EVALUATION OF ERECTILE DYSFUNCTION
Part of “CHAPTER 117 – ERECTILE DYSFUNCTION“
OVERVIEW
The diagnostic testing and treatment options for ED are intimately related. Invasive therapy necessitates greater reliance on diagnostic testing than do benign therapeutic interventions. Consequently, practice conventions have changed radically now that a relatively safe, orally administered medication for treatment of ED is available.
For years, the evaluation and treatment of ED was the purview of specialists. The complexity of the erectile and ejaculatory processes often required evaluation by clinicians from several disciplines. With the introduction of sildenafil, how-ever, most men are seen initially by their primary care physicians. Commonly, empirical treatment ensues, and referral to a specialist is made only after treatment failure. This approach provides treatment to a large number of men at lowest cost, but it shifts efficacy and risk assessments to primary care providers.
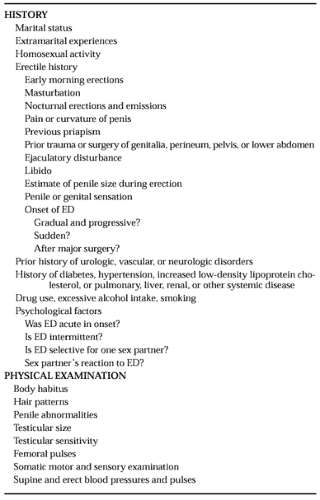
Before any treatment is initiated, the assessment should begin with a careful history-taking and physical examination, recording of the sexual history, and a thorough review of the sexual problem. Use of questionnaires can be particularly helpful for the sexual history-taking and problem documentation. These procedures allow informed determination of (a) the need for treatment, (b) the nature of the dysfunction, (c) the severity of the condition, and (d) the potential contraindications for treatment. Sometimes problems are related to medication side effects, and at other times they may stem directly from relationship issues. If the physician has a high clinical suspicion of a specific pathologic condition (e.g., hypothyroidism), appropriate laboratory testing should be performed. Further diagnostic assessment usually is considered only after the initial treatment challenge fails. Additional diagnostic tests are indicated, as interventions become more invasive.
HISTORY AND PHYSICAL EXAMINATION
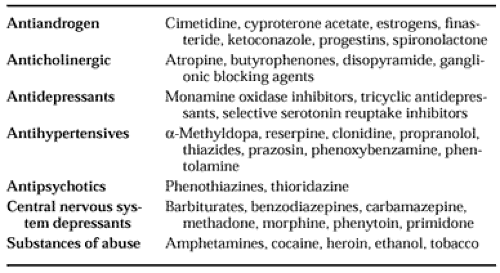
The history-taking and physical examination seek to evaluate the severity of the patient’s erectile problems and determine the cause. Whether the ED is due primarily to organic or psychogenic factors helps direct the therapeutic approach. Aspects of the history and physical examination are outlined in Table 117-1. Use of a short questionnaire may help identify specific sexual complaints. Many drugs that act on the central or autonomic nervous system have been associated with ED29,30 and 31 (Table 117-2); however, most of these drugs have not been tested using objective measures of erectile function. For example, questionnaire studies addressing the effects of the use of selective serotonin reuptake inhibitors in 152 men and 192 women revealed greater delayed orgasm and ED with paroxetine than with fluvoxamine, fluoxetine, and sertraline. Overall, sexual dysfunction correlated with dosage. On the other hand, patients with premature ejaculation benefited from ejaculatory delay and had improved sexual satisfaction.32 This latter result supports the laboratory-demonstrated therapeutic benefit realized by patients with premature ejaculation from the use of clomipramine33,34 and fluoxetine.35 Nonetheless, objective studies of drug-related iatrogenic ED are largely lacking.
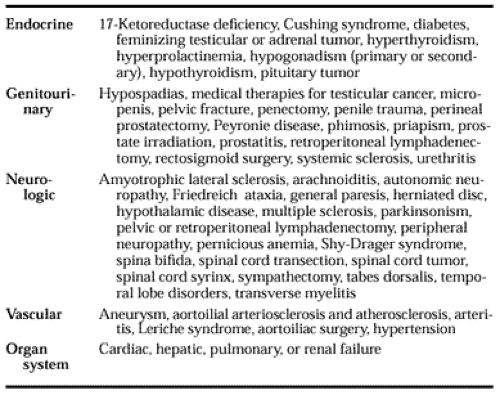
The clinician should consider relevant comorbid factors (Table 117-3). Many endocrine disorders, genitourinary diseases, and neurologic dysfunctions are associated with ED. Importantly, aging per se does not cause ED; however, the incidence of many ED-causing diseases increases as a function of age. In the community-based Massachusetts Male Aging Study, hypertension, diabetes, cigarette smoking, and low levels of
HDL lipoprotein cholesterol increased the risk of ED.2 Cigarette smoking increased the probability of total ED in men with heart disease and hypertension. Increased Lp(a) lipoprotein levels also have been correlated with ED of vascular origin.36
HDL lipoprotein cholesterol increased the risk of ED.2 Cigarette smoking increased the probability of total ED in men with heart disease and hypertension. Increased Lp(a) lipoprotein levels also have been correlated with ED of vascular origin.36
QUESTIONNAIRES
Sexual function inventories and psychometric tests provide valuable clinical information even though they do not reliably differentiate the cause of ED as being organic, psychological, or behavioral. Most specialized clinics assess attitudes toward sex, knowledge about sexual matters, prior sexual experience, self-perception, relationship dynamics, and performance anxiety. Exploring, at least in general, certain psychiatric issues—especially mood, general anxiety, and personality—is also helpful. Several standardized sexual functioning questionnaires are available. Widely recognized sexual history and functioning instruments designed for men include the Florida Sexual History Questionnaire, the Sexual Arousability Inventory, the Sexual Anxiety Inventory, the Pittsburgh Sexual Functioning Inventory, and the Derogatis Sexual Functioning Inventory. Relationship issues can be investigated using the Dyadic Adjustment Scale or the more elaborate Family Adaptability and Cohesion Evaluation Scales III (FACES-III). Commonly used self-administered instruments for assessing mood, anxiety, and personality include the Beck and Zung depression inventories, the Spielberger State-Trait Anxiety Inventory, and the Minnesota Multiphasic Personality Inventory. Alternatively, a psychiatric interview can provide the skilled clinician with comparable information.
The use of information obtained from the questionnaires mentioned previously helps to optimize the treatment plan. However, a positive psychological test finding does not necessarily indicate a psychogenic basis for ED. Distress arising from an organically based intermittent erectile failure is understandable. Performance anxiety is likely to emerge, mood may suffer, and changes in relationship dynamics will follow. Denial, avoidance, projection, guilt, reaction formation, or depression may accompany organic ED. For many men, the development of ED, regardless of its cause, constitutes a crisis. Psychological or behavioral measures reflect this fact.
If ED is primarily psychogenic, evaluating the nature and scope of psychological, relationship, and behavioral disruption can identify problems and suggest appropriate ways to intervene. If the primary mechanism underlying ED is organic, psychometric instruments can identify factors compounding the condition. Moreover, psychological and relationship issues may render physiologically targeted therapies ineffective unless the clinician addresses secondary behavioral factors. Therefore, because psychiatric, relationship, and behavioral influences can predispose to, precipitate, or perpetuate ED, these nonorganic factors must not be overlooked.
LABORATORY AND ENDOCRINE TESTS
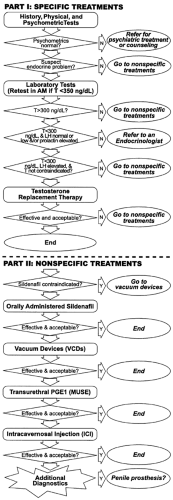
Usually, a complete blood count and screening serum chemistries will detect systemic diseases that can cause ED, and measurement of serum T level can detect androgen deficiency (Fig. 117-2). If the initial T level is <350 ng/dL, early morning serum T, luteinizing hormone, and prolactin levels should be obtained. Because T and prolactin values are higher in the early morning, blood specimens should be collected between 8:00 and 10:00 a.m. The age-related increase in TeBG or sex hormone–binding globulin produces a reduction in non–TeBG-bound T. This is the fraction that is bioactive; therefore, measurement or calculation of non–TeBG-bound T in men who are older than 60 years or have altered levels of TeBG may be useful. (However, commercially available free T assays are influenced by the level of TeBG and often are unreliable.) Thyroid and adrenal disease can cause ED and, if suspected, should be considered in the evaluation.
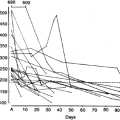
SLEEP-RELATED ERECTION TESTING
SREs were first reported in adults in 1944.37 The association between SREs and REM sleep was established 21 years later, and the term nocturnal penile tumescence (NPT) was coined. Although the function of REM sleep erections is unknown, they have proven useful for assessing erectile capability in men complaining of ED.38 Erectile activity can be measured directly and objectively in terms of increases in penile length, circumference, and volume, duration of erection, and firmness of the penis during erection. Procedures used to measure activity during the initiation and maintenance phases of erection need to be as unobtrusive as possible to minimize alterations in erection produced by the apparatus. Measuring penile length or volume is both difficult and expensive; by contrast, expandable strain gauges provide easily transduced electronic signals that are linearly related to circumference change.39 Other instruments measure penile circumference by measuring lengths of inelastic band encircling the penis.40 Measuring circumference increase is the most common method for indexing the presence and duration of erections.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree