequently in smokers; the rate ratio for lung cancer was 21.4 (19.7–23.2). The increased mortality among smokers compared with never-smokers was mainly from diseases such as lung cancer that can be attributed to tobacco smoking. Among former smokers who stopped smoking permanently between the ages of 25 years and 34 years or between the ages of 35 years and 44 years, the respective relative risks were 1.05 (95% CI, 1.00–1.11) and 1.20 (95% CI, 1.14–1.26) for all-cause mortality and 1.84 (95% CI, 1.45–2.34) and 3.34 (95% CI, 2.76–4.03) for lung cancer–specific mortality.
In the EU in 2012, nearly 88,000 women died from breast cancer, corresponding to almost 16% of all cancer deaths among women. The projected lung cancer-related deaths for 2015 are 187,000 for men and 85,204 for women. In a pooled analysis of 13,169 lung cancer cases and 16,010 controls from Europe and Canada, the most common histologic subtype was squamous cell carcinoma among men (4747 of 8891; 53.4%) and adenocarcinoma among women (1013 of 2017; 50.2%). No clear-cut evidence for gender preference was found among the major subtypes of small cell lung cancer (SCLC): 19.8% in men and 21.9% in women. Never-smoking status was reported for 220 (2.1%) men and 609 (24.2%) women; the most common subtype was adenocarcinoma (57.6% in men and 70.1% in women).
Similar to US data, an epidemiologic study conducted in Poland showed that a higher proportion of women (23%) were diagnosed with lung cancer at a younger age (less than 50 years) compared with men (12%).
Asia
In Asia, the lung cancer mortality rates for women are lower than in the United States and Europe. However, these rates are increasing across several Asian countries, including China, South Korea, and Japan. Adenocarcinoma tends to be the most common histologic type in women in Asia, and this proportion continues to increase over time. Although tobacco smoke is the most common cause of lung cancer in women throughout the rest of the world, the cause of lung cancer in Asian woman is considered more complex ( Fig. 5.4 ). The proportion of women with lung cancer who are never-smokers ranges from 61% to 83%. In fact, the smoking rate is higher than 10% only for Filipino and Japanese women. Environmental tobacco smoke and indoor pollutants, including cooking oil fumes and burning coal, have been implicated in increasing the risk of lung cancer among nonsmoking Asian women.
In China, cancer incidence and mortality data for 2009, including demographic information from 104 population-based cancer registries, were reported to the National Central Cancer Registry, a government organization for cancer surveillance. After an evaluation procedure, data from 72 registries were deemed satisfactory and were then compiled for analysis. According to these data, lung cancer was the most common cancer in China overall and in its urban areas and the second most common cancer in its rural areas. There were 197,833 new cancer cases and 122,136 deaths. The crude cancer mortality was 184.67/100,000 overall, 228.14/100,000 for men and 140.48/100,000 for women. These findings indicate that lung cancer was the most common cancer for men in all areas, particularly urban areas, and second to breast cancer in women, especially in urban areas. Lung cancer was the leading cause of cancer-related deaths in all groups stratified by gender and area. Ages over 50 years were the high-risk age groups because of the increase in incidence and mortality rates that accompany increasing age.
In India, over a 2-year period, 130 trained physicians independently assigned causes to 122,429 deaths in 6671 randomly selected small areas from the 1991 census and monitored all births and deaths in 1.1 million homes representative of all of India. Among people 30 years to 69 years old, the three most common fatal cancers among men were oral (including lip and pharynx, 45,800 [22.9%]), gastric (25,200 [12.6%]), and lung (including trachea and larynx, 22,900 [11.4%]); among women, the three most common fatal cancers were cervical (33,400 [17.1%]), gastric (27,500 [14.1%]), and breast (19,900) [10.2%]). Tobacco-related cancers represented 42.0% (84,000) and 18.3% (35,700) of cancer-related deaths among men and women, respectively, and there were twice as many deaths caused by oral cancers compared with lung cancers.
Data from the Korean National Cancer Incidence Database on 599,288 adult patients diagnosed with solid cancers between 2005 and 2009 were analyzed to identify possible gender differences. For all solid cancer sites combined, the risk of death for women was 11% lower than that for men (relative excess risk 0.89; 95% CI, 0.88–0.90) after adjusting for year of follow-up, age, stage, and case mix. The relative excess risks for cancer of the lung, head/neck, esophagus, small intestine, liver, nasal cavities, bone/cartilage, soft tissue, brain and central nervous system, and thyroid and melanoma were significantly lower for women.
Susceptibility
Never-Smokers
Never-smokers with lung cancer represent a unique subset of all people with lung cancer. Globally, an estimated 15% of lung cancer cases in men and 53% of cases in women are not attributable to tobacco smoking. The risk of lung cancer is 2.5 times more common among female lifetime nonsmokers than among male lifetime nonsmokers. One of the most relevant risk factors for nonsmoking women is environmental tobacco smoke exposure. A meta-analysis of 55 studies of spousal smoking on the risk of lung cancer for a nonsmoking spouse showed a pooled relative risk of 1.27 (95% CI, 1.17–1.37), with risk increasing monotonically with increasing exposure. This association has been replicated in different populations across Asia, Europe, and North America.
Nevertheless, there remains a large fraction of lung cancers among never-smokers that cannot be definitively associated with established environmental risk factors, and limited data are available on the epidemiologic risk factors for lung cancer in never-smokers according to gender. Although smoking prevalence has decreased, the incidence of lung cancer has increased steadily in Taiwan over the past several decades; only 9% to 10% of women with lung cancer and 79% to 86% of men with lung cancer are tobacco smokers. In a matched case–control study conducted between 2002 and 2009, several epidemiologic factors of lung cancer in never-smokers differed between men and women. The risk for lung cancer was higher for people exposed to environmental tobacco smoke (odds ratio, 1.39; 95% CI, 1.17–1.67) with a history of pulmonary tuberculosis and with a family history of lung cancer in first-degree relatives (odds ratio, 2.44); people with a history of hormone-replacement therapy and who used fume extractors when cooking were protected. For men, only a family history of lung cancer in first-degree relatives was significantly associated with risk of lung cancer (odds ratio, 2.77).
A case–control study in China included 399 lung cancer cases and 466 controls, of which 164 cases and 218 controls were female nonsmokers. Among nonsmoking women, lung cancer was strongly associated with multiple sources of indoor air pollution, including heavy exposure to environmental tobacco smoke at work (adjusted odds ratio, 3.65), high frequency of cooking (adjusted odds ratio, 3.30), and use of solid fuel for cooking (adjusted odds ratio, 4.08) and heating (adjusted odds ratio for coal stove, 2.00). In addition, housing characteristics related to poor ventilation, including single story homes, less window area, absence of a separate kitchen, lack of a ventilator, and limited time with windows open, were associated with lung cancer.
Smokers
A prospective evaluation of 50-year trends in smoking-related mortality in the United States demonstrated that the relative and absolute risks of death from smoking continue to increase among female smokers. The relative risks of death from lung cancer, chronic obstructive pulmonary disease (COPD), ischemic heart disease, any type of stroke, and all causes are now nearly identical for female and male smokers. The risk of death from lung cancer among male smokers appears to have stabilized since the 1980s, whereas it continues to increase among female smokers. For women aged 60 years to 74 years old, the all-cause mortality rate is now at least three times as high among current smokers as among never-smokers.
Currently, no conclusive data are available on the susceptibility of lung cancer among female smokers. Some studies have shown a greater risk of lung cancer for female smokers than for male smokers. Data generated by the American Health Foundation database indicate that the odds ratio for the major lung cancer types is consistently higher for women than for men at every level of exposure to cigarette smoke. The dose–response odds ratios for lung cancer among women are 1.2-fold to 1.7-fold higher than among men. A Canadian case–control study of gender differences in lung cancer from 1981 to 1985 showed that with a 40-pack-year smoking history (compared with lifelong nonsmokers), the odds ratio for the development of lung cancer was 27.9 for women and 9.6 for men. In both of these studies, the increase in lung cancer risk held for all major histologic types. In a pooled analysis that included 13,169 cases and 16,010 controls from Europe and Canada, the odds ratio for different histologies of lung cancer was assessed. For male current smokers (average of 30 cigarettes per day), the odds ratios were 103.5 (95% CI, 74.8–143.2) for squamous carcinoma, 111.3 (95% CI, 69.8–177.5) for SCLC, and 21.9 (95% CI, 16.6–29.0) for adenocarcinoma. For female current smokers, the corresponding odds ratios were 62.7 (95% CI, 31.5–124.6), 108.6 (95% CI, 50.7–232.8), and 16.8 (95% CI, 9.2–30.6).
Other studies have shown comparable risks for men and women when controlling for smoking exposure. A gender-smoking interaction in association with lung cancer risk within a population-based case–control study (Lombardy, Italy, 2002–2005) was evaluated in 2100 cases with incident lung cancer and 2120 controls. Lung cancer odds ratios for pack-years (categorical) were higher for men than women, with a negative gender-smoking interaction for women ( p = 0.0009). For medium (20–29 pack-years) and high (40 pack-years or more) categories, the risk of lung cancer was similar for men and women.
Genetic Factors
Polymorphisms of genes that encode for enzymes involved in the breakdown of tobacco-derived carcinogens may potentially play a role in the development of lung cancer in female smokers and never-smokers. Arylamine N -acetyltransferase (NAT2) is an enzyme involved in biotransformation of xenobiotics, mainly aromatic and heterocyclic amines and hydrazines. NAT2 activity can influence the risk of lung cancer as well as cytochrome P (CYP)450 CYP1A2 activity (see Chapter 6 ). In nonsmoking Chinese women, low NAT2 activity and fast CYP1A2 activity were associated with a higher risk for the development of lung cancer, with an adjusted odds ratio of 6.9 compared with high NAT2 activity and slow CYP1A2 activity.
CYP1A1 is associated with an increased risk of lung cancer in female nonsmokers (odds ratio, 3.97; 95% CI, 1.85–7.28). CYP1A1 plays a role in converting tobacco carcinogens into DNA-binding metabolites that are important in DNA adduct formation. Glutathione S -transferase ( GSTM1 ) and GSTT1 are relevant for the detoxification of carcinogens. GSTM1 null genotype has been associated with an increased risk of lung cancer in some studies but not in others. One study conducted among Japanese women demonstrated an association between GSTM1 null genotype and an increased risk of lung cancer, particularly among female never-smokers with the null genotype. Additionally, an association was found between the GSTM1 null genotype and an increased risk of lung cancer in female never-smokers with the null genotype who had a substantial exposure to environmental tobacco smoke (odds ratio, 2.27; 95% CI, 1.13–2.7) compared with female never-smokers without the null genotype who did not have substantial exposure. Similar to GSTM1 , the null genotype of GSTT1 increases the risk for the development of lung cancer in never-smokers.
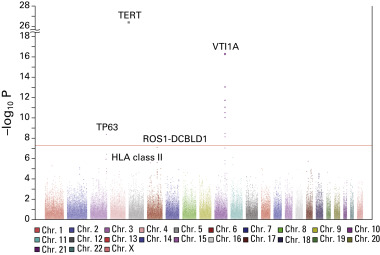
To gain insights into the etiology of lung cancer in never-smoking women, the Female Lung Cancer Consortium in Asia (FLCCA), which includes mainland China, South Korea, Japan, Singapore, Taiwan, and Hong Kong, was founded. The FLCCA identified a distinct pattern of environmental risk factors causally linked to lung cancer in never-smoking Asian women, as well as a distinct molecular phenotype of lung cancer in never-smokers by the identification of three new susceptibility loci at 10q25.2, 6q22.2, and 6p21.32 ( Fig. 5.5 ).
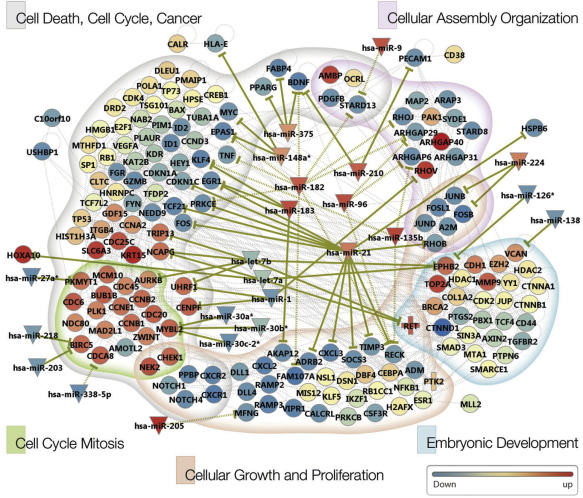
In six Korean female never-smokers, novel genetic aberrations, which included 47 somatic mutations and 19 fusion transcripts, were identified. Most of the altered genes were responsible for disturbances in G2/M transition and mitotic progression, causally linked to tumorigenesis in these patients ( Fig. 5.6 ).
In a study of the genotype of 3026 lung adenocarcinomas, correlation of the major epidermal growth factor receptor (EGFR) mutations (exon 19 deletions and L858R) and V-Ki-ras2 Kirsten rat sarcoma viral oncogene homolog (KRAS) mutations (G12, G13) with demographic, clinical, and smoking history data indicated a higher frequency of KRAS G12C mutations in women, who were also younger at the time of diagnosis than men with the same mutation (median age, 65 years vs. 69 years; p = 0.0008) and less exposed to active smoking. These findings support an increased susceptibility to tobacco carcinogens. Distinct differences in gender, age, and stage distribution were found for the two most common types of EGFR mutations.
Family History
Nitadori et al. evaluated the association between the incidence of lung cancer and family history in Japan. The authors concluded that, for women, the risk of lung cancer was higher if a first-degree relative was diagnosed with lung cancer (hazard ratio, 2.65, compared with 1.69 for men). However, this has not been a consistent finding. In a Taiwanese study, a family history of lung cancer in first-degree relatives was associated with a significantly increased risk of lung cancer for both men and women. In another study, there was a 1.51-fold increase (95% CI, 1.39–1.63) in lung cancer risk for individuals who had a first-degree relative with lung cancer compared with individuals who had no family history of the disease, after adjustment for proband age, proband gender, ethnicity, education, smoking status of the proband, pack-years of smoking, and study number. For ever-smoking individuals with a family history of lung cancer in a first-degree relative, the risk of lung cancer was increased 3.19-fold compared with never-smokers without a history of lung cancer in a first-degree relative. When stratified by relative type, the association was strongest for individuals who had a sibling with lung cancer (odds ratio, 1.82; 95% CI, 1.62–2.05), compared with a father (odds ratio, 1.25; 95% CI, 1.13–1.39) or mother (odds ratio, 1.37; 95% CI, 1.17–1.61). This pattern was similar in male and female probands (and for every histologic type examined), and the association was stronger among Asian individuals and those who were younger at the time of diagnosis (odds ratio, 1.83 and 1.45, respectively).
Viral Factors
Human papillomavirus (HPV) may play a role in the development of lung cancer, especially in Asia. Some studies have shown that the prevalence of HPV-16 and HPV-18 infection is higher among never-smoking women older than 60 years of age with lung cancer compared with control patients (without cancer). However, other studies have yielded different results. In a retrospective evaluation of 223 lung cancer cases, HPV infection had no role in the pathogenesis of primary lung cancer, whereas HPV positivity was indicative of pulmonary metastasis from a primary HPV-associated cancer elsewhere in the body. HPV has been associated with lung cancer in Asian populations, especially patients with EGFR activating mutations, who are often women. The prevalence of HPV infection among patients with lung cancer was 32% in a study from Taiwan; HPV infection and EGFR mutation were both found to be independently predictive of better survival.
Environmental Exposures, Diet, and Preexisting Lung Disease
Environmental Exposures
The relationship between gender and the risk of lung cancer due to environmental exposures (asbestos, radiation, other chemicals, radon) and diet has not been extensively investigated. The risk for lung cancer has been higher among never-smoking women exposed to asbestos (odds ratio, 3.5; 95% CI, 1.2–10) and pesticides (odds ratio, 2.4; 95% CI, 1.1–5.6). In a recent review, the burden of lung cancer in never-smokers attributable to previously identified risk factors was evaluated in different geographic regions. The population-attributable fractions of lung cancer related to the selected risk factors varied by geographic region. These risk factors appeared to be responsible for a substantial proportion of lung cancer in China, but accounted for a smaller proportion of cases in Europe and North America. In China, known risk factors accounted for a larger proportion of lung cancer cases in women than in men. For instance, increased levels of several carcinogens were found in the urine of nonsmoking Chinese women who reported frequent wok-style cooking. Radiotherapy for breast cancer has been reported to increase the risk of lung cancer particularly in smokers. Among women who received adjuvant radiotherapy after mastectomy the risk of lung cancer was increased for women who smoked (odds ratio, 18.9; 95% CI, 7.9–45.4), but not for never-smokers. According to data on 558,871 women with breast cancer in the Surveillance, Epidemiology and End Results (SEER) database who were followed for more than 20 years, the mortality rate was increased for women who had radiation therapy during 1973 to 1982 and 1983 to 1992, but not for women who had radiation therapy after 1993.
Exposure to high levels of radon is also associated with an increased risk for the development of lung cancer, particularly in smokers or people exposed to secondhand smoke. Bonner et al. reported data on 66 women that were pooled from several case–control studies in which exposure to secondhand smoke and radon was assessed. Among women exposed to residential radon, the risk of lung cancer was threefold higher for women who had the GSTM1 null genotype than for GSTM1 carriers (odds ratio, 3.41; 95% CI, 1.10–10.61), even after adjusting for age, smoking status, and secondhand smoke exposure.
In a Spanish study, the exposure to residential radon was evaluated in 69 never-smokers or light-smokers with lung cancer. The median concentration of radon in men’s homes was 199 Bq/m 3 , compared with 238 Bq/m 3 in women’s homes; the median concentration was 237 Bq/m 3 , a level higher than the reference level of 100 Bq/m 3 recently recommended by WHO. Higher radon concentrations were mainly associated with large cell and small cell histology. However, the study has some limitations, including the small cohort and the fact that residential radon concentrations among the participants were almost three times higher than that found in almost 2500 homes in the region studied.
Diet
In case–control and cohort studies, high dietary intake of fruits and vegetables has reduced the risk of lung cancer. Tomatoes and cruciferous consumption have also been associated with a decreased risk for lung cancer. More than 71,000 Chinese women with no history of smoking or cancer at baseline were prospectively evaluated for their dietary intake with a follow-up time exceeding 11 years. The main food contributors to riboflavin intake were rice, fresh milk, eggs, and bok choy; dietary riboflavin intake was inversely associated with lung cancer risk (hazard ratio, 0.62; 95% CI, 0.43–0.89; p = 0.03 for the highest quartile compared with the lowest). In the same cohort, the intake of soy food before the diagnosis of lung cancer was associated with better overall survival.
Preexisting Lung Disease
Preexisting lung diseases such as asthma and COPD can represent other potential risk factors for lung cancer. Several case–control studies have demonstrated an increased risk for the development of lung cancer in both men and women diagnosed with these nonneoplastic lung diseases. Even after controlling for active and passive tobacco exposure, some studies have shown an increased risk for lung cancer. Wu et al. found that the risk for lung cancer was increased for nonsmoking women with previous lung disease (adjusted odds ratio, 1.56; 95% CI, 1.2–2.0) and this finding was mainly driven by the prevalence of tuberculosis in this population.
Steroid Hormones in Lung Cancer
Classical steroid hormone pathways have been successfully targeted in the treatment of breast and prostate cancer, where hormone-dependent growth has been well established. Steroid hormone receptors are known to be expressed in tissues outside the reproductive tract and to have biologic effects in tumors in nonreproductive sites. Some effects mediated by steroid receptors appear to be independent of steroid ligands and result from activation of steroid receptors by phosphorylation pathways. Steroid hormone receptors could thus have biologic activity via steroid-induced signaling or steroid-independent signaling. The findings of population studies and preclinical research suggest that steroid hormone pathways are involved in the biology of lung cancer, and the estrogen signaling pathway is a promising target for lung cancer therapy. The progesterone receptor (PR) may play a role in lung cancer biology as well.
Estrogen Receptors
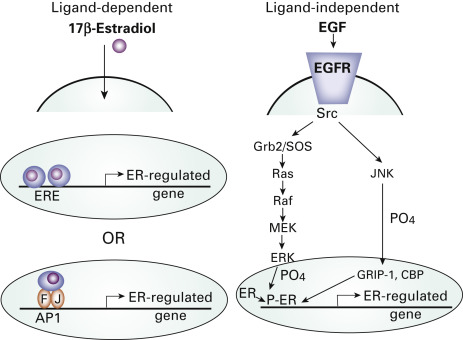
The results of studies of gender differences in lung cancer risk and disease presentation suggest that estrogen may be involved in the etiology of this disease. For example, women are more likely than men to have adenocarcinoma of the lung and to be never-smokers. Also, the rate of diagnosis of lung cancer among never-smoking women is higher than among never-smoking men. Estrogen receptors (ERs), members of the nuclear steroid receptor superfamily, mediate cellular response to estrogen. These proteins either function as ligand-activated transcription factors or can be activated by phosphorylation independent of ligand ( Fig. 5.7 ). Two forms of the ER have been identified, ERα and ERβ, which are encoded by separate genes and display different tissue distributions. In addition, multiple isoforms of ERα and ERβ exist, including at least five ERβ isoforms.
The reports on the presence of ERs in lung tumors have been inconsistent. These differences could be due to interpretation of staining, antibodies and dilutions used, variability in the scoring assessment, or differences in patient cohort characteristics. With the identification of antibodies that distinguish between ERα and ERβ and more standard immunohistochemical procedures, it is now clear that ERβ is expressed and functional in most human nonsmall cell lung cancer (NSCLC) cell lines and is present in primary specimens of human NSCLCs from both men and women. However, the frequency and function of the different ERβ isoforms in lung cancer are still not completely understood. There is less agreement about the expression of ERα in the lung. ERα was mainly found in the cytoplasm and membrane in immunohistochemical studies and was found to be composed of mostly alternatively spliced variants on immunoblot and RNA analysis. This nonnuclear ERα pool may consist of a variant isoform that lacks the amino-terminal because it is differentially detected by antibodies that recognize the ERα amino- and carboxy-terminal. ERβ, in contrast, is found in both the nucleus and the cytoplasm and is composed of mainly full-length protein in addition to some variants. ER-mediated RNA transcription and proliferation in lung tumor cell lines support the hypothesis that at least some forms of ER are functional.
Several reports relating ER status to survival in NSCLC have shown nuclear localization of ERβ in 45.8% to 69% of lung cancer cases, which was found to be a favorable prognostic indicator in some studies. In some reports, the prognostic significance was found only in men or was limited to a subset of patients with a particular mutation. However, most of these studies used antibodies to total ERβ that did not distinguish between the different ERβ isoforms. Recently, cytoplasmic ERβ-1 was identified as an independent negative prognostic factor for lung cancer. This isoform specificity was confirmed in an additional study that showed that ERβ-1, but not ERβ-2, was linked to a worse prognosis in women with stage I lung cancer. Nuclear ERβ-1 correlated with poor survival for patients with metastatic lung cancer but not in a cohort of patients with early-stage lung cancer. Both ERβ-2 and ERβ-5 have been linked to better survival in lung cancer.
Nuclear ERα expression is never or rarely detected in NSCLC tumors. Prognostic significance of ERα was shown to have either no effect on survival or to correlate with poor prognosis. Kawai et al. reported that the presence of cytoplasmic ERα is associated with a worse prognosis among patients with NSCLC. Clearly, both nuclear and cytoplasmic ERs are important, and each component should be assessed separately and together when examining tissue specimens for clinical evaluation. In addition, further analysis on the various ERβ isoforms will be necessary to completely understand the role of ERβ in lung cancer. Standardized approaches should be developed and validated for screening of lung tumor ERs to validate the prognostic significance of these hormone markers. These markers may also be useful to identify patients who may have a response to hormone therapy for lung cancer.
Several studies have shown that women with advanced NSCLC live longer than men with advanced NSCLC. A population study examining lung cancer presentation and survival in premenopausal and postmenopausal women demonstrated that more premenopausal women had advanced disease at the time of diagnosis, including poorly differentiated tumors with less favorable histologies. However, in that study, survival for the two groups did not differ significantly. In a more recent study, women older than 60 years of age had a significant survival advantage over both men and younger women; the difference compared with younger women is potentially due to higher levels of circulating estrogen in the younger population. Survival did not differ by age among men.
Exposure to exogenous estrogens through hormone replacement therapy (HRT) has a negative effect on lung cancer survival. Ganti et al. evaluated nearly 500 women with lung cancer and found a significant association between both a lower median age at the time of lung cancer diagnosis and a shorter median survival time for women who used HRT around the time of diagnosis compared with women who did not. This effect was more pronounced in women who smoked than in women who did not, suggesting an interaction between estrogens and tobacco carcinogens. The Women’s Health Initiative also reported a strong adverse effect on survival after a lung cancer diagnosis in women who received HRT. In that randomized, placebo-controlled trial, more than 16,000 postmenopausal women received placebo or daily HRT for 5 years. The likelihood of dying from lung cancer was significantly greater in the HRT group, with a trend toward more lung cancer diagnoses compared with the placebo group. This increase in lung cancer incidence by HRT was also demonstrated in the Vitamins and Lifestyle Study, and the effect of HRT on lung cancer risk was duration dependent. However, the findings of other studies have suggested that HRT use could actually protect women from the development of lung cancer, especially if they smoked. An inverse relationship was also found between HRT use and NSCLC risk in postmenopausal women with ER-positive but not ER-negative lung tumors. This finding may suggest different effects on the balance between induction of cell differentiation and cell proliferation by estrogen in normal lung epithelium compared with malignant epithelium. Because lung tumors are also known to produce aromatase (discussed later), it is possible that use of exogenous hormones reduced local estrogen production by inhibiting aromatase expression. Exact HRT used, duration of use, and timing of use is crucial information needed to elucidate the exact role of HRT on lung cancer risk and survival of women with lung cancer in future studies.
Retrospective population studies have recently demonstrated that antiestrogen use can influence survival in lung cancer. An observational study that included more than 6500 women with breast cancer showed significantly lower lung cancer mortality for women who received antiestrogen treatment. Similarly, in the Manitoba Cancer Registry, in which 2320 women with or without exposure to antiestrogens were evaluated, antiestrogen use both before and after lung cancer diagnosis was significantly associated with decreased mortality. Together, these studies on HRT and antiestrogen use support the idea of estrogen acting as a promoter of lung cancer aggressiveness and formation and perhaps having a key role not only in the biology but also the outcome of lung cancer.
Preclinical evidence also demonstrates that estrogen is a major driver of lung cancer. Estrogen acts to induce cell proliferation of NSCLC cells in vitro and in vivo and can modulate expression of genes in NSCLC cell lines that are important for inducing cell proliferation. Genomic estrogen signaling has been demonstrated to occur mainly through ERβ in NSCLC cells. Furthermore, fulvestrant, an ER antagonist with no agonist effects, inhibits cell proliferation in vitro and lung tumor xenograft growth in severe combined immunodeficient mice by approximately 40%. Thus, preclinical evidence strongly suggests that targeting the estrogen signaling pathway may have therapeutic value in the treatment or prevention of lung cancer.
Three strategies are currently available to target the estrogen signaling pathway in cancer cells: (1) antagonists of ER function through drugs such as tamoxifen and raloxifene; (2) downregulation of ER function through agents such as fulvestrant; and (3) reduction of estrogen levels through aromatase inhibitors, such as the reversible nonsteroidal agents letrozole and anastrozole and the irreversible steroidal inactivator exemestane. Tamoxifen and raloxifene have partial agonist effects in certain tissues, such as endometrium. Tamoxifen has been shown to increase lung tumor xenograft growth and is not an appropriate choice of therapy for NSCLC. Additionally, the National Surgical Adjuvant Breast and Bowel Project Breast Cancer Prevention Trial did not show any decreased risk of lung cancer. Seventeen tumors of the lung, trachea, and bronchus were reported among the placebo group, and 20 were reported among the women in the tamoxifen group. Although not significant, these results suggest that tamoxifen could have some agonistic effects in the lung.
Aromatase
Lung cancer cells can also produce their own estrogen. The aromatase enzyme, a member of the CYP450 family, catalyzes the conversion of the androgens androstenedione and testosterone to estrone and estradiol, respectively, and is expressed in the lung. Preclinical work suggests that aromatase inhibitors are also potential inhibitors for lung cancer therapy. Aromatase protein was expressed in lung tumor cell lines and tumor tissue and was demonstrated to be functional. Additionally, the growth of lung tumor xenografts decreased substantially when treated with anastrozole. Anastrozole was recently shown to prevent tobacco-induced lung carcinogenesis in female mice, and this effect was further enhanced when anastrozole was combined with fulvestrant. Interestingly, in this animal model of lung cancer prevention, aromatase expression was confined almost exclusively to inflammatory cells that had infiltrated preneoplastic areas of the lungs, whereas the abnormal epithelial cells were mostly negative. Thus, an important source of estrogen synthesis may be inflammatory cells that infiltrate the lungs in response to carcinogens, beginning early in carcinogenesis. This local production of estrogen may be part of the chronic inflammatory reaction occurring in lung tumors. Aromatase inhibitor therapy in lung cancer is further supported by Coombes et al., who reported a decreased incidence of primary lung cancer in women with breast cancer who were treated with exemestane after 2 years to 3 years of tamoxifen therapy (4 women) compared with continued tamoxifen treatment (12 women).
Mah et al. identified aromatase as an early-stage predictive biomarker of lung cancer survival. Among women older than 65 years of age, lower levels of aromatase in tumor tissue predicted a greater chance of survival compared with women who had tumors with higher levels of aromatase expression. Furthermore, the prognostic value of aromatase expression was greatest for patients with stage I or II lung cancer. In this population of patients with low levels of circulating estrogen levels (because of decreased production by the ovaries), tumor cells could compensate for the loss by producing estrogen through aromatase. However, no general association between aromatase and lung cancer survival was found in a separate cohort unless aromatase expression was combined with that of other markers, such as ERβ, EGFR, and PR. These results strongly suggest that aromatase inhibitors, which are already approved to treat breast cancer, may be of use to treat lung cancer in women with lung cancers that have high levels of aromatase. Aromatase expression may also be a new tool to predict survival at an early stage of disease, when more treatment options are available. A phase I clinical trial (NCT01664754) is currently underway to evaluate the side effects and best dose of the aromatase inhibitor exemestane in combination with pemetrexed and carboplatin to treat late-stage lung cancer. Other enzymes involved in intratumoral production and metabolism of estrogens are currently under investigation as potential targets for lung cancer therapy.
Nongenomic Estrogen Signaling and Interactions With Growth Factor Receptor Signaling Pathways
In addition to the nuclear mechanisms of ER action, such as increased cell proliferation and gene transcription, estrogen can also rapidly activate signaling in seconds to minutes. These rapid signaling effects are referred to as nongenomic effects and occur via nonnuclear ERs located in the membrane or in the cytoplasm ( Fig. 5.8 ). In human breast cancer cells, a membrane ER was identified as a G protein–coupled receptor called GPR30. Expression of GPR30 has recently been demonstrated in lung cancer cells, but the function and regulation of GPR30 in the lung is still unknown. In NSCLC cells, other extranuclear ERs have been identified in plasma membrane fractions and cytoplasmic fractions and have been shown to promote rapid stimulation of signaling pathways. These effects can be inhibited by the addition of fulvestrant.
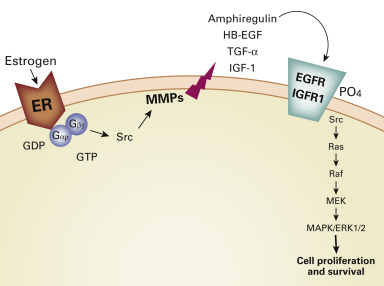
Nongenomic ER signaling acts in concert with growth factor signaling pathways, such as EGFR/HER-1 and the insulin-like growth factor 1 receptor (IGF-1R). EGFR is a member of the tyrosine kinase receptor family that also includes HER2, HER3, and HER4. These receptors have been implicated in proliferation, cell motility, angiogenesis, cell survival, and differentiation. Clinically, overexpression of EGFR correlates with poor prognosis in people with NSCLC. Furthermore, combined overexpression of EGFR and ERα was demonstrated to be an independent indicator of poorer prognosis in lung cancer, consistent with cross-talk between these two pathways. An interaction between ER and EGFR has been demonstrated in lung cancer cells. In this regard, estrogen can rapidly activate EGFR in lung cancer cell lines (ligand-dependent signaling) and the combination of fulvestrant and gefitinib, an EGFR tyrosine kinase inhibitor (TKI), in NSCLC can maximally inhibit cell proliferation, induce apoptosis, and affect downstream signaling pathways both in vitro and in vivo. The more clinically relevant EGFR TKI, erlotinib, also showed superior antitumor activity in NSCLC tumor xenograft experiments when used in combination with fulvestrant compared with single agent therapy as well as a multitargeted TKI, vandetanib. A synergistic effect of gefitinib and the aromatase inhibitor anastrozole was found in lung cancer cell lines, further supporting a functional interaction between these pathways. In addition, membrane ERs were found to be colocalized with EGFR in lung tumors. Ligand-independent nongenomic signaling can also occur. EGF can directly phosphorylate ER at specific serine residues. These residues were found to be phosphorylated in 87.5% of ER-positive lung tumors examined.
A reciprocal control mechanism was also observed between ER and EGFR in lung cancer cells. EGFR protein expression was downregulated in response to estrogen and upregulated in response to fulvestrant in vitro, suggesting that the EGFR pathway is activated when estrogen is depleted. Conversely, ERβ protein expression was downregulated in response to EGF and upregulated in response to gefitinib, providing a rationale to target these two pathways simultaneously. Similar cross-talk has also recently been reported between the estrogen signaling pathway and the IGF-1R pathway in lung cancer. The IGF-1R signaling pathway has been implicated in lung cancer development. Estrogen has been shown to upregulate IGF-1R expression specifically through ERβ in lung cancer cells and tissues. Furthermore, both aromatase and ERβ expression were positively correlated with IGF1 and IGF-1R expression. These pathways have also been demonstrated to act synergistically to promote the development of lung adenocarcinomas in mice. Additionally, combined treatment with fulvestrant and an IGF-1R inhibitor showed maximum antitumor effects compared with single agent treatment in a carcinogen-induced lung cancer murine model. Targeting EGFR through small molecule TKIs is of limited use in the absence of an EGFR mutation, which occurs in a minority of patients. Interestingly, the patients who have a response to EGFR TKIs are mainly women and never-smokers, which may relate to the bidirectional signaling between EGFR and ER in lung cancer. Additionally, some studies have demonstrated a correlation between EGFR mutation and ER expression. These observations have been translated to a phase I clinical trial using drugs that target these two signaling pathways to assess the toxicity of combined treatment with gefitinib and fulvestrant in 22 postmenopausal women. Targeting both pathways was found to be safe and have antitumor activity in women with stage IIIB/IV NSCLC. Additionally, nuclear ERβ was correlated with improved patient survival. A phase II trial comparing the combination of erlotinib and fulvestrant with erlotinib alone showed that the combination treatment was well tolerated and progression-free survival was similar for the two treatments. In patients with EGFR wild-type tumors, the clinical benefit rate was significantly higher among patients treated with the combination (3 people who had a partial response) compared with erlotinib alone, with a trend toward improved survival. The findings of these clinical trials suggest that targeting the ER signaling pathway via both nuclear and extranuclear receptors in conjunction with the EGFR signaling pathway has increased beneficial antitumor effects in NSCLC, as has been observed in breast cancer cells, particularly in patients whose tumors do not contain an EGFR mutation. The combination of antiestrogen therapy with an IGF-1R inhibitor also warrants clinical investigation.
Progesterone Receptors
Progesterone effects are mediated through the PR. There are two main isoforms of PR, PR-A and PR-B, which play different roles in modulating cellular responses to progesterone. In general, the presence of PR in breast cancer indicates a more differentiated tumor that is responsive to antiestrogen therapy, and PR is a known estrogen-responsive gene. The ratio of PR-A:PR-B is thought to affect the clinical outcome in breast cancer. Several studies have demonstrated the expression of total PR by primary NSCLC, although the reported frequency of expression has varied greatly. Several studies found little or no PR in NSCLC, whereas PR expression was lower in lung tumors than in matched normal lung tissue. Two studies showed that PR is a strong protective factor for lung cancer. The antibodies used in these lung cancer survival studies do not distinguish between the PR-A and PR-B isoforms, which could exert different functions. Enzymes capable of synthesizing progesterone were also detected in many NSCLCs, and a positive correlation was found between intratumoral levels of progesterone and the presence of three enzymes that participate in progesterone synthesis. Progesterone treatment led to growth inhibition of tumor xenografts and concomitant induction of apoptosis, in agreement with clinical data suggesting that the presence of PR was correlated with longer overall survival in NSCLC. In addition, progesterone has been shown to inhibit the migration and invasion of lung cancer cell lines. In breast cancer, PR is known to signal through ligand-independent mechanisms due to phosphorylation by kinases. One mechanism for low tumor PR expression in breast tumors is through increased growth factor signaling, which leads to a more aggressive tumor biology with faster progression. Whether this same mechanism occurs in lung tumors is unknown and is currently being investigated.
Progesterone derivatives have been useful in the treatment of both endometrial cancer and breast cancer. Agents such as medroxyprogesterone acetate, which can be given orally, have potential for treatment of lung cancer, perhaps in combination with agents that suppress either the ER pathway or act on growth factor pathways such as EGFR or c-Met, or other TKIs. Long-term progesterone treatment may even be feasible for chemoprevention of lung cancer.
Implications for Lung Cancer Therapy
Research on estrogen in lung cancer is likely to benefit both men and women. Because lung tumors from both men and women express ER and aromatase and cell lines derived from both men and women respond to estrogens, antiestrogens, and aromatase inhibitors, these types of treatments may be beneficial for both populations, not solely women. Preclinical evidence suggests that these hormone therapies are effective in male mice (Stabile and Siegfried, unpublished data). Further understanding of the role of estrogen, estrogen synthesis, and ERs in lung cancer will provide a rationale for future targeting of this pathway for therapy earlier in the course of disease and possibly for lung cancer prevention. Additional understanding of the role of nonnuclear versus nuclear ERs as well as PRs in lung cancer and which drugs affect which receptors will be important for designing new effective treatments and clinically exploitable strategies. As hormone therapies are currently being evaluated in the clinic for lung cancer, identification of patients most likely to benefit is warranted to guide the design of future clinical trials targeting this pathway. Biomarker identification will be key to selecting the best candidates for hormone therapy in lung cancer. Because antiestrogens are safe and can be given for long periods of time, there is tremendous potential to bring them to clinical use for lung cancer.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree