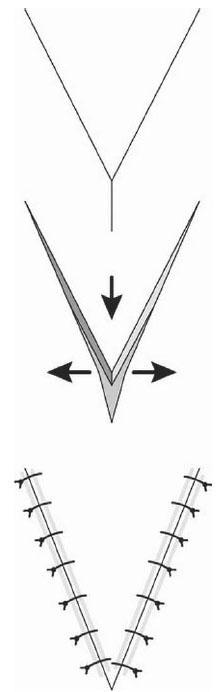
Figure 12.2 A preoperative picture of an ischemic and infected right second digit (A), followed by an amputation at the metatarsophalengeal joint level, and closure by a double V-Y flap (B). A final clinical postoperative outcome (C).
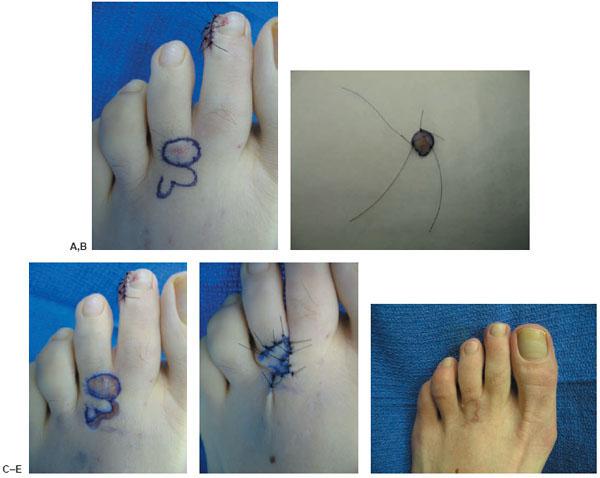
Y-V PLASTY
The Y-V plasty is the opposite of the V-Y flap by increasing tension in line with the Y to V and releasing tension perpendicular to the flap. The procedure is usually performed as series of multiple Y-V incisions. These flaps are done in a series to release a contracture over the dorsum of the forefoot, in areas of burn scar contracture, or in contracted digits. The incisions of the Y-V plasty are carried deep into the subcutaneous tissue layer with gentle undermining of the surrounding tissue. The subcutaneous tip of the flap should be gently held in position with a skin hook, with care taken not to damage the skin layer of the tip. When the contracture is released, the Y incisions are closed with simple interrupted sutures at the base to release tension on the apex. The closure is comparable to that of a Z-plasty flap (Fig. 12.3) (106).
V-Y-S PLASTY
This skin plasty combines the V-Y plasty technique with the rotation flaps of the S-plasty. This combination maximizes tissue conservation and reduces the need for undermining the wound edges. Circular defects lend themselves to this procedure, and it is effective in areas on the extremities where the skin is taut.
Once the lesion has been outlined with a skin marker, an ellipse or fusiform drawing in the typical 3-to-1 pattern further encompasses the circular mark. The long axis of this marking lies parallel to the maximal skin tension lines, along the relaxed skin tension lines or skin folds. The circular defect is excised, leaving two triangular sections on either side of the defect. An intact side of one of the triangles is incised along its entire length and a back cut is made along approximately 30% to 50% of the remaining side. This produces a flap that hinges on one partially intact side. When creating the back cut on each side, it is important not to exceed cutting >50% of one side. Back cuts that exceed 50% greatly increase the risks of vascular compromise to the flap and enhance possible flap necrosis. This is even more of a possibility in skin that is under significant tension. The V-Y-S-plasty closure of circular defects conserves tissue and it also eliminates the need for undermining of wound edges (111). Once the first flap is made, the second triangle is then transformed into a flap in a similar manner, but the relative positions of the incisions are reversed, the two triangles are then rotated toward each other and sutured into place. A small amount of undermining may be performed beyond the flaps to close them, but usually this is not necessary. The small remaining defects are then closed in the V-Y technique with minimal displacement of adjacent tissues. The resultant closed incision resembles “$”; hence, the slang term dollar plasty (106). The V-Y-S plasty is also useful for the extremities in which skin is under considerable tension (111).
Figure 12.3 Y-V plasty that is the opposite of the V-Y flap by increasing tension in line with the Y to V and releasing tension perpendicular to the flap.
CRESCENTIC ADVANCEMENT FLAP
The crescentic advancement flap can be used to close a triangular defect. As described by Jackson (36), a crescent-shaped incision is made extending from the base of the triangle and the resulting skin excised. The outer edge of the crescent should be equal to or slightly less than the combined length of the base of the triangle and the length of the inner edge of the crescent. The flap created between the triangular defect and the crescent-shaped donor site is widely undermined and advanced into the triangular defect.
OBLIQUE SIGMOID ISLAND FLAP
The oblique sigmoid island flap is a variation of a V-to-Y flap and is used to close small circular defects (73). After the lesion is excised in a circular fashion, two small 1- to 2-mm triangles are excised from opposite sides of the defect. The triangles should be positioned such that their apices are pointing along the RSTL. Next, a line should be drawn tangent to the circular defect and parallel to the RSTL. A flap is then designed using the tangent line as an axis. The width of the flap should be equal to the diameter of the defect. The side of the flap closest to the defect has an S-shaped edge and the side away from the defect has a spindle-shaped edge. The flap is then advanced obliquely into the defect and the remaining incision line is closed directly. This technique has been performed successfully on defects up to 10 mm in diameter (73). Skin plasties for congenital fifth digit contractures can also be included in this category. V-to-Y flaps create a functional and cosmetically pleasing outcome.
A V-shaped incision is made, with the length of the flap one and a half to two times as long as the diameter of the defect. The incision made in the plane of advancement is as wide as the perpendicular diameter (2,62,66–89,91,93,94,100,101,104). The flap should be designed such that the resulting stem of the “Y” lies perpendicular to the RSTL. This produces movement of the flaps along the LME. The resulting V-shaped flap is raised and advanced, with minimal tension. To increase the amount of advancement possible, the thickness of the flap, or the amount of undermining, may be varied, while being careful to preserve the underlying subcutaneous structures (66). Undermining of the pedicle of the flap should be minimized, whereas undermining the surrounding skin is advisable (66). The remaining deficit is closed, thereby forming the stem of the “Y.” Flaps can be moved from 1 to 2 cm (3–14) or 1 to 3.5 cm (64), depending on the author. Some authors have been able to advance the flap 3 to 4 cm, depending on the elasticity of the skin (91).
The extended V-to-Y flap, one variation of the standard V-to-Y flap, may be used for large defects and in regions with decreased mobility (77). As with the standard V-to-Y flap, the length of this flap measures one and a half to two times the diameter of the defect. One of the advantages of this flap is that it reduces the occurrence of trap doors, dog ears, and unnatural depressions at the sutured site (73). Disadvantages include a somewhat complicated operative technique that often includes delicate flap trimming and a slightly long scar (73).
ROTATION FLAPS
Rotation flaps are those that pivot around a point and move through an arc. These flaps include single rotation flaps, double rotation flaps, and the Satterfield-Jolly flaps. Rotation flaps provide redistribution and redirection of tension from the primary defect to the donor site (30). They are frequently used in areas with convex surfaces or where tension lines are curved (30). Rotation flaps can be subfascial or suprafascial, as described by Shaw and Hidalgo (86). They can also be fasciocutaneous, myocutaneous, or a combination of both. Rotation flaps can be axial or random, depending on the level of dissection and angiosome involved.
Rotation flaps can be elevated from the non–weight-bearing arch to areas of pathologic weight-bearing surfaces. They allow for movement of premorbid tissue for coverage in areas that require durable and mobile tissues. They can be used to correct defects on the plantar aspect of the heel by including the heel pad (29). They can also be used to cover large defects in the foot; however, they often require a skin grafting component for closure of the donor site.
Rotation flaps are an excellent adjunct in Charcot foot reconstruction. Because of their inherent design, they can yield a wide-based exposure to the plantar osseous structures that are often subluxed or dislocated in neuropathic arthropathies. Fasciocutaneous rotation flaps can be rotated from medial to lateral to provide adequate coverage of plantar hardware used for the Charcot foot or for unstable midfoot and rearfoot pathologies (92). Because of the required skin grafting component, strict elevation and bed rest must be enforced for 5 to 7 days, therefore increasing hospitalization and cost.
CLASSIC ROTATION FLAP
The rotation flap consists of a triangle or two radians or wedges from a portion of a circle. If the rotation flap does not cover the entire defect it may be designed larger or the length of the curved incision may be extended to free more tissue. Additionally, if even more movement is needed, a back cut may be employed to the arc of the flap. The rotation flap used to close a circular defect is usually a combination of both primary and secondary movements. The primary movement is the rotation and advancement of the flap itself over the defect and the line of the greatest tension extends from the pivot point toward the defect site. This distal tension point is the area of greatest vascular compromise. The secondary movement is the movement of the adjacent or surrounding skin in the opposite direction of the flap movement. The skin from the side of the defect opposite to the flap moves over the defect more than the flap itself moves over the defect. This requires less rotation of the flap and creates less puckering at the flap pedicle. When puckers occur they may be eliminated by cutting a Burrow’s triangle at the end of the incision (106).
SINGLE ROTATION FLAP
A single rotation flap may be used to close either a triangular or circular defect. For closure of a triangular defect, the flap is shaped semicircular and rotates about a pivot point.
For a triangular defect, the base of the defect becomes part of the circumference of a semicircle (Fig. 12.4). An arch-shaped flap is then designed so that the leading tip of the flap will rotate around the circumference of the circle on which the defect lies. To enable primary closure of the donor site, the flap should have a circumference five to eight times the width of the defect (19) or an area of three to four times the area of the defect (30). The major movement is in the direction of the arc of rotation of the flap. Secondary movements of the adjacent or surrounding skin in the opposite direction of the flap movement also occur. Key sutures are placed along the closing edge or shorter side of the flap. Burrow’s triangles may be used at any point along the arc or longer incision, but are typically found at the base of the flap. The narrower the triangular defect, the less distance the flap will need to move (22); therefore, the defect should be excised with as narrow a triangle as possible.

Figure 12.4 A single rotation flap being used to close a triangular defect. Note that the flap is shaped semicircular and rotates about a pivot point.
The use of a back cut, incised at the pivot point of the flap, is controversial. Some (3,30,36,44) feel that back cuts allow for additional mobility of the flap, allowing it to be inset into the defect with little tension. Others feel that back cuts into the base should be avoided. If a back cut is used, it should be cut away from the base if possible or its length should be minimized to avoid jeopardizing the perfusion of the flap. To avoid potentially compromising the vascularity of the flap when using a back cut, perforators into the flap should be evaluated with the use of a Doppler (3).
If the flap will not close without excessive tension, then a maneuver described by Jackson (36) should be used. In this technique, the circumference of the rotation flap is increased, thereby lengthening the leading edge of the flap and allowing closure with decreased tension.
For a circular defect, an arc is created that is tangent to the circle, having a greater radius than the defect. The resulting flap is then rotated into the defect. In this case, there is usually a combination of both primary and secondary movements, in varying degrees depending on the elasticity of the surrounding skin. The primary movement is the rotation of the flap into the defect. The secondary movement is the movement of the surrounding tissue in the opposite direction of the flap movement. If puckering of the flap occurs, then a Burrow’s triangle may need to be excised from the end of the flap (Fig. 12.5).
DOUBLE ROTATION FLAP
The double rotation flap, also known as O-to-Z flap, S-plasty, biwinged flap, and V-Y-S plasty is a variation of the standard fusiform incision for closing circular wounds. It disperses the tension of closure along three lines, as opposed to just one line when a simple elliptical closure is used. It also preserves premorbid and nonpathologic tissues.
With the O-to-Z flap, two arc-like incisions are made tangential to a circular defect. The radii of the arcs are greater than that of the original defect. The incisions are made on opposing sides of the defect and do not need to be of equal length. Burrow’s triangles may be used where needed. The sides of the defect are approximated and sutured in place, creating the central line of the “Z.” These are key sutures and are under the greatest tension. The arc-like incisions are then closed, creating the final two lines of the “Z.”
Figure 12.5 A delayed single rotation flap at the initial heel ulcer débridement (A), followed by a delayed closure (B). A final clinical postoperative outcome (C).
With the biwinged flap, the lesion is bisected with a line that runs parallel to the RSTL. The line should be approximately three times the length of the diameter of the lesion. Two equal triangles are then excised on each side of the bisector, such that the base of the triangles is one fourth to one half the diameter of the lesion. When the skin edges are re-approximated, the resulting incision resembles a rounded step or a lazy “S.” It should be noted that the central arm of the “S” is placed under increased tension and care must be taken when suturing to ensure adequate wound approximation (14). It was determined that the biwinged flap used minimal amounts of surrounding tissue to close a defect, when compared with a standard fusiform incision (32). Lesions on all areas of the foot, including plantar and medial lesions, can be excised using the biwinged flap, and for some authors (20) this flap has replaced the use of elliptical closure for circular defects.
The V-Y-S plasty is a variation of the O-to-Z flap and involves placing V-to-Y advancement flaps on the ends of the arcs, resulting in an S-shaped incision. It controls the amount of tissue displacement that occurs at the ends of a double rotation flap and minimizes asymmetry.
SATTERFIELD-JOLLY ROTATION FLAP
The Satterfield-Jolly flap (83) is a variation of a single rotation flap, which is used to close excisions of painful plantar forefoot lesions. First, a medial to lateral transverse incision is made along the plantar margin of the sulcus, following its natural arc. Then, a triangular portion of skin, containing the lesion, is excised. This triangle is designed so that its base is formed by the initial transverse incision and its apex is proximal. The triangle is typically four to five times as long as it is wide. The underlying plantar fat is left intact. The leading edge of the flap is undermined at the fascial plane. The amount of undermining should be kept at a minimum, performing only the amount necessary to allow tension-free movement of the flap. Burrow’s triangles are typically necessary along the length of the transverse incision, interdigitally, high in the sulcus. The flap is then sutured into place, without tension.
Figure 12.6 The Catanzariti-Wehman rotation flap for complete closure of plantar defects without the need for Burrow’s triangles.
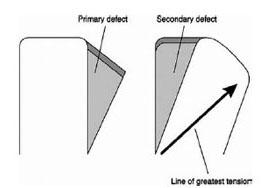
Figure 12.7 A transposition flap that moves over adjacent intact skin to close a defect and combines the use of both rotation and advancement techniques.

Figure 12.8 A transposition flap created to close a plantar defect (A), followed by insetting the flap to the original defect (B), and close of the donor site with a split-thickness skin graft harvested from the plantar aspect of the same foot (C). A final clinical postoperative outcome (D).
Advantages of this flap include a non–weight-bearing scar, primary closure of the donor site and flap simultaneously, and a broad-based exposure to underlying structures of the metatarsal parabola.
CATANZARITI-WEHMAN ROTATION FLAP
A very similar approach using a modified rotation flap was described by Catanzariti and Wehman in 1988. The wedge is much smaller and the incision along the arc is much longer. This provides for complete closure without the need for Burrow’s triangles, but the design places more of the incision on the ball of the foot. The curved incision is brought down across the plantar ball, trying to avoid the weight-bearing surfaces as much as possible. They are especially useful in the removal of hypertrophic scars or triangular lesions on the plantar aspect of the foot (Fig. 12.6) (106).
TRANSPOSITION FLAPS
Transposition flaps are similar to rotation flaps except these flaps are tongue-like in shape and generally have narrower bases than rotation flaps. The surface area of a transposition flap is less than the surface area of a rotation flap covering a defect of the same size. Transposition flaps are also more likely than rotation flaps to require split-thickness skin grafts to close their donor sites, especially in the plantar arch. Transposition flaps are more capable than rotation flaps of covering large wounds in the plantar hindfoot because the coverage of the donor site by a split-thickness skin graft augments the total surface area. A number of modifications to the standard transposition flap have been described and many have been used in the foot. These modifications include rhomboid flaps, bilobed flaps, and Z-plasties (97).
Transposition flaps (Fig. 12.7) move over adjacent intact skin to close a defect and combine the use of both rotation and advancement. These flaps include the single lobe flap, the bilobed flap, Z-plasty, double-Z rhomboid, double opposing Z-plasty or five-flap Z-plasty, four-flap Z-plasty, double opposing semicircles, W-plasty, the rhomboid or Limberg flap, flap of Dufourmentel, the 30-degree transposition flap, double and triple rhomboid flaps, and the note flap. As with rotation flaps, these flaps redistribute and redirect tension from the primary defect to the donor site (30). It is critical that the flap extend beyond the defect, thereby ensuring adequate length after its transposition (19). If additional length is required, a back cut away from, or into, the base can be made; the latter option poses a risk of reducing the blood supply into the flap (19). Closure of the donor site may be primary, if the adjacent skin is elastic enough, but more likely a skin graft or another skin flap will be required (Fig. 12.8).
SINGLE LOBE FLAP
The single lobe flap, also known as the Schrudde slide-swing plasty (Fig. 12.9), may be used to close circular, oval, and semicircular defects (84). It has been used successfully for removal of small digital lesions, such as fibrous scars, intractable keratoses, and digital mucoid cysts (22) and to close a defect plantar to a metatarsal head (Fig. 12.10) (1,10–28).
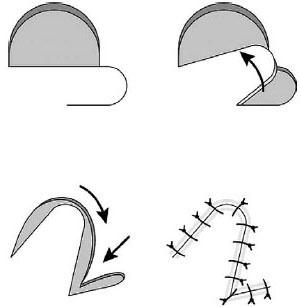
Figure 12.9 The single lobe flap, also known as the Schrudde slide-swing plasty may be used to close circular, oval, and semicircular defects.
To close a circular defect, a flap in the shape of a lobe is created. The rounded end of the flap is designed with a radius smaller than the circular defect and the flap as a whole is designed to be smaller in size than the original defect. The base of the flap is placed at a 90-degree angle to the defect (84). The length to width ratio is typically 3:1 (30). Key sutures are at the distal ends of the flap. The donor region is closed primarily.
To close an oval defect, a similar flap is designed, but the base of the flap is placed at a 60-degree angle to the defect (Fig. 12.11) (84). The advantages of a single lobe flap are that it can be used to close a large defect, its broad base ensures good vascularity, and it avoids a secondary defect (22). Because most lesions are circular and this flap was designed to close a circular defect, it does not involve additional excision of healthy tissue to produce a defect of a specific geometrical figure such as a rhombus (84). It should be noted that up to one third of the flap length may be lost during transposition of the tissue into the defect (30). The disadvantage of a single lobe flap may be that too much tension is created and closure is not possible without an additional lobe to disperse the tension.
BILOBED FLAP
The bilobed flap consists of two flaps that are separated by an angle and that share a common pedicle (Fig. 12.12). It was originally described by Esser (24) and later revised by Zimany (93). It is designed to move more skin over a larger distance than is possible with a single lobe flap and it works well in regions in which skin mobility is limited (94). It has been described as using the Robin Hood principle of borrowing from the rich laxity of a neighboring area and transposing it to a relatively poor area of inelastic skin (88). This flap has been used to close defects on the plantar aspect of the foot (10,68,81,93), where it is recommended for defects 1 to 3 cm in diameter (81).
Figure 12.10 A preoperative picture of a mucoid digital cyst (A), followed by a circular excision (B) and closure by a single lobe local flap (C–E).
The bilobed flap is very versatile and can be adapted for closure of defects throughout the foot. Its uses include closure of excisions for digital cysts, metatarsal head ulcerations, osteomyelitis, and plantar rearfoot ulcerations and heel defects (Fig. 12.13). Bilobed flap technique and arthroplastic resection is useful for excision of digital mucoid cysts. The use of bilobed flap allows for greater exposure than the traditional semielliptical incisions while it also permits the wide excisional defects to be closed primarily with no recurrence, flap failures, or other major complications as it was shown in a retrospective study of 15 patients with an average follow-up of 4.6 years (52).
Figure 12.11 A preoperative picture of a heel ulcer (A), excised as an oval defect (B) and closure by a single lobe local flap (C–E).
Since two flaps are used, two adjacent donor sites are needed to close the defect. The first lobe closes the original defect, whereas the second lobe closes the first flap donor site. The second flap donor site is then closed primarily. Typically the lobes are designed to be 90 degrees from the defect and from each other, although this is not a necessity (30–46,64–68) and the angles may vary from 45 to 90 degrees (93). On the plantar aspect of the foot, it is recommended that the angles be no greater than 60 degrees (81). The first lobe can be up to 20% smaller than the defect, and the second lobe can be up to 20% smaller than the first lobe (88). Some authors (1,3–46,64–71,95,107) feel that the lobes can be up to half the size of the defect they close. A general rule for lobe creation includes the following parameters. The first lobe can be 75% of the width of the original defect, whereas the second lobe is 50% of the original defect. The rotating base should be the only area undermined (23), although some authors recommend wide undermining (88,94). Some authors have found it easier and quicker to suture the second lobe into the defect caused by the first lobe and then suture the first lobe into the original defect (99). The two apices should actually be closed first, followed by the circumferential sutures along the lobes.
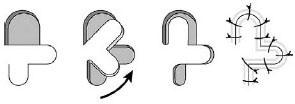
Figure 12.12 The bilobed flap consists of two flaps that are separated by an angle and that share a common pedicle.
An improvement in the design of bilobed flaps consists of rotating each lobe only 45 degrees, including a Burrow’s triangle in the original design of the flap, and extending the length of the second lobe (94). This results in a reduction of dog-ear formation, pincushioning, and distortion (94). A trilobed flap has been described (35) to reduce the dog ear often obtained with a bilobed flap, but at the expense of an enlarged incision.
The advantage of the bilobed flap is the ability to recruit large amounts of tissue by borrowing from different areas and opposing directions. The disadvantages are the length and varying directions of the incisions required (42). A modified bilobed flap is useful for areas in which skin laxity is less. A modified bilobed flap from mastoid and lateral neck skin for reconstruction of complex defects of the posteromedial surface of the auricle and mastoid skin is described, with the preservation of the retroauricular sulcus and closure of the donor site. Scars were hidden along minimal tension lines and the possibilities of wearing spectacles along with sensitivity all over the reconstructed area were maintained (112).
Figure 12.13 A bilobed flap designed on the dorsal aspect of the foot (A), followed by a circular excision of the lesion (B) and final closure (C–E).
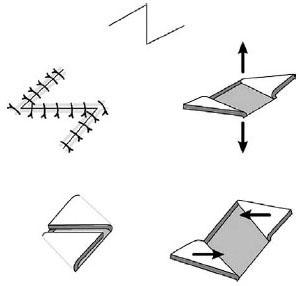
Z-PLASTY
With the Z-plasty, two triangular flaps are transposed, using a Z-shaped incision. The Z-plasty is a useful technique for lengthening a linear scar contracture, dispersal of a scar by breaking up the scar, realigning a scar within the LME (67), and web space widening and construction (44). Z-plasties have many adaptations for foot surgery. They can be useful for correction of congenital fifth toe contractures, congenital overriding of the fifth toe, revisional bunion surgeries, and reconstruction of burn scar contractures to the dorsal and plantar regions of the foot (113). Also, a Z-plasty can be used to prevent a scar contraction, when an elective incision will cross a flexion crease (44), such as over the metatarsal phalangeal joints or over the joints on the digits. In addition, it can be used in conjunction with other flaps to improve cosmesis or flap movement (36).
Z-plasty should only be considered if there is sufficient skin laxity in the direction opposite to the direction of skin to be lengthened. Once it has been determined to use a Z-plasty, certain design parameters such as length of incisions and angles between incisions must be determined. Given the design of the Z-plasty, the amount of length that will be gained is determined by both the lengths of the incisions and the angle between the incisions (Figs. 12.14 and 12.15). Because length is gained at the expense of width, the longer the three incisions are, the more the scar can be lengthened; however, this results in a narrower width with increased tension (44). Theoretically, the amount of length gained is equal to the length of the center diagonal incision minus the length of an imaginary line connecting the other two incisions. Similarly, the closer to 90 degrees the angles are, the more the length will be increased. Ninety-degree advancing tip angles, however, generally result in dog ears at the bases. When angles are too acute, the advancing tips may have compromised blood supply and may become ischemic. A 75-degree angle may theoretically result in 100% increase in length; however, it will also result in too large of a lateral tension on the flaps and will likely cause a failure of the flaps (16). A 30-degree angle will only result in a theoretical 25% increase in length and will not provide a sufficient amount of tension release (16). In general, angles between 45 and 60 degrees work best (44).
Figure 12.14 The Z-plasty with two triangular flaps being transposed by using a Z-shaped incision. The Z-plasty is a useful technique for lengthening a linear scar contracture and realigning a scar within the LME.
Some authors feel that it is more advantageous to use one large Z-plasty as compared with multiple smaller Z-plasties (Fig. 12.16), given the fact that larger Z-plasties have larger flaps that typically have better blood supply (44); other authors believe that multiple Z-plasties are preferred (67). In the digits, larger Z-plasties may constrict the digit horizontally and compromise the blood flow into the digit. In the digits, it is better to use multiple Z-plasties (44).

Figure 12.15 A Z-plasty is shown over a contracted second digit (A), followed by transposition of the flaps (B) and arthrodesis of the proximal interphalangeal joint (C,D).
Figure 12.16 A schematic diagram showing a large Z-plasty compared with multiple smaller Z-plasties.
The initial incision, which will become the diagonal line of the Z, is made longitudinally along the length of the scar or along the direction to be lengthened. The other two incisions are then made off this central line at 45- to 60-degree angles and should parallel the RSTL. The three limbs of the Z-shaped incision should be of equal length. If the three incisions are not made of equal length, then puckering will occur (67). The incisions may be made of unequal length; however, if the skin on one side of the central incision is elastic and loose then the skin on the other side of the central incision is constricted (67). The flaps should be fully elevated to slightly beyond their bases to allow for ease of rotation (36); however, care must be taken to avoid undermining the tip of the flaps. An imaginary line connecting the two noncentral incisions becomes the new central line or diagonal of the final Z after the flaps have been transposed. If the surrounding skin is extremely taut, then a smaller angle, such as 45 degrees, and a longer central incision should be used (16). By curving the top and bottom incisions of the Z-flap away from the diagonal incision, extra tissue can be included in the flap base that may help to increase flap vascularity (Fig. 12.17). (36).
A critical stitch or suture should first be placed in the midpoint of the new central arm, followed by other sutures at the base of the flaps. Apical sutures should be used at the tips of the flaps. Oblique sutures should be used to advance the tip of each Z-flap. If there is excess tension across the central limb of the final Z, then a mini Z-plasty can be performed along that limb (85). The technique involves incising two lines that are parallel to the outer limbs of the larger Z, less than half the length of the larger limbs, and are carried out just through to the dermal layer. The central limb of the mini-Z is contained within the central one third of the central limb of the larger Z. It is especially useful if the initial Z-plasty design was slightly larger than appropriate and can therefore repair problems that result from poor planning (85).
A Z-plasty is preferred over the W-plasty when there is either too much or too little skin tension (1,9–46,64–67). In comparison with the W-plasty, the Z-plasty uses all the available skin without increasing the overall tension in the area (9). The limbs are larger on the Z-plasty, however, and could lead to more visible scarring (9). A Z-plasty should not be used if the scar does not cross the RSTL (67).

Figure 12.17 A radiographic (A) and clinical picture (B) of the resected distal first metatarsal caused by osteomyelitis. Multiple small Z-plasties (C) for wound closure after the insertion of bone grafting with internal fixation at the first ray (D–F). A final clinical postoperative outcome (G).
Figure 12.17 (Continued)
DOUBLE-Z RHOMBOID FLAP
The double-Z rhomboid flap uses the technique of two Z-plasties to correct a rhomboid-shaped defect. It may be used to create a non-weight bearing incision because of the transposition of the two Z-flaps. Double-Z rhomboid flaps can be used for fifth metatarsal head pathologies, in addition to a variety of plantar forefoot and rearfoot conditions (Fig. 12.18).
The double-Z rhomboid flap was originally described as a rhomboid-to-W flap (6). The flap was later designed so that its long diagonal was parallel to the RSTL (17,18). This, however, was later redesigned (37). The recommended technique is to draw two parallel lines in the direction of the RSTL that will enclose the defect. Then a second set of parallel lines are drawn to complete a 60- and 120-degree rhombus. Two Z-plasties are then drawn on opposing sides of the rhombus, such that their central lines are continuations of the original two parallel lines of the rhombus. The flaps are then transposed in a similar fashion as a Z-plasty, resulting in an incision shaped like two Zs end-to-end.
DOUBLE OPPOSING Z-PLASTY
A double opposing Z-plasty, which is very similar to the five-flap Z-plasty (34), can be used when the anatomy or vascularity of the area does not permit the use of a large single Z-plasty and is as effective as the single Z-plasty in release of a scar contracture (67).
Two Z-plasties are designed so that their central incision or diagonal stem of the Z are along the same line. The two Z-plasties are then created such that one Z is backward and one is forward, in relation to each other. The flaps are then elevated and transposed in a manner similar to single Z-plasties. To facilitate closure, the double opposing Z-plasty may be converted to a five-flap Z-plasty by creating an additional incision to bisect the largest flap.
Double opposing Z-plasty is useful for syndactyly release, operating on only one side of the finger at any particular time to prevent ischemic compromise to the finger should one of the digital vessels be absent or be injured. The surgical division is individually tailored based on complexity and location of the syndactyly. Generally, the release is accomplished by dividing the fingers and resurfacing the surgical wound with a well-vascularized dorsal trapezoidal shaped flap, interdigitating fasciocutaneous flaps, and full-thickness skin grafts to resurface interdigital space. If the fingernail is involved, divide it longitudinally. Osteotomize and cover any bony exposure with local fasciocutaneous flaps for stable coverage. It is important that the local interdigitating flaps be designed well to minimize the need for skin grafts (114).
DOUBLE OPPOSING V-Y-Z PLASTY
This technique is a combination of V-Y plasty with Z-plasty in double opposing fashion, both ensuring primary donor site closure. The technique was applied to 21 postburn scar contractures in 14 patients. All flaps healed uneventfully with adequate lengthening and functional recovery was achieved in all cases. Double opposing V-Y-Z plasty, as a good alternative to multiple Z-plasties and multiple rhomboid flaps, is a very useful technique to ensure more lengthening and prevent recurrence in the treatment of serious postburn scar contractures (63).
FOUR-FLAP Z-PLASTY
To obtain maximal lengthening of a scar, a four-flap Z-plasty can be used (36-46,64–67). It consists of designing a wide-angled Z-plasty and then dividing the two triangle flaps into four triangle flaps. The flaps are then elevated and transposed so that they lie in alternating fashion, in between each other. Other multiple Z-plasty flaps have been described, such as a five-flap (34) and a six-flap (101), and have been found useful for correcting web contractures between fingers.
DOUBLE OPPOSING SEMICIRCULAR FLAP
The double opposing semicircular flap is a variation of the Z-plasty and can be used for the closure of large circular defects in the range of 2 to 5 cm in diameter (39). Two different versions of this theory exist.
The first version was described by Golomb (27). In his version, two semicircles are incised on opposing sides of a circular defect. One of the semicircles is bisected. The flap formed by half of the bisected semicircle is transposed into the adjacent half of the circular defect. The same procedure is followed for the opposing side.
A later version by Keser (39) involves bisecting the circular defect with a line that is inclined 45 degrees from the RSTL. Then two tangents are drawn on opposite sides of the circular defect, parallel to the RSTL. The distance from the point at that one of the tangents and the bisector intersect, to the point at that the bisector intersects the opposite side of the circle, is noted. With the use of calipers, the same distance is then marked on the opposite end of that tangent. The same procedure is carried out for the other tangent. From the points of intersection of the tangents to the circular defect, a line is drawn perpendicular to the tangents, of a length equal to the radius of the circle. A curve is then drawn from the distant aspect of the tangent line to the distant aspect of the line perpendicular to the tangent. This curve should have the same radius as the circular defect. An identical but opposite curve should be drawn on the opposite side of the defect. The semicircular flaps are then elevated and transposed into the circular defect. The advantage of this flap is that it achieves closure of the defect without excision of additional tissue and without alteration of the shape of the circular defect; the flaps fit perfectly into the defect and do not require trimming, and three of the five suture lines follow the RSTL (39).
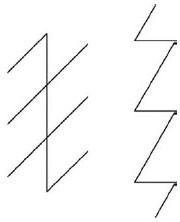
W-PLASTY
Similar to the Z-plasty, the W-plasty can also be used to break up a scar into smaller components. Since it involves excising the scar tissue, it has the disadvantage of increasing the tension in the area of a scar secondary to the removal of tissue (9,67). It should be employed in areas with sufficient tissue and elasticity. The W-plasty produces a zigzag scar and is simpler than using multiple Z-plasties. The amount of lengthening that occurs, however, is minimal (36).
Figure 12.18 A double-Z rhomboid flap (A) uses the technique of two Z-plasties to correct a rhomboid-shaped defect (B). It may be used to create a non–weight bearing incision because of the transposition of the two Z-flaps (C,D).
Two zigzag patterns are designed along the length of the scar, one on each side of the scar. As with a Z-plasty, the optimum angle between incisions should be 55 to 60 degrees (67). It is recommended that at the end of the W-plasty, the triangles be designed smaller in size, with a tapering of the length of the limbs of the W-plasty (67). Once one incision is made along one side of the scar, the other opposing incision is made so that the tip of one triangle on one side corresponds to the midpoint of the base of a triangle on the opposing side. The piece of skin containing the scar is then excised. On a curved scar, the angles of the triangles on the inner incision should be more acute than the angles of the triangles on the outer aspect of the curve.
A continuous subcuticular suture should be used to approximate the triangles between the two zigzag incisions and should be placed halfway between the apex and the base of each triangle (67). Additional approximation can then be obtained using interrupted sutures.
RHOMBOID OR LIMBERG FLAP
The rhomboid or Limberg flap (Fig. 12.19) is typically used to close a rhomboid-shaped defect, but may be used to close circular defects (30,43). A flap of exactly the same shape and size as the defect is raised and transposed 60 degrees into the defect. Although the flap covers the original defect 100%, it only closes half of the total defect; the remaining defect is closed primarily (11). The flap redistributes and redirects tension from the donor site to the recipient site, in 90 degrees (Fig. 12.20) (30).
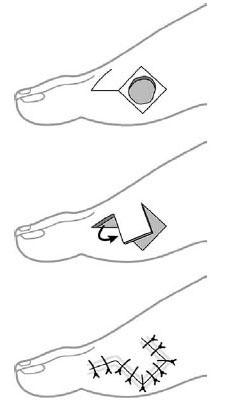
Figure 12.19 The rhomboid or Limberg flap is typically used to close a rhomboid-shaped defect, but may be used to close circular defects. A flap of exactly the same shape and size as the defect, is raised and transposed 60 degrees into the defect. Although the flap covers the original defect 100%, it only closes half of the total defect; the remaining defect is closed primarily.
The rhomboid flap is one of the most versatile adjuncts for closure of foot wounds and pedal defects. It can be used for correction of isolated metatarsal head lesions, with simultaneous exposure for osseous corrections, such as a condylectomy, osteotomy, or metatarsal head resection. Rhomboid flaps may also be used to correct a plantar lesion. It has been adapted for dorsal lesions of the foot (4), although greater mobility is required for primary closure. Desyndactylization procedures can also employ a rhomboid flap in the foot for plantar closure (75) or in the hand (45).
Two parallel lines are drawn in the same direction as the LME or perpendicular to the RSTL. These are drawn tangential to the defect. Two additional lines are drawn that complete the design of an equilateral parallelogram or rhombus with 60-and 120-degree angles. Four possible rhomboid flaps can then be drawn (Fig. 12.21). Two of these possible rhomboid flaps will have their short axis parallel to the LME. In closing the donor site, choosing either of these two will result in the area of greatest tension to occur in the same direction as the LME (7,8,12,41,45). If the short axis of the flap is perpendicular to the LME, the design will result in immobile flaps (19). By using the pinch test to determine the orientation of the LME, the best flap for transposition can be chosen. Anatomic constraints or surgeon preference will result in the optimum choice from the two final possibilities.
An alternative way of viewing the design of a rhomboid flap is to first excise the lesion in the shape of a rhombus so that two of the sides are parallel to the LME. Next, extend the short diagonal of the rhombus, in either direction, by the same length as the sides of the rhombus. The final side of the flap is designed at a 60-degree angle to the end of the extended short diagonal and equal to the length of the sides of the rhombus. Once again, the short axis of the flap must lie parallel to the LME.
Although the complex geometry must be understood, it does not need to be strictly adhered to obtain satisfactory clinical results (11). Although the rhomboid flap was designed for use in areas in which skin extensibility is significant, the flaps may be used in regions of tense skin (95). In such cases, the entire area must be undermined, including the margins of the rhomboid defect and the base of the flap. Undermining of the donor site can be successfully achieved without compromising the surrounding subcutaneous perforators. Mobility can be increased with concomitant bone resection.
A major advantage of the rhomboid flap is that the surgeon can choose the ideal flap from four possibilities. Another advantage is that once the length of one of the sides of the rhomboid is determined, all other incisions are the same length and calipers can be used to facilitate the design (45). One disadvantage of the rhomboid flap is that in younger patients or when the skin is dense and thick, cosmetically significant bulges or dog ears may occur (104).
FLAP OF DUFOURMENTEL
The flap of Dufourmentel can be used for rhombic defects of any acute angle, not just those of 60 and 120 degrees (11). Although more difficult than the classic Limberg flap, it is especially useful for rhombic defects with an acute angle of 60 to 90 degrees (11,41–45), or when excision of additional skin to create a more acute angle is undesirable (41). If the acute angle is 60 degrees, then the flap becomes wider than the primary defect and the use of the flap is not advantageous (45).
Figure 12.20 A rhomboid or Limberg flap is typically used to close a rhomboid-shaped defect (A). Resection of the prominent bony prominence might be necessary in certain cases (B). Flap closure (C) and final clinical outcome (D).
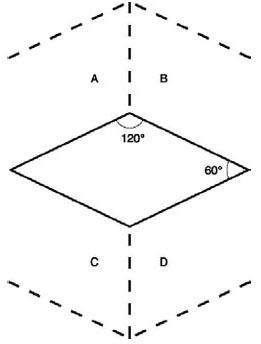
Figure 12.21 The versatility of the rhomboid flap is shown on this schematic diagram. Two parallel lines are drawn in the same direction as the LME or perpendicular to the RSTL. These are drawn tangential to the defect. Two additional lines are drawn that complete the design of an equilateral parallelogram or rhombus with 60- and 120-degree angles. Then four possible rhomboid flaps can be drawn and used to close the primary defect.
First the defect is excised in the shape of a rhombus or an equilateral parallelogram. The short diagonal of the rhombus is extended from the tip of one of the less acute sides. From that same point, one of the sides of the defect is also extended. The angle formed by these two lines is then bisected by a line equal in length to the sides of the rhombus and the corresponding line forms one of the sides of the flap. The final side of the flap is incised equal in length to all the other sides of the rhombus, but parallel to the long axis of the defect. Once again, as with the Limberg flap, the use of calipers may facilitate the design, although the addition of a protractor may also be helpful (45).
Some authors (8) feel that since the flap of Dufourmentel does not take advantage of the LME to the extent that the Limberg flap does, then it is not as useful as the Limberg flap; however, this had been discounted previously (45).
THIRTY-DEGREE TRANSPOSITION FLAP
A variation of the rhomboid flap, the 30-degree transposition flap contains a 30-degree angle at the distal end of the typical rhomboid flap. It was found that a 30-degree angulation will not cause cosmetically significant bulges that plague the typical rhomboid flap (104). Since one drawback of using a 30-degree distal angle is a significantly increased incision length, the 30-degree angle is typically combined with an M-plasty, which shortens the rhomboid shape.
The distal end of the flap is designed parallel to the RSTL. The final edge of the flap is at a 30-degree angle to the distal end of the flap. The flap is transposed in a similar fashion to the rhomboid flap. The sides of the M-plasty are advanced into the side of the defect. Although more difficult than the classic Limberg flap, it has the advantages of dispersing tension more evenly around the flap (41), thereby closing with less tension.
DOUBLE OR TRIPLE RHOMBOID
Double or triple rhomboid flaps are useful in the closure of large rectangular or circular defects (41). Double rhomboid flaps may be used to close a 60-degree parallelogram with a 2:1 length to width ratio (1,12–42). Given the fact that a 2:1 parallelogram is actually two 60-degree rhombi, the closure with the use of double rhomboid flaps can be visualized easily. Triple rhomboid flaps may be used to close a larger defect, if the defect can be designed as a hexagon, or three 60-degree rhombi (45). The calipers are set to the length of the radius of the defect. The flaps should all have their limbs pointing in the same direction. Only in special circumstances should two of the flaps share a common base because in that instance, when they are rotated, a 120-degree angle is closed. This will likely cause a pronounced and probably permanent dog ear.
NOTE FLAP
Walike and Larrabee (115) designed this flap, which allows for closure of a circular defect with a triangular flap that maximizes use of surrounding tissues (41). A tangent is drawn on either side of a circular defect, parallel to the RSTL. The tangent should be approximately one and a half times the diameter of the circle. At the end of the tangent, a 50- to 60-degree flap is designed, having a length approximately equal to the diameter of the circle. The flap is then transposed into the circular defect and the tip is trimmed or de-epithelialized. The major movement is perpendicular to the tangent (41). Because the flap is approximately two thirds the size of the defect, clinical judgment is required when using the flap (41). The flap is recommended for smaller defects, 2 cm or less (41). The small dog ear that is created usually resolves, but may be revised at the time of the procedure (41).
CONCLUSION
Local flap reconstruction of pedal defects can be accomplished with a variety of techniques. Multiple geometric constructs have been described for closure of foot defects. Each has its own unique principles that can be adapted to certain locations and premorbid conditions. Local flaps considered for closure of foot defects should lie within the higher level of any algorithm, because of their versatility, reproducibility, and long-term functional outcomes. In addition, hospitalization, length of anesthesia, and perioperative care can be much less with the use of local flaps.
REFERENCES
- Gillies H, Millard DR Jr. In: Gillies HD, Millard DR Jr. eds. The principles and art of plastic surgery. Boston: Little, Brown, 1957:5.
- Stedman’s medical dictionary, 26th ed. Baltimore: Lippincott Williams & Wilkins, 1995:660.
- Attinger C. Soft-tissue coverage for lower-extremity trauma. Orthop Clin North Am 1995;26(2):295–334.
- Attinger CE. Use of soft tissue techniques for salvage of the diabetic foot. In: Kominsky S, ed. Medical and surgical management of the diabetic foot. St. Louis: Mosby, 1994:323–366.
- Attinger C, Cooper P, Blume P. Vascular anatomy of the foot and ankle. In: Jurkiewicz MJ, Culbertson JH, eds. Operative techniques in plastic and reconstructive surgery. Los Angeles: General Publishing Group, 1996:183–198.
- Becker H. The rhomboid-to-W technique for excision of some skin lesions and closure. Plast Reconstr Surg 1979;64(4):444–447.
- Borges AF. Choosing the correct Limberg Flap. Plast Reconstr Surg 1978;62(4):542–545.
- Borges AF. The rhombic flap. Plast Reconstr Surg 1981;67(4):458–466.
- Borges AF. The W-plastic versus the Z-plastic scar revision. Plast Reconstr Surg 196944(1):58–62.
- Bouché RT, Christensen JC, Hale DS. Unilobed and bilobed skin flaps. Detailed surgical technique for plantar lesions. J Am Podiatr Med Assoc 1995;85(1):41–48.
- Bray DA. Clinical applications of the rhomboid flap. Arch Otolaryngol 1983;109:37–42.
- Brobyn TJ, Cramer LM, Hulnick SJ. Facial resurfacing with the Limberg Flap. Clin Plast Surg 1976;3(3):481–490.
- Callegari PR, Taylor GI, Caddy CM, et al. An anatomic review of the delay phenomenon: I. Experimental studies. Plast Reconstr Surg 1992;89(3): 397–407.
- Chang TJ, Stanifer EG, Jimenez AL. Plastic repair techniques: skin plasties and local flaps. In: Tucker GA, ed. Reconstructive surgery of the foot and leg ’93. Tucker, GA: Podiatry Institute Publishing, 1993:52–65.
- Colen LB, Replogle SL, Mathes SJ. The V-Y planter flap for reconstruction of the forefoot. Plast Reconstr Surg 1988;81(2):220–228.
- Crawford ME, Dockery GL. Use of Z-skin plasty in scar revisions and skin contractures of the lower extremity. J Am Podiatr Med Assoc 1995;85(1):28–35.
- Cuono CB. Double Z-plasty repair of large and small rhombic defects: the double-Z rhomboid. Plast Reconstr Surg 1983;71(5):658–667.
- Cuono CB. Double Z-rhombic repair of both large and small defects of the upper extremity. J Hand Surg 1984;9(2):197–202.
- Daniel RK, Kerrigan CL. Principles and physiology of skin flap surgery. In: Plastic surgery. McCarthy JG, ed. Philadelphia: Saunders, 1990:275–328
- Dayton PD, Griffiths T. Biwinged excision for round pedal lesions. J Foot Ankle Surg 1996;35(3):244–249.
- Dockery GL, Christensen JC. Principles and descriptions of design of skin flaps for use on the lower extremity. Clin Podiatr Med Surg 1986;3(3):563–577.
- Dockery GL. Single-lobe rotation flaps. J Am Podiatr Med Assoc 1995;85(1):36–40.
- Elliot RA. Rotation flaps of the nose. Plast Reconstr Surg 1969;44(2):147–149.
- Esser JFS. Gestielte lokale Nasenplastik mit Zweizipfligem lappen Deckung des Sekundaren Detektes vom ersten Zipfel durch den Zweiten. Dtsch Z Chirurgie 1918;143:385.
- Fleetwood FR, Barret SL, Day SV. The burrow advancement flap for closure of plantar defects. J Am Podiatr Med Assoc 1987;77(5)246–249.
- Gidumal R, Carl A, Evanski P, et al. Functional evaluation of nonsensate free flap to the sole of the foot. Foot Ankle 1986;7(2):118–123.
- Golomb FM. Closure of the circular defect with double rotation flaps and Z-plasties. Plast Reconstr Surg 1984;76(4):813–816.
- Hale DS, Dockery GL. Giant keratoacanthoma of the planter foot: a report of two cases. J Foot Ankle Surg 1993;32(1):75–84.
- Heinz TR. Local flaps for hindfoot reconstruction. In: Jurkiewicz MJ, Culbertson JH, eds. Operative techniques in plastic and reconstructive surgery. Los Angeles: General Publishing Group, 1996:157–164.
- Heniford BW, Bilin PL, Marsico RE Jr. Field guide to local flaps. Dermatol Clin 1998;16(1):65–74.
- Hidalgo DA, Shaw WW. Anatomic basis of plantar flap design. Plast Reconstr Surg 1986;78(5):627–636.
- Hirshowitz F, Kaufman T, Amir I. Biwinged excision for closure of rounded defect. Ann Plastic Surg 1980;5:372–380.
- Hirshowitz B, Mahler D. T-plasty technique for excisions in the face. Plast Reconstr Surg 1966;37(5):453–458.
- Hirshowitz B, Karev A, Levy Y. A 5-flap procedure for axillary webs leaving the apex intact. Br J Plast Surg 1977;30:48–51.
- Iida N, Ohsumi N, Sakai M. A trilobed flap for reconstruction of nasal skin defects. Plast Reconstr Surg 1997;100(4):991–995.
- Jackson IT. Local flaps in head and neck reconstruction. New York: Mosby, 1985:6–3.
- Katoh H, Nakajima T, Yoshimura Y. The double-Z rhomboid plasty: an improvement in design. Plast Reconstr Surg 1984;74(6):817–824.
- Kerrign CL. discussion of “An anatomic review of the delay phenomenon: I. Experimental studies” by Callegari and “An anatomic review of the delay phenomenon: II. clinical application” by Taylor. Plast Reconstr Surg 1992;89(3):417–418.
- Keser A, Sensoz O, Mengi AS. Double opposing semicircular flap: a modification of opposing Z-plasty for closing circular defects. Plast Reconstr Surg 1998;102(4):1001–1007.
- Kinsella JB, Rassekh CH, Wassmuth 2D, et al. Smoking increases facial skin flap complications. Ann Otol Rhinol Laryngol 1999;108:139–142.
- Larrabee WF Jr. Design of local skin flaps. Otol Clin North Am 1990;23(5):899–923.
- Larrabee WF. Bilobed flap reconstruction of the temporal forehead. Arch Otolaryngol Head Neck Surg 1992;117: 983–984.
- Lawrence WT. The nasolabial rhomboid flap. Ann Plast Surg 1992;29(3):269–273.
- Lesavoy MA. Local incisions and flap coverage. In: McCarthy JG, ed. Plastic surgery. Philadelphia: Saunders, 1990:4441–4458.
- Lister GD, Gibson T. Closure of rhomboid skin defects: the flaps of Limberg and Dufourmentel. Br J Plast Surg 1972;25:300–314.
- Lombardo M, Aquino JM. Local flaps for resurfacing foot defects: a vascular perspective. J Foot Surg 1982;21(4):302–304.
- Archer KA, Lembo T, Haber JA. Protein s deficiency and lower-extremity arterial thrombosis: complicating a common presentation. J AM Podiatr Med Assoc 2007; 97(2):151–155.
- Sumpio BE, Paszkowiak JJ, Blume PA. Vascular ulcers. In: Creager J, Olin J, eds. Vascular medicine, St. Louis: Mosby, 2006:880–893.
- Frykberg RG, Zgonis T, Armstrong DG, et al. Diabetic foot disorders: a clinical practical guideline. J Foot Ankle Surg 2006;45(5): S1–S66.
- Sumpio BE, Schroeder SM, Blume PA. Etiology and management of foot ulcerations. In: Lee BY. The wound management manual. New York: McGraw-Hill, 2005:126–133.
- Price NM. Closure of surgical wounds using contiguous island flaps (double V to Y procedure). Ann Plast Surg 1979;3(4):321–325.
- Blume PA, Moore JC, Novicki DC. Digital mucoid cyst excision by using the bilobed flap technique and arthroplastic resection. J Foot Ankle Surg 2005;44(1):44–48.
- Hanft JR, Blume PA, Dardik P, et al. A pilot clinical study for the treatment of diabetic foot ulcers with an injectable bioactive co-polymer (abstract). Presented at: Symposium on Advanced Wound Care and the 15th Annual Medical Research Forum on Wound Repair; April 2005; San Diego, CA.
- Attinger C, Bulan EJ, Blume PA. Pharmacological and mechanical management of wounds. In: Mathes SJ. Plastic surgery, vol 1. St. Louis: Elsevier, 2006:863–899.
- Nishimura K, Blume P, Ohgi S, Sumpio BE. The effect of different regimen stretch on human dermal fibroblasts. J Surg Res 2006;130(2):331–332.
- Sumpio BE, Paszkowiak J, Aruny J, Blume PA. Lower extremity ulceration. In: Creager MA, Dzau VJ, Loscalzo J, eds. Vascular medicine, a companion to Braunwald’s heart disease. Philadelphia: Saunders, 2006;880–893.
- Attinger CE, Bulan EJ. Débridement: the key initial first step in wound healing Foot Ankle Clin 2001;6(4):627–660.
- Attinger CE, Cooper PS, Blume PA, Bulan B. The safest surgical incisions and amputations applying the angiosome principles and using the Doppler to assess the arterial: arterial connections of the foot and ankle. Foot Ankle Clinics Soft Tiss Cover 2001;6(4):745–799.
- Sumpio BE, Blume PA. Contemporary management of foot ulcers. In: Pierce WH, Matsumura JS, Yao JST, eds. Trends in vascular surgery. Chicago: Precept Press, 2002:277–290.
- Alnaeb ME, Boutin A, Crabtree VP, et al. Assessment of lower extremity peripheral arterial disease using a novel automated optical device. Vasc Endovascular Surg 2007;41(6):522–527.
- Bosch E, Kreitner KF, Peirano MF, et al. Safety and efficacy of gadofosvesetenhanced MR angiography for evaluation of pedal arterial disease: multicenter comparative phase 3 study. AJR Am J Roentgenol 2008; 190(1): 179–186.
- Taylor GI, Palmer JH, McManamny D. The vascular territories of the body (angiosomes) and their clinical applications. In: McCarthy M, ed. Plastic surgery. Philadelphia: Saunders, 1990:329–378.
- Tan O, Atik B, Ergen D. A new method in the treatment of postburn scar contractures: double opposing V-Y-Z plasty. Burns 2006;32(4):499–503.
- Manson PN, Anthenelli RM, Im MJ, et al. The role of oxygen-free radicals in ischemic tissue injury in island skin flaps. Ann Surg 1983;198:87–90.
- Marcinko DE. Plastic surgery in podiatry (simplified illustrated techniques). J Foot Surg 1988;27(2):103–109.1
- Maruyama Y, Iwahira Y, Ebihara H. V-Y advancement flaps in the reconstruction of skin defects of the posterior heel ad ankle. Plast Reconstr Surg 1990;85(5):759–764.
- McCarthy JG. Introduction of plastic surgery. In: McCarthy M, ed. Plastic surgery. Philadelphia: Saunders, 1990:55–68.
- McGregor JC, Soutar DS. A critical assessment of the bilobed flap. Br J Plast Surg 1981;34:197–205.
- Milton SH. Pedicled skin-flaps: the fallacy of the length:width ratio. Br J Surg 1961;57:502–508.
- Morain WD, Dellon AL, MacKinnon SE, et al. Current concepts in plastic surgery for the diabetic. Adv Plast Reconstr Surg 1987;4:1–36.
- Morgan BL, Samiian MR. Advantages of the bilobed flap for closure of small defects of the face. Plast Reconstr Surg 1973;52(1):35–37.
- Morris SF, Taylor GI. Predicting the survival of experimental skin flaps with a knowledge of the vascular architecture. Plast Reconstr Surg 1993;92(7):1245–1251.
- Ono I, Gunji H, Sato M, et al. Use of the oblique island flap in excision of small facial tumors. Plast Reconstr Surg 1993;91(7):1245–1251.
- Palmer B, Jurell G, Norberg KA. The blood flow in experimental skin flaps in rats studied by means of the 133 xenon clearance method. Scand J Plast Reconstr Surg 1972;6:6–12.
- Park S, Eguchi T, Tokioka K, et al. Reconstruction of incomplete syndactyly of the toes using both dorsal and plantar flaps. Plast Reconstr Surg 1996;98(3):534–537.
- Parker JA, Searles JM. Local flaps for forefoot and midfoot reconstruction. In: Jurkiewicz MJ, Culbertson JH, eds. Operative techniques in plastic and reconstructive surgery. Los Angeles: General Publishing Group, 1996:148–156.
- Pribaz JJ, Chester CH, Barrall DT. The extended V-Y flap. Plast Reconstr Surg 1992;90(2):275–280.
- Pyka RA, Coventry MB. Avascular necrosis of the skin after operations on the foot. J Bone Joint Surg 1961;43:955–960.
- Rand-Luby L, Pommier RF, Willians ST, et al. Improved outcome of surgical flaps treated with topical dimethylsulfoxide. Ann Surg 1996;224(4):583–590.
- Rooks MD. Coverage problems of the foot and ankle. Orthop Clin North Am 1989;20(4):723–736.
- Sanchez-Conejo-Mir J, Bueno Montes J, Moreno Gimenez JC, et al. The bilobed flap in sole surgery. J Dermatol Surg Oncol 1985;11(9):913–917.
- Sarrafian SK. Anatomy of the foot and ankle, 2nd ed. Philadelphia: JB Lippincott, 1993:329.
- Satterfield VK, Jolly GP. A new method of excision of painful planter forefoot lesions using a rotation advancement flap. J Foot Ankle Surg 1994;33(2):129–134.
- Schredde J, Petrovici V. The use of slide-swing plasty in closing skin defects: a clinical study based on 1,308 cases. Plast Reconstr Surg 1981;67(4):467–481.
- Seyhan A. Mini Z in Z to relieve the tension on the transverse closure after Z-Plasty transposition. Plast Reconstr Surg 1998;101(6):1635–1637.
- Shaw WW, Hidalgo DA. Anatomic basis of plantar flap design: clinical applications. Plast Reconstr Surg 1986;78(5):637–649.
- Sherif MM. V-Y Dorsal metacarpal flap: a new technique for the correction of syndactyly without skin graft. Plast Reconstr Surg 1998;101(7):1862–1866.
- Sutton AE, Quatela VC. Bilobed flap reconstruction of the temporal forehead. Arch Otolaryngol Head Neck Surg 1992;118:978–982.
- Taylor GI, Corlett RJ, Caddy CM, et al. An anatomic review of the delay phenomenon. II. Clinical applications. Plast Reconstr Surg 1992;89(3):408–416.
- Attinger CE, Evans KK, Bulan E, et al. Angiosomes of the foot and ankle and clinical implications for limb salvage: reconstruction, incisions, and revascularization, Plast Reconstr Surg 2006;117(7 Suppl):261S–293S.
- Imanishi N, Kish K, Chang H, et al. Anatomical study of cutaneous venous flow of the sole. Plast Reconstr Surg 2007;120(7):1906–1910.
- Blume PA. A closer look at plastic surgery techniques: Q/A. Podiatry Today 2003;16:24–28, HMP communications.
- Barret JP, Herndon DN, McCauley RL. Use of previously burned skin as random cutaneous local flaps in pediatric burn reconstruction. Burns 2002;28(5):500–502.
- Huang SR, Li XY, Wang H, et al. The use of local flap in repairing deeply burned wound of extremities. [article in Chinese.] Zhonghua Wai Ke Za Zhi 2005;43(3):182–184.
- Ashbell TS. The rhomboid excision and Limberg flap reconstruction in difficult tense skin areas. Plast Reconstr Surg 1982;724.
- Blume PA, Paragas LK, Sumpio BE, Attinger CE. Single-stage surgical treatment of noninfected diabetic foot ulcers. Plast Reconstr Surg 2002;109(2):601–609.
- Zgonis T, Jolly GP, Blume PA. A guide to closure techniques for open wounds. Podiatry Today 2003;40–48, HMP communications.
- Sumpio BE, Blume PA. Treatment of foot ulcers. N Engl J Med 2001;344(2):correspondence.
- Aranmolate S, Attah AA. Bilobed flap in the release of postburn mentosternal contracture. Plast Reconstr Surg 1987;83(2):356–361.
- Lu F, Mizano H, Uysal CA, et al. Improved viability of random pattern skin flaps through the use of adipose-derived stem cells. Plast Reconstr Surg 2008;121(1):50–58.
- http://ejournals.ebsco.com/direct.aspPArticleID=4B07898BA5C10BA00897
- Armstrong DG, Lavery LA, Boulton AJ. Negative pressure wound therapy via vacuum-assisted closure following partial foot amputation: what is the role of wound chronicity? Int Wound J 2007;4(1):79–86.
- Blume PA, Walters J, Payne W, et al. Comparison of negative pressure wound therapy utilizing vacuum-assisted closure to advanced moist wound therapy in the treatment of diabetic foot ulcers: a multicenter randomized controlled trial. Diabetes Care 2008;31:631–636.
- Kouba DJ, Miller SJ. “Running pleated” suture technique opposes wound edges of unequal lengths. Dermatol Surg 2006;32(3):411–414.
- Asken S. A modified M-plasty. J Dermatol Surg Oncol 1986;12(4):369–373.
- Dockery G, Crawford M. Lower extremity soft tissue and cutaneous plastic surgery. Philadelphia: Saunders, 2006:76–133.
- Atasoy E, Ioakimidis E, Kasdan ML, et al. Reconstruction of the amputated finger tip with a triangular volar flap. J Bone Joint Surg Am 1970;52-A(5):921–926.
- Aoki R, Pennington DG, Hyakusoku H. Flap-in-flap method for enhancing the advancement of a V-Y flap. J Plast Reconstr Aesthet Surg 2006;59(6):653–657.
- Li JH, Xing X, Li P, Xu J. Transposition movement of V-Y flaps for facial reconstruction. J Plast Reconstr Aesthet Surg 2007;60(11):1244–1247.
- Askar I. Double reverse V-Y-plasty in postburn scar contractures: a new modification of V-Y-plasty. Burns 2003;29(7):721–725.
- Sheridan AT, Humzah D. V-Y-S-plasty closure of circular defects. Aust J Dermatol 2000;41(4):260–261.
- D’Arpa S, Cordova A, Moschella F. Further application of the bilobed flap: the split bilobed flap for reconstruction of composite posterior auricular and mastoid defects. J Plast Reconstr Aesthet Surg 2006;59(12):1330–1335.
- Thordarson DB. Congenital crossover fifth toe correction with soft tissue release and cutaneous Z-plasty. Foot Ankle Int 2001;22(6):511–512.
- http://www.emedicine.com/orthoped/TOPIC563.HTM
- Walike JW, Larrabee WF. The “note flap.” Arch Otolaryngol 1985;111(7):430–433.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree