Fig. 20.1
a Patient following right wide local excision and centralization of the nipple areola complex for invasive ductal carcinoma and radiotherapy. Evident lack of volume with scar retraction and contour deformity. b Patient following lipomodelling for symmetrization (result at 1 year after injection of 200 cc of purified fat)
The combination of an autologous LD flap and lipomodelling to augment the volume obviating the need for an implant is attractive for many patients, giving good consistency and a more natural and durable breast shape and reducing the incidence of implant-related complications or recurrences in the longer term [18, 19, 28, 33]. The latissimus dorsi flap is an ideal recipient site for fat grafting because of its excellent vascular network that can support large volumes of injected fat [34] with up to 500 ml of purified fat in a single sitting being possible. In a large single institution series, it was possible to achieve symmetry with the contralateral breast in 70% of patients. In those 30% where volume enhancement with fat grafting was insufficient, symmetry was achieved through contralateral mastopexy/reduction or insertion of a prosthesis on the reconstructed side [18, 19, 28] (◘ Fig. 20.2).
- 3.
Lipomodelling in Conjunction with Implant-based Reconstruction
Fig. 20.2
a Patient following right skin-sparing and left nipple-sparing mastectomy and immediate reconstruction with extended autologous LD flap. Evident asymmetry with left breast smaller than the contralateral one and with contour irregularities. b Patient following lipomodelling for symmetrisation (6 months after lipomodelling: 150 of purified fat injected in the right breast, 300 cc in the left breast)
Breast reconstruction with implants is associated with a number of potential problems. First, a defect in the cleavage area resulting in a visible step in the upper pole of the reconstructed breast and asymmetry of the cleavage area compared with the contralateral side. A second defect is frequently seen at the medial aspect of the breast characterized by a lack of filling and an excessively wide intermammary space. Finally there can be a lack of filling on the lateral aspect of the reconstructed breast immediately beneath the anterior axillary line. In addition there may be irregularities due to variable flap thickness and areas where implant coverage is thinned resulting in visible and palpable wrinkling. In the delayed reconstruction setting, especially when chest wall radiotherapy has been administered, the remaining skin may be of poor quality, scarred, lacking in elasticity and often with a thin layer of subcutaneous fat. Preemptive fat grafting may help to improve the quality of the flaps before or after definitive surgery. Fat transfer can be utilized to overcome these defects [24–26, 28, 35, 36]. In the upper medial pole of the cleavage area, fat is transferred mainly into the pectoralis major muscle. In the medial aspect of the breast (the intermammary area), fat should be transferred into the pectoralis muscle and between the skin and the periprosthetic capsule. The lateral defect can also be treated with an injection between the skin and the periprosthetic capsule. In these last two cases, an implant exchange is strongly recommended as inadvertent implant puncture is possible, especially in the presence of thin flaps. Smaller amounts of fat are generally required in these circumstances compared with autologous reconstructions, commonly involving volumes ranging from 50 to 150 cm3 of purified fat (◘ Fig. 20.3).
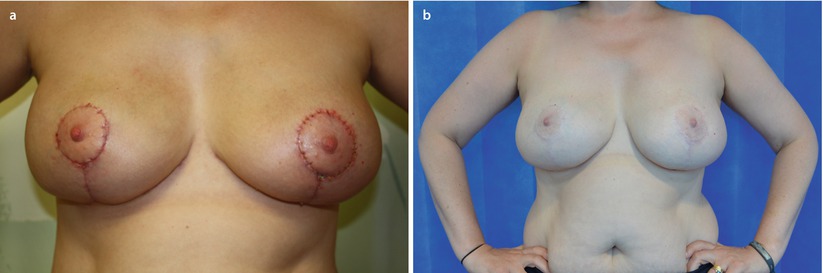
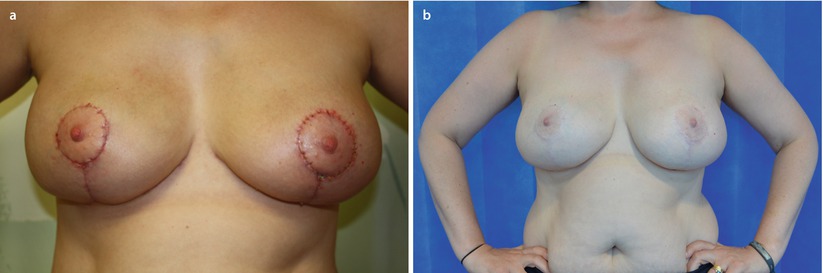
Fig. 20.3
a Patient following bilateral nipple-sparing, skin-reducing and risk-reducing mastectomy and reconstruction with expander implants. Lack of volume is visible in the cleavage bilaterally. b Patient following bilateral lipomodelling (2 sessions of lipomodelling required with a total of 380 cc of purified fat injected in the cleavage area and around the implants each side)
Tissue quality must be carefully assessed as it is often inferior to autologous reconstructions. The recipient sites should not be saturated to ensure the best possible graft survival. The aesthetic results are usually very good and improve the cosmetic outcome compared to use of an implant alone. In addition, pericapsular fat injection may reduce the capsular contracture rate, which has been shown in animal models [37], but further clinical studies are needed to support this use.
- 4.
Breast Reconstruction with Lipomodelling Alone
The idea of reconstructing an entire breast mound with exclusive use of fat transfer [38, 39] is surgically challenging. This technique is only applicable to a select number of cases, and specifically three main conditions must be met. The patient’s contralateral breast should be of small to moderate volume. The chest wall tissues at the mastectomy site have to be of good quality (in terms of thickness of the subcutis and muscle layers and their suppleness), and, finally, the patient must possess donor sites with plentiful excess of fat to allow for multiple harvest and transfer procedures. If all these criteria are fulfilled, then the patient can be considered for this technique and should be informed of the multiple-stage nature of this reconstruction and the fact that the breast mound may not be fully restored for some considerable time. Based on these limitations, few women elect to have this type of reconstruction when it is offered [39] (◘ Fig. 20.4).
Fig. 20.4
a Patient awaiting right breast reconstruction exclusively with lipomodelling. b Patient following right breast reconstruction exclusively with lipomodelling (four sessions of lipomodelling required, with a total of 756 cc of purified fat injected) and left mastopexy reduction for symmetrisation
The principles of fat harvesting, fat processing by centrifugation and the injection technique are similar to those described for general lipomodelling.
There are two main scenarios for an exclusive lipomodelling reconstruction:
The first case is a delayed breast reconstruction where part of the upper abdominal skin is used to perform an abdominal advancement flap to increase the volume of the recipient site and restore the breast footprint (the inframammary and lateral folds in particular) (see ► Chaps. 31 and 30, for more details).
A second, less common, scenario is the exclusive use of lipomodelling in immediate breast reconstruction after skin-sparing mastectomy where the skin envelope is preserved, thereby improving the shape of the reconstructed breast. In all cases fat is transferred into the pectoralis major muscle and the subcutis of the cleavage area. The skin envelope or the abdominal advancement flap is quilted onto the pectoralis muscle to accelerate tissue adhesion. Subsequent lipomodelling sessions are planned to restore the full breast mound observing a minimum interval of 4 months between sessions. The mean number of surgical procedures required is three (range 1–5) and is usually carried out in a day case setting. It is crucial to accurately assess the potential volume of fat available and properly manage the donor site. Overestimation of available fat donor sites could compromise the final reconstructed breast volume and prompt conversion from autologous to implant reconstruction.
Retrospective analysis suggests that the transferred fat volume needs to be about twice the amount necessary when compared with combined reconstruction with a latissimus dorsi flap for obtaining the same degree of breast volume enhancement. The possible explanation for this significant difference is the lack of a mechanical and vascular scaffold, which is conferred by the latissimus dorsi flap [39].
20.5 Complications of Fat Grafting
20.5.1 Complications
Common donor and recipient site complications include pain bruising, haematoma and swelling, excessive loss of volume, infection, fat necrosis, calcifications and oil cyst formation [8, 25–28, 40].
Pain
Significant pain relief can be achieved in the first 10 h by using postoperative infiltration of local anaesthetic. In the first postoperative day pain can be managed with analgesics like paracetamol and dihydrocodeine. Acute pain may last for about 48 h, and then only hypersensitivity or a dull ache can persist for a period of 1–3 months. In the longer term, a small percentage of patients may experience longer-term or even chronic pain, and patients must be warned about this at the time of consent.
Bruising and Oedema
Bruising at the donor site may take 2–3 weeks to resolve, while oedematous changes usually takes a month to resolve but may persist for longer if harvesting was overly aggressive or previous scarring and lymphatic drainage was compromised or infection develops. This may benefit from compression garments which provide both symptomatic support and reduce oedema, bruising and aid contouring [16].
Volume loss at the recipient site is an important issue. Injectate volume generally decreases by about 30%, although this rate can be as high as 40–50% depending on tissue quality at the recipient site, the quality of the injectate (generally better quality fat is harvested from those who are not very obese as the adipocytes are less fragile) and the volume of liquid in the injectate (e.g. poor centrifugation). The rate of reabsorption is lower for subsequent fat transfers as the quality and thickness of the tissues improve with every procedure and stabilizes over a period of 3–4 months.
Other Complications
Rarer complications include hypertrophic scarring, altered sensations, under- or overcorrection of the defect and contour irregularities; very rarely damage to underlying structures, e.g. implants, pneumothorax, peritonitis and fat embolism, have all been reported infrequently [8, 24, 26, 28].
As a guide, in a large single centre series of 950 lipomodelling procedures (all eligible patients being included) the following complications occurred [8, 19, 29, 39]:
A 0.7% rate of wound infection, with most cases responding to standard oral antibiotic treatment.
A 3% rate of fat necrosis, presenting clinically either as a palpable lump or an area of firmness, which slowly resolved. It should be noted that in some cases, ultrasound examination of fat necrosis can mimic cancer. If any doubt exists and particularly if any increase in size of the necrotic area is noted, a core biopsy should be performed to exclude tumour recurrence.
A 0.1% rate of intraoperative pneumothorax secondary to perforation of the pleura by the transfer cannulas. Multilayer parallel injections, in a tangential direction (avoiding perpendicular trajectories) will prevent such a rare complication.
There were no documented cases of fat embolism or perforation of any intra-abdominal viscus.
20.5.2 Follow-Up
Surgical follow-up. An assessment should be planned for 3 months to evaluate the recipient and donor sites and for planning further staged procedures. Evaluation of midterm outcomes can be made at an interval of 1 year.
Radiological and oncological follow-up should be according to local protocols. However, lipofilling may cause changes on breast imaging. Mammography is best performed before the actual procedure and deferred for at least 6 months postoperatively. The clinician requesting the mammogram must provide adequate information regarding the procedure and site where lipomodelling has been performed so accurate interpretation of imaging changes is possible. Usually an interval of 12–18 months is required before microcalcifications associated with lipofilling become apparent on mammography. An experienced radiologist aware of a past history of lipofilling can usually easily discriminate between the typical resulting benign calcifications and new suspicious microcalcification. Biopsy may however be needed in some cases and patients need to be made aware that this procedure has the potential to subject them to a need for extra interventional procedures and biopsies [9, 10, 41].
20.6 Technique
Joint guidelines developed by the Association of Breast Surgery, the British Association of Plastic, Reconstructive and Aesthetic Surgeons and the British Association of Aesthetic Plastic Surgery emphasize the need for detailed and informed assessment of patients suitability and individual risk factors, to identify those who will benefit from the technique and to minimize the risk of adverse outcomes [16].
It is important to ensure that local governance processes are in place and adhered to when introducing lipomodelling as a new procedure in an institution. Patients should be given preoperative, operative and postoperative information in detail and explanation about short-and long-term complications. It is important that surgeons have received appropriate training in the technique.
20.7 Informed Consent
Informed consent should be in the form of an ongoing agreement with the patient about the treatment and requires a full and detailed explanation of all risks and benefits.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree